Journal of comprehensive Nursing Research and Care Volume 2 (2017), Article ID: JCNRC-107
https://doi.org/10.33790/jcnrc1100107Research Article
Experiences of Nurses in the Process of Determining a Nursing Diagnosis and Needs for Applying a Nursing Diagnosis: Fostering Understanding to Support the Use of Nursing Diagnoses in Clinical Practice
Yasuko Kume*, Harumi Yamaguchi
Graduate School of Nursing, School of Nursing, Mukogawa Women’s University Hyogo, Japan
Corresponding Author Details: Yasuko Kume, Graduate School of Nursing, School of Nursing, Mukogawa Women’s University, Hyogo, Japan. E-mail: kume@mukogawa-u.ac.jp
Received date: 06th January, 2017
Accepted date: 27th March, 2017
Published date: 31st March, 2017
Citation: Kume, Y., & Yamaguchi, H. (2017). Experiences of Nurses in the Process of Determining a Nursing Diagnosis and Needs for Applying a Nursing Diagnosis: Fostering Understanding to Support the Use of Nursing Diagnoses in Clinical Practice. J Comp Nurs Res Care 2: 107.
Copyright: ©2017, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Purpose: This study illustrates through experiences of nurses while determining nursing diagnoses in terms of thought, behavior, and emotion. It demonstrates current issues in and the needs for support in the use of nursing diagnoses.
Methods: Data were collected through conducting semi-structured interviews based on an interview guide concerning the experiences of nurses and their awareness of issues in the process of determining nursing diagnoses.
Principal Results and Major Conclusions: Followingten categories were selected upon considering the experiences of nurses in determining nursing diagnoses from a thought perspective: [Comparison with defining characteristics], [Confirmation of defining characteristics, related factors, and definition], [Searching for potential nursing diagnoses from main symptoms and problems], [Considering nursing diagnosis from nursing intervention and outcome], [Patterned thinking relating to specific diagnoses], [Considering some temporary nursing diagnoses and monitoring progress], [Identification of multiple nursing diagnoses], [Comparison of some nursing diagnosesby pickingpotential diagnoses of defining characteristics or related factors, definition], [Integrating multiple nursing diagnoses], and [Avoiding nursing diagnosis decisions]. From the behavioral and emotional perspectives, emphasis was placed on [Confirming and reviewing with other staff to determine a diagnosis] and [Solo confirmation and review to decide on a nursing diagnosis]. These were found to be driven by: [Pressure to provide a nursing diagnosis], [Sense of burden over task load that goes with nursing diagnoses], [Anxiety when determining a nursing diagnosis], [Negative emotions towards nursing diagnoses], and [Decline of negative emotions towards nursing diagnoses]. Needs for nursing diagnosis application included [Needs for fostering understanding and learning of nursing diagnosis], [Needs for expanding the process of nursing diagnosis], [Needs for nursing diagnosis and nursing intervention for patients in specific situations], [Needs for the application of an electronic health record system], and [Needs for thinking ability in applying nursing diagnosis], suggesting a need to foster understanding of nursing diagnoses and application of examples.
Introduction
According to the Nursing Diagnosis Association International (NANDA-I), “A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability” (p. 464) [1]. It is also an important tool for keeping records of one’s thought process and practice when practicing nursing.
Seventy-eight percent of office-based physicians used some form of an electronic health record (EHR) system in 2013 [2]. It is reported that the introduction rate for electronic health record systems in Japan is 27.3%, with over 70.1% of hospitals having more than 400 beds [3]. The prevalence of nursing diagnoses and use of an electronic medical recoding system might have the same tendency, indicating that nursing diagnosis is primarily being spread to medical facilities with a large number of beds. Consequently, there have also been studies conducted regarding the difficulties and issues with using nursing diagnoses, highlighting the fact that psychiatric nursing units have few nursing diagnostic labels, insufficient understanding of nursing diagnostic definitions and concepts, and insufficient assessment [4]. Issues concerning the accuracy of diagnoses have also been pointed out in a study of nursing diagnostic ability using mock cases [5]. As issues are s till expected to arise in the application of nursing diagnosis, we considered it necessary to investigate what nurses experience in the process of determining nursing diagnoses, what is lacking in order to apply nursing diagnosis in practice, what difficulties exist, and what needs exist.
Purpose
This study explored the experiences of nurses in the process of determining nursing diagnoses in terms of thought, behavior, and emotion. It also examined the needs for the use of nursing diagnoses and considered current issues and a support system for making improvements based on these needs.
Methods of Data Collection and Analysis
Since this study focuses on interpreting the experiences of nurses by focusing on learning and reflection based on experience from the characteristics of nursing practices, it explored these experiences from the three perspectives of thought, behavior, and emotion under the Action and Looking back on the action and Awareness of essential aspects and Creating alternative methods of action, and Trial (ALACT) model proposed by Korthagen [6]. The meanings of thoughts, behaviors, and emotions were explored in the following manner. The thought perspective signifies what nurses were thinking during the process of determining a nursing diagnosis. The behavioral perspective signifies what actions the nurses actually took during this process. Finally, the emotional perspective signifies what the nurses felt during this process. In addition, needs required for applying nursing diagnosis refers to that which is recognized as lacking and as being difficult in the process of determining nursing diagnoses, as well as that which needs to be fulfilled.
Participating this study were 13 female nurses who work at Hospital A and agreed to participate in this study. Five of these nurses work in the internal medicine ward, two of them work in the surgical ward, and six of them work in the mixed medical ward. Hospital A is a general hospital with 499 beds in the Kansai region of Japan. Years of clinical experience among the participants varied from two years to 18 years with an average of 9.2±5.8 years. Data were collected by conducting semi-structured interviews based on an interview guide concerning the experiences of nurses and their awareness of issues in the process of determining nursing diagnoses. Data analysis was performed using a content analysis method [7], and records of the interviews were prepared. The whole of the transcript from the nurses’ testimony was considered for context, and details of their testimony were noted. Individual details of the notes were summarized and expressions indicating important details within that text were sampled along with tendencies in thought, behavior, emotion, and awareness of problems. Categorization was also done based on similarities and integrated into both categories and subcategories. The reliability of the analysis was also verified between three researchers to ensure the process of analysis remained faithful to the data contents. Collection of data was conducted from March to September of 2015.
Ethical Considerations
The primary aim of the study, the voluntary nature of participation, and strict observance of anonymity were explained to the participants of the study, and interviews were conducted once consent was given. A private room was prepared for conducting interviews, and interviews were generally done once within 30 minutes to an hour time and location were adjusted according to the interviewee’s convenience. Approval was obtained from the Ethics Committee of Mukogawa Women’s University and from the institution that conducted the interviews.
Results
1. Experiences of nurses in the process for determining nursing diagnosis.
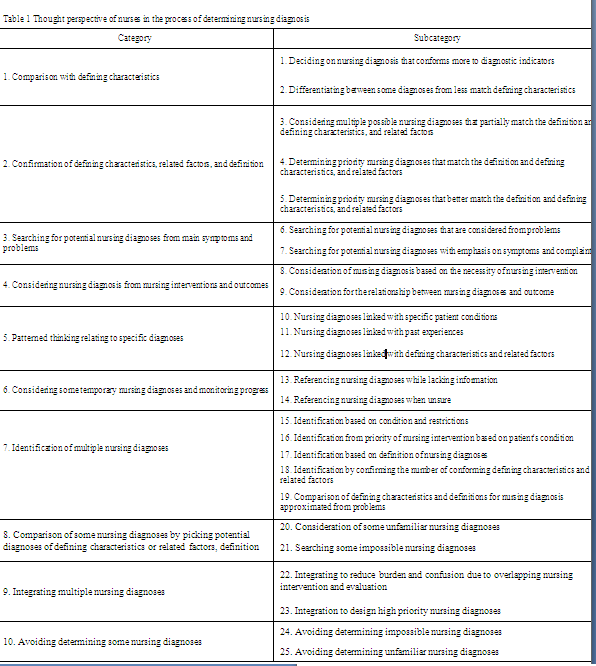
Thought perspective of nurses in the process of determining a nursing diagnosis (refer to Table 1).
Ten categories were selected from the thought perspective of nurses in the process of determining nursing diagnoses. They include [Comparison with defining characteristics], [Confirmation of defining characteristics, related factors, and definition], [Searching for potential nursing diagnoses from main symptoms and problems], [Considering nursing diagnosis from nursing interventions and outcomes], [Patterned thinking relating to specific diagnoses], [Considering some temporary nursing diagnoses and monitoring progress], [Identification of multiple nursing diagnoses], [Comparison of some nursing diagnoses by picking potential diagnoses of defining characteristics or related factors, definition],[Integrating multiple nursing diagnoses], and [Avoiding determining some nursing diagnoses These consist of a further 25 sub-categories.
[Comparison with defining characteristics] consists of two
sub-categories, including
[Considering nursing diagnosis from nursing intervention and
outcome] consists of the subcategory
[Patterned thinking relating to specific diagnoses] has several
categories, including
[Planning a temporary nursing diagnosis and watching the
progress] consists of the two subcategories
[Integrating multiple nursing diagnoses] consists of the two
subcategories
Subcategories for [Avoiding determining some nursing diagnoses]
include
Behavioral perspective of nurses in the process of determining a nursing diagnosis
The three categories of [Confirming and reviewing with other staff when determining a diagnosis], [Solo confirmation and review to determine a nursing diagnosis], and [Taking action without confirming] were selected from the behavioral perspective of nursing in the process of determining a nursing diagnosis and consisted of a further 11 subcategories.
The category [Confirming and reviewing with other staff when
determining a nursing diagnosis] includes subcategories such as
[Confirming and reviewing with other staff to decide on a diagnosis]
consists of the categories
Other subcategories include
[Taking action without confirming] consists of the three subcategories
Emotional perspective of nurses in the process of determining a nursing diagnosis
The five categories of [Pressure to do a nursing diagnosis], [Sense of burden for task load that goes with nursing diagnosis], [Anxiety when determining a nursing diagnosis], [Negative emotions towards nursing diagnosis], and [Decline of negative emotions towards nursing diagnosis] were selected for the emotional perspective of nursing in the process of determining a nursing diagnosis, with a further 11 subcategories.
[Pressure to do a nursing diagnosis] includes the subcategories
[Sense of burden for task load that goes with nursing diagnosis]
includes the subcategories
[Anxiety when determining a nursing diagnosis] consists of
two subcategories. One is
[Negative emotions towards nursing diagnosis] derives from
subcategories such as
[Decline of negative emotions towards nursing diagnosis] is made
up of three subcategories.
Needs for the use of nursing diagnoses
Needs for the application of nursing diagnosis include the seven categories of [Needs for fostering understanding and learning of nursing diagnosis], [Needs for expanding the process of nursing diagnosis], [Needs for nursing diagnosis and nursing intervention for patients in specific situations], [Needs for the application of an electronic health record system], [Needs for nursing diagnosis in situations with insufficient patient information], [Needs for thinking ability in applying nursing diagnosis], and [Needs for sharing of information among staff], consisting of a further 22 subcategories.
[Needs for fostering understanding and learning of nursing
diagnosis] includes five subcategories relating to viewpoints and
methods to help understand nursing diagnoses. This includes
[Needs for nursing diagnosis and nursing intervention for patients in
specific situations] contains three subcategories.
[Needs for the use of an electronic health record system] consists of
four subcategories.
[Needs for thinking ability in applying nursing diagnosis] includes
the two subcategories
Discussion
Issues with the process for determining a nursing diagnosis from a thought perspective, and support to improve them
It was demonstrated that a trait in the thought perspective in the general process of determining a nursing diagnosis is the tendency to focus on main symptoms, problems, nursing intervention, or outcome to give a candidate for nursing diagnosis that is then compared to the defining characteristics.
Another characteristic trend in the way nurses think was their patterned thinking for specific nursing diagnoses. Nurses who practice clinical nursing daily in particular will develop a pattern from their repeated experiences with similar situations of patient care, and there also seems to be an unwritten rule appearing within wards where a nursing diagnosis is made by combining these experiences with defining characteristics and related factors. Benner et al. explain that when grasping a patient’s condition and providing support, experienced nurses provide pattern recognition, recognition of similarities, common understanding, proficient and practical knowledge, the ability to notice important points, and a rationale gained through experience [8]. This thinking pattern in the process of determining a nursing diagnosis is thought to be connected with their ability, cultivated through experience, to recognize similarities and perceive important points. Thus, we consider the increasing focus on intuitive nursing diagnosis during a nurse’s experiences and find that it is an effective way of thinking in terms of making effective progress for nursing diagnoses. On the other hand, patterned thinking is uniform and not analytical, and thus can potentially lead to insufficient support for individual cases and insufficient review of the information of individual patients. Bearing these disadvantages in mind, however, it is essential that intuitive judgment continues to be applied.
Another trend that has been demonstrated for clinical settings is the sense of burden that accompanies giving too many nursing diagnoses, as well as the tendency to integrate nursing diagnoses when nursing intervention overlaps. This integration also takes into consideration the importance of nursing intervention and the outcome that the patient requires. It is thought that the anxiety and sense of burden when making a nursing diagnosis is reduced once clinical nurses have an indicator or hint concerning the thought processes for this integration.
Issues with the decision-making process for nursing diagnosis from an emotional and thought perspective, and support to improve them
The results indicate that nurses experienced pressure to provide a nursing diagnosis. It was pointed out in a Korean study that some nurses complained that using standardized nursing languages, such as the NANDA-I, was a burden, as they do not have enough time. This study suggested it would take extra time to write nursing documentation if they do not have enough knowledge about SNLs [9]. Ofi and Sowunmi said that lack of time and knowledge, and the need for extensive writing are the major barriers against documentation [10]. Nurses felt there was a lack of education for nursing diagnoses and recognized its necessity, and also felt anxiety when making a diagnosis. This suggested that the knowledge of nursing diagnoses and time for documentation influenced feelings of being burdened.
For that reason, they did not make independent decisions for nursing diagnoses and regularly carried out multiple forms of verification through conferences and consultation. This emphasis on determining nursing diagnoses through confirmation and agreement with groups shows that the unwritten rules in all wards are easily influenced when reviewing nursing diagnoses in groups, and is assumed to also influence patterned thinking. While it was indicated that conferences are effective for a nurse’s state of mind, further confirmation of their effect in terms of validity and accuracy will be required.
Needs for the use of nursing diagnoses and support measures
Nurses brought up the need for fostering understanding of nursing diagnosis terminology and called for explanation and discussion using specific examples. Clinical nurses recognize the issue with understanding defining characteristics and definitions and sought methods that convey terminology more easily
“Needs for the use of an electronic health record system” also came up, which in turn suggests the need to provide support in utilizing the electronic health record system. Meiβner and Schnepp point out that the quality of records can help improve the quality of care, and state that the time needed to complete electronic health records depends on effective use of IT [11]. In addition, the two argues that in addition to the attitude of the nurses, ease of use and ability to use IT and equipment availability and technical functionality also affects the effective use of IT. As regards to the emotional perspective of the nurses, the sense of burden in completing and recording nursing diagnosis was mentioned. This suggests that there is a need to provide both user support and physical support, can help improve the quality of care, and state that the time needed to complete electronic health records depends on effective use of IT [11]. In addition, the two argues that in addition to the attitude of the nurses, ease of use and ability to use IT and equipment availability and technical functionality also affects the effective use of IT. As regards to the emotional perspective of the nurses, the sense of burden in completing and recording nursing diagnosis was mentioned. This suggests that there is a need to provide both user support and physical support, et al. suggested the following four factors based on a systematic literature review: the nurse as a diagnostician, diagnostic education and resources, complexity of a patient’s situation, and hospital policy and environment [12]. Considering previous study results such as above and the results of this research, we can argue that in order to make effective use of nursing diagnosis, it is crucial to clarify the policies within the nursing section of hospitals, and to provide educational support and environment for lack of learning. The NANDA-I explains the need for leaders in the nursing industry and nursing information specialists to work together to introduce an inspection system that can verify the accuracy of nursing diagnoses by using defining characteristics obtained from patient assessments and related/risk factors. Future cooperation with nursing information specialists will be needed to advance the application of nursing diagnosis.
Limitations
Since the participants of this study were nurses from a portion of one facility in Japan, the findings may have been influenced by the characteristics of said facility’s department and the education background of its nurses. However, the facility is a mid-scale hospital that is unique for having around 500 beds and is thought to be representative of the characteristics of nurses working in Japan. Increasing the number of regions and facilities and further investigating whether similar situations exist will need to be attempted.
Conclusions
Ten categories were selected upon viewing the experiences of nurses in determining nursing diagnoses from a thought perspective. These categories are [Comparison with defining characteristics], [Confirmation of defining characteristics, related factors, and definition], [Searching for nursing diagnosis candidates from main symptoms and problems], [Considering nursing diagnosis from nursing intervention and outcome], [Patterned thinking relating to specific diagnoses], [Considering some temporary nursing diagnoses and monitoring progress], [Identification of multiple nursing diagnoses], [Comparison of some nursing diagnoses by picking potential diagnoses of defining characteristics or related factors, definition], [Integrating multiple nursing diagnoses], and [Avoiding determining some nursing diagnoses]. These categories revealed that there is no general nursing diagnosis process, and nurses will search for nursing diagnoses from main symptoms and nursing intervention or have a patterned thought process. From the behavioral and emotion perspectives, emphasis was placed on [Confirming and reviewing with other staff to determine a diagnosis] and [Solo confirmation and review to decide on a nursing diagnosis]. These were indicated to be driven by the following: [Pressure to do a nursing diagnosis], [Sense of burden for task load that goes with nursing diagnoses], [Anxiety when determining a nursing diagnosis], [Negative emotions towards nursing diagnoses], and [Decline of negative emotions towards nursing diagnoses].
Conflict of Interest
The authors declare that they have no competing interests.
Acknowledgments
We extend our thanks to all the participants in this study. This work was supported by JSPS KAKENHI Grant Number 15K11537. The authors declare no conflict of interest associated with this manuscript.
References
Herdman, T., & Kamitsuru, S., (2014). From assessment to diagnosis. In: T Herdman & S Kamitsuru (Eds.), NANDA International Nursing Diagnoses: Definitions and Classification 2015-2017 (10th ed.) p. 464. Wiley Blackwell, Oxford.View
Hsiao, C.J., & Hing, E. (2012). Use and characteristics of electronic health record systems among office-based physician practices: United states, 2001-2012. NCHS Data Brief 1-8.View
Japanese Association of Healthcare Information Systems Industry (2016). Report on situation of introduction of ordering and electronic health record systems in hospitals. 1-2.
Shiraishi, S., Fujiki, M., Takemasa, N., Hosako, K., & Yatabe. K., et al. (2015). Seishin kangoryouiki ni okeru kangoshindandonyuu nikansuru zenkoku jittaichousa [National wide survey of introducing nursing diagnosis in psychiatric nursing units]. J Japan Soc Nurs Diagn 20: 4-13.
Hasegawa, T., Ogasawara, C., & Katz, E.C. (2007). Measuring diagnostic competency and the analysis of factors influencing competency using written case studies. Int J Nurs Know 18: 93-102.View
Korthagen, F.A.J. (1999). Linking reflection and technical competence: The logbook as an instrument in teacher education. E Euro J Teacher Edu 22: 191-207.View
Graneheim, U.H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurs Edu Today 24: 105-112.View
Benner, P., Tanner, C. (1987). Clinical judgment: How expert nurses use intuition. Am J Nurs 87: 23-31.View
Park, H., & Lee, E. (2015). Incorporating Standardized Nursing Languages In to an Electronic Nursing Documentation System in Korea: A Pilot Study. Int J Nurs Knowl 26: 35-42.View
Ofi, B., & Sowunmi, O. (2012). Nursing documentation: Experience of the use of the nursing process model in selected hospitals in Ibadan, Oyo State, Nigeria. Int J Nurs Pract 18: 354-362.View
Meiβner, A., & Schnepp, W. (2014). Staff experiences within the implementation of computer-based nursing records in residential aged care facilities: a systematic review and synthesis of qualitative research. BMC Medical Informatics and Decision Making.View
Paans, W., Nieweg, R.M., van der Schans, C.P., & Sermeus, W. (2011). What factors influence the prevalence and accuracy of nursing diagnoses documentation in clinical practice? A systematic literature review. J Clin Nurs 20: 2386-2403.View