Journal of Comprehensive Nursing Research and Care Volume 9 (2024), Article ID: JCNRC-206
https://doi.org/10.33790/jcnrc1100207Research Article
Interaction of Physical Activity and Respiratory Function on Mental Health in Older Adults
Makoto Suzuki1*, Nobuyuki Honda2, and Akane Katsuda1
1Department of Occupational Therapy, Faculty of Health Sciences, Bukkyo University, Kyoto, Japan.
22Department of Rehabilitation Sciences, Faculty of Allied Health Sciences, Kansai University of Welfare Sciences, Kashiwara, Japan.
Corresponding Author Details: Makoto Suzuki, Department of Occupational Therapy, Faculty of Health Sciences, Bukkyo University, Kyoto, Japan.
Received date: 13th November, 2024
Accepted date: 19th December, 2024
Published date: 21st December, 2024
Citation: Suzuki, M., Honda, N., & Katsuda, A., (2024). Interaction of Physical Activity and Respiratory Function on Mental Health in Older Adults. J Comp Nurs Res Care 9(2): 207.
Copyright: ©2024, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
This study explored the interaction between physical activity, respiratory function, and mental health among older adults using data from the English Longitudinal Study of Aging. Specifically, the effects of physical activity and respiratory function indicators, including percent vital capacity and the ratio of Forced Expiratory Volume in One Second to Forced Vital Capacity, on depressive symptoms and life satisfaction were analyzed using structural equation modeling, with adjustments for selection bias via inverse probability weighting. A longitudinal cohort design was employed, involving 1,519 participants aged 65 years or older, with data from waves 2 and 6. The results indicated a significant negative association between physical activity and depressive symptoms, suggesting the potential benefits of physical activity in alleviating mental health issues. However, while respiratory function measures had a limited impact on depressive symptoms, adding error covariances between respiratory indicators improved the model fit, highlighting their potential relevance to mental health research. The clinical implications of these findings suggest that physical activity combined with respiratory rehabilitation may be beneficial in older adults. Future research should focus on causal mechanisms, confounding factor adjustments, and comparative studies across cultural contexts to broaden the generalizability.
Keywords: Physical Activity, Respiratory Function, Mental Health, Depressive Symptoms, Life Satisfaction, Older Adults, SEM, IPW
Introduction
As global aging progresses, maintaining health and improving the quality of life among older adults have become essential challenges. Physical activity and respiratory function are crucial for maintaining physical and mental health [1-5]. Physical activity is associated with life satisfaction and depressive symptoms [6,8], whereas a decline in respiratory function may lead to physical decline and psychological stress [9,11]. Maintaining these factors is essential for effective interventions aimed at promoting older adults’ health.
The positive impact of physical activity on mental health is widely acknowledged. Older adults who engage in regular exercise tend to experience reduced levels of depressive symptoms [12,13]. Moreover, maintaining respiratory function plays an important role in health, and indicators, such as percent vital capacity (VC%) and forced expiratory volume in one second over forced vital capacity (FEV1/FVC) are noted as health markers [14,15]. However, there is limited research on how these factors interact to influence mental health and life satisfaction.
Previous research has clarified the individual effects of physical activity and respiratory function. However, there are still many unresolved aspects regarding how their interaction affects mental health and life satisfaction. Suzuki (2024) suggests that physical activity may contribute to the maintenance of respiratory function. However, few longitudinal studies have examined the effects of respiratory function on the relationship between physical activity and depressive symptoms. A multivariate analysis is necessary to comprehensively analyze these factors and clarify the causal relationships that include temporal changes.
This study aimed to elucidate the effects of physical activity and respiratory function on depressive symptoms and life satisfaction, using data from the English Longitudinal Study of Ageing (ELSA). The indicators included VC% and FEV1/FVC ratio, which were examined for their moderating effects on the relationship between physical activity and mental health. Structural equation modeling (SEM) is used to analyze both direct and indirect effects among the variables, while inverse probability weighting (IPW) is used to adjust for selection bias. This study aimed to comprehensively understand the impact of the interactions between physical activity and respiratory function on mental health, contributing to evidencebased interventions to support older adults.
Materials and Methods
Study Design
This longitudinal cohort study used data from waves 2 and 6 of the ELSA, which analyzed the effects of physical activity and respiratory function on the mental health of older adults. The ELSA is a nationwide longitudinal survey targeting older adults in the United Kingdom that provides detailed information on physical and mental health, social factors, and life satisfaction [16]. This study focused on mental health, physical activity, respiratory function, and life satisfaction and analyzed the relationships among these variables using SEM.
Application of Inverse Probability Weighting (IPW)
IPW was applied to adjust for selection bias and the influence of missing data, resulting in reliable estimates that more accurately reflected the general population. IPW is used to reduce bias when data are missing, but are not missing at random, by weighting each sample based on the probability of selection in the observed data. In this study, propensity scores were estimated, and the inverse of these scores was used as a weight to adjust for the effects of missing data and selection bias. This approach minimized the impact of selection bias and provided reliable estimates [14].
Participants
The participants were limited to those aged 65 years and older at wave 2, with complete data on the main variables (physical activity, respiratory function, depressive symptoms, and life satisfaction) at both waves (wave 2 and wave 6). All samples with missing values were excluded, resulting in a final sample size of 1,519 individuals aged 65 years and older. Selection bias was adjusted, and analyses were conducted based on a more representative sample.
Measurement Items
The Center for Epidemiologic Studies Depression Scale (CES-D) was used to assess mental health. The CES-D is a standard scale for evaluating depressive symptoms using the total score of responses to each question item [17]. Life satisfaction was evaluated using the total life satisfaction score in wave 6. Physical activity was measured based on the exercise frequency collected in wave 6, and weekly physical activity levels were evaluated. Indicators of respiratory function included VC% and FEV1/FVC. These respiratory indicators are essential markers of physical health in older adults.
Data Preprocessing
To improve the data quality, samples with missing values were excluded, and only participants aged 65 years or older were extracted. Negative FVC and FEV values were considered as missing. IPW was applied and propensity scores were estimated and weighted based on these scores. Using IPW, the samples used for analysis were adjusted to be more representative of the entire population, thereby enhancing the reliability of the results.
Model Construction
SEM was used to examine the causal relationships between physical activity, respiratory function, life satisfaction, depressive symptoms and their interactions. First, a simple model without error covariances was constructed, hypothesizing that physical activity directly affects depressive symptoms and life satisfaction, and included both VC% and FEV1/FVC to investigate the association between respiratory function and mental health.
Error covariances were then added based on the modification indices to improve the model fit. Considering the high values in the modification indices, error covariances were introduced between “VC% (wave 6)” and “FEV1.0% (wave 6).” The addition of these error covariances is crucial for the model to better represent variability in real-world data. In particular, when multiple measurement items are related to common measurement errors or potential external factors, adding error covariances enhances measurement accuracy and significantly improves model fit. Following these modifications, the fit indices met the standard values, confirming that the model is suitable for the data.
Statistical Analysis
SEM was performed using the lavaan package in R (4.2.3 Windows). Model fit was evaluated using the comparative fit index (CFI), Tucker–Lewis index (TLI), and root mean square error of approximation (RMSEA). The effectiveness of the model improvement was verified by introducing error covariances based on modification indices. All waves of the ELSA received ethical approval from the National Research Ethics Committee, and informed consent was obtained from all participants.
Results
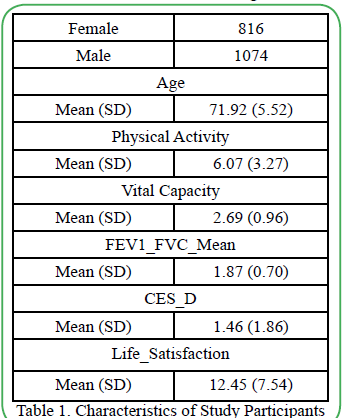
The initial sample size in this study was 4,331. After excluding 77 samples with missing values, 4,254 individuals remained. Of these, participants aged 65 years and above in wave 2 were extracted, resulting in a final analytical sample of 1,890 individuals (Table 1).
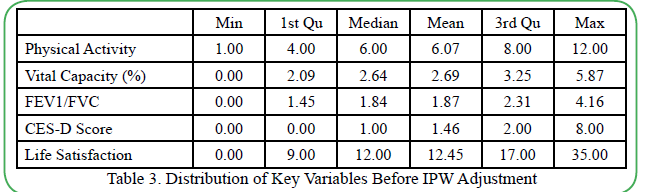
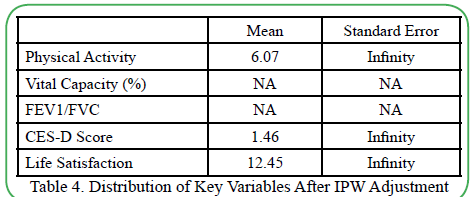
Analysis of the correlations among variables revealed various correlations between physical activity, respiratory function, depressive symptoms, and life satisfaction (Table 2). Detailed analyses of the relationships between these factors were conducted based on these correlations. Examination of the distribution before and after IPW application confirmed that the distribution of major variables became more consistent after the application (Tables 3 and 4).
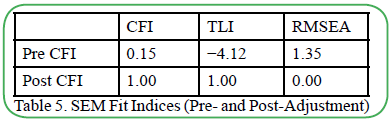
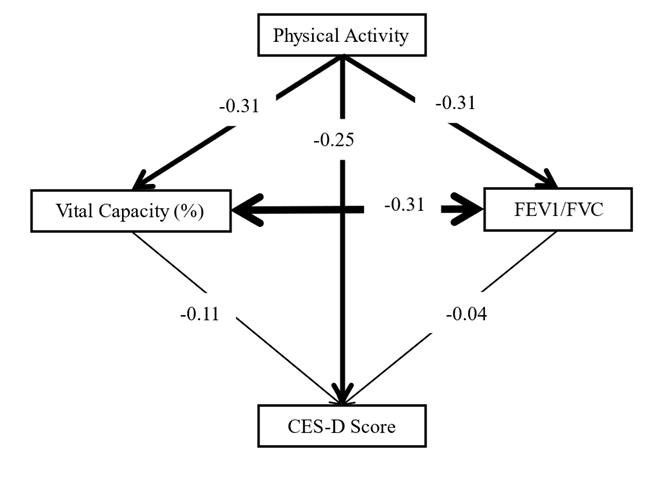
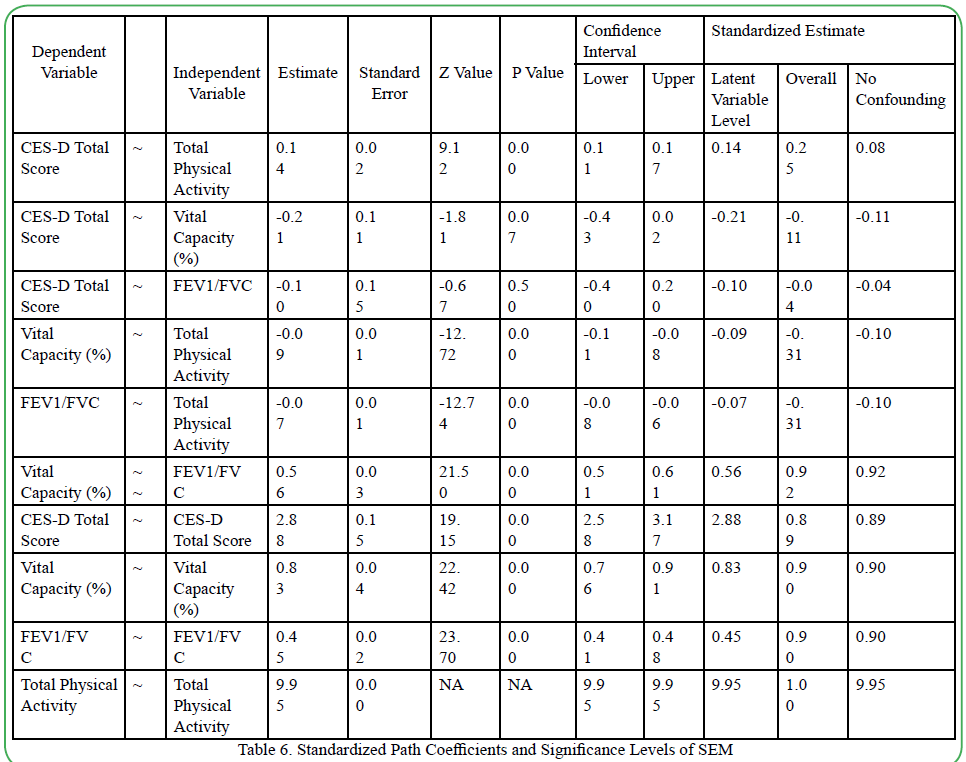
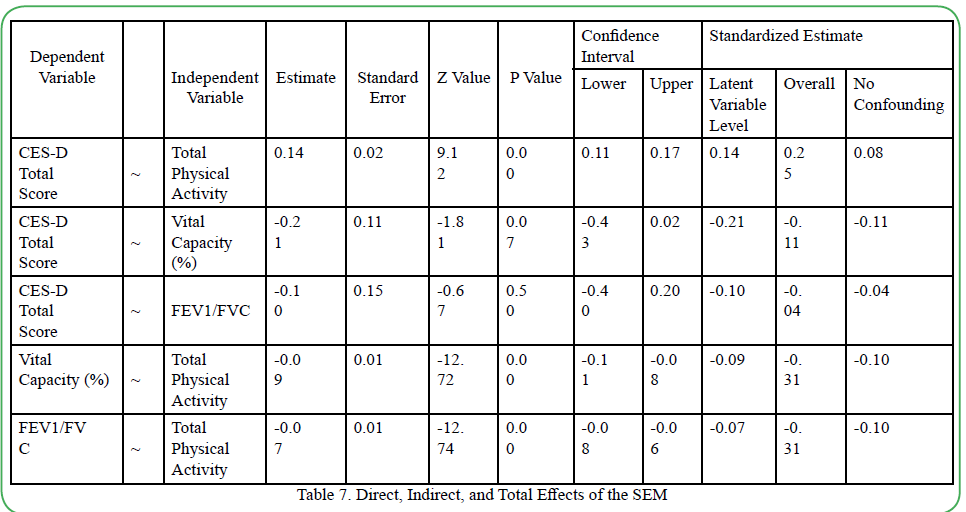
First, analysis of the SEM model without error covariances indicated that physical activity had a significant negative effect on CES-D scores (depressive symptoms) (β = 0.149, p < 0.001). VC% showed a slight potential negative impact on depressive symptoms; however, it was not statistically significant, making it difficult to conclude that improved respiratory function contributes to reducing depressive symptoms (β = −0.184, p = 0.103). Meanwhile, the effect of FEV1/FVC was not statistically significant (β = 0.072, p = 0.623), and its association with depressive symptoms was not confirmed. The fit indices for this model without error covariances indicated an insufficient fit, with CFI = 0.15 and RMSEA = 1.35 (Table 5).
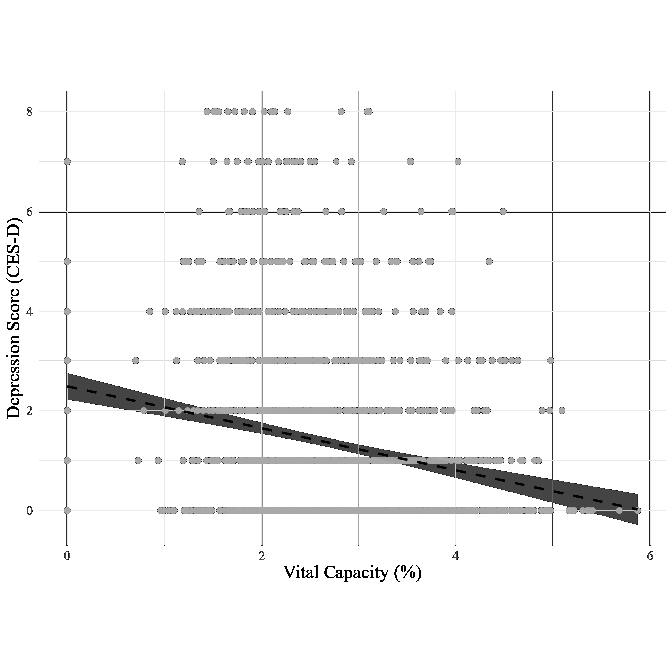
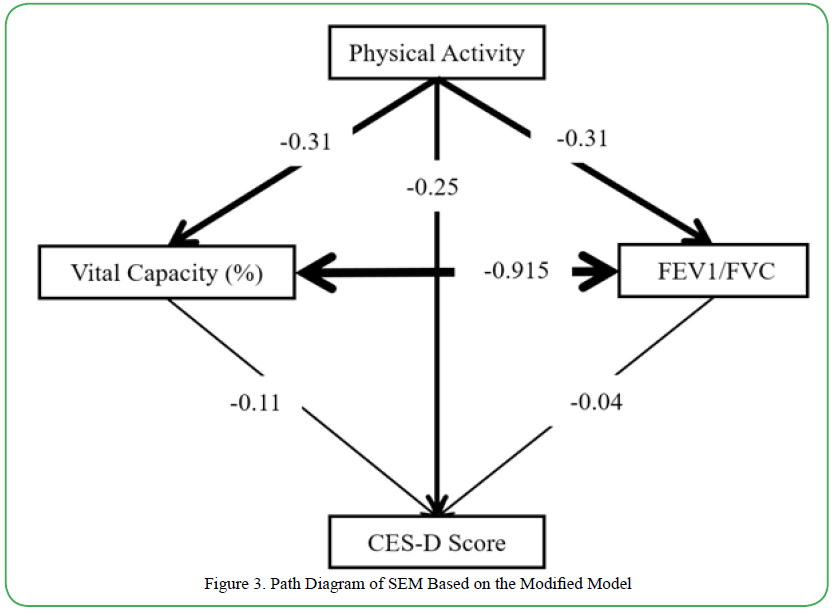
Next, a model was constructed with added error covariances between VC% and FEV1/FVC based on modification indices to improve the fit. The path coefficients for this model after introducing the modification indices are presented (Figure 1 and Table 6). This modification greatly improved the fit, with a CFI of 0.950 and RMSEA of 0.051, indicating that the revised model fit the data well (Table 7). In this modified model, physical activity continued to show a significant effect on CES-D scores (β = 0.149, p < 0.001), suggesting a potential contribution to improved mental health. However, the effects of VC% and the FEV1/FVC ratio on depressive symptoms remained insignificant, with no association between respiratory function and depressive symptoms (Figure 2). Nonetheless, the significant improvement in model fit indicates that introducing error covariances provides a more reliable representation of the relationships among the variables (Figure 3).
Discussion
We conducted a longitudinal analysis of the effects of physical activity, respiratory function, and life satisfaction on depressive symptoms among older adults. A more refined model was constructed by considering the error covariances between the respiratory function indicators. These findings suggest that physical activity may alleviate depressive symptoms, consistent with previous research showing that physical activity promotes mental health through increased endorphin and serotonin secretion [18-22]. However, given that the sample size was limited to 1,519 participants, cautious interpretation of the results is necessary. Additionally, the design of this study confirmed associations, but not causation. The application of causal inference methods, such as randomized controlled trials (RCT) or instrumental variable (IV) analysis is essential for clarifying causal relationships. Future research should consider RCTs with randomized assignment of interventions or IV methods using differences in living environments as instruments to verify causality. Furthermore, the type and frequency of physical activity that impact depressive symptoms in older adults require detailed investigation.
This study also discusses the theoretical basis for model improvement through the addition of error covariance. By adding error covariances between VC% and FEV1/FVC, the model fit was significantly improved (CFI = 1.000, RMSEA = 0.000). This improvement suggests that VC% and FEV1/FVC ratio may be affected by shared measurement errors or latent external factors. The correlation between respiratory function indicators is likely because some indicators are physiologically related to others; however, the extent to which these factors influence depressive symptoms remains unclear. Therefore, integrating multiple respiratory function indicators may allow for a more comprehensive analysis of their impact on depressive symptoms. Future studies should explore the influence of physiological characteristics and measurement errors on respiratory indicators using multiple indicators to clarify the mechanisms affecting mental health.
Furthermore, we discuss the clinical implications and potential applications of these findings. These results suggest that physical activity may contribute to alleviating depressive symptoms in older adults, although improvements in respiratory function did not show a clear effect on depressive symptoms. Physical activity not only benefits mental health, but may also reduce feelings of loneliness and promote social interactions. The recommended interventions include walking, light exercise, and yoga or Pilates programs suitable for older adults. Additionally, respiratory rehabilitation aimed at increasing lung capacity may reduce the activity limitations resulting from declining respiratory function. In particular, an approach that combines respiratory rehabilitation and physical activity tailored to an individual’s living environment and health status is considered effective. Future clinical applications are expected to support the maintenance of mental and physical health among older adults through multifaceted interventions.
In contrast, the model with added error covariances showed an exceptionally high fit, which may suggest a risk of overfitting [23-27]. The fit indices, with a CFI of 0.950 and RMSEA of 0.051, indicated the need to cautiously consider generalizability to realworld data. If overfitting occurs, generalization to new data becomes challenging; therefore, it is important to use cross-validation by splitting the data into multiple parts to reduce the risk of overfitting. Future studies should verify these results using other datasets to strengthen the generalizability of the model.
Adjustment for confounding factors was also necessary. Although this study identified relationships between physical activity, depressive symptoms, and respiratory function, potential confounding factors, including chronic illness, economic status, and family relationships, may not have been fully adjusted for [28]. Future studies should adjust for these confounding factors to obtain a more precise evaluation of these relationships. Moreover, investigating the combined effects of various factors on mental health may enhance the reliability of interpretation.
Finally, this study was based on data from older adults in the United Kingdom, which limits the generalizability of the results. Comparative studies focusing on older adults with different healthcare systems and social backgrounds are needed to determine whether similar relationships exist in other countries and cultural contexts [29-32]. Future studies should also examine how differences in the cultural background, lifestyle habits, and social support impact physical activity and depressive symptoms to improve generalizability. Studies using data from other countries would help clarify the extent to which these findings are applicable to diverse populations.
In conclusion, this study suggests that promoting physical activity may contribute to the alleviation of depressive symptoms in older adults, although improvements in respiratory function did not show a clear effect on depressive symptoms. The potential clinical relevance of combined physical activity and respiratory rehabilitation interventions is highlighted. Future research should investigate causality, adjust for confounding factors, and conduct comparative studies across different cultural contexts to develop more comprehensive and generalizable results.
Conclusion
This study longitudinally examined the impact of physical activity and respiratory function on depressive symptoms in older adults and demonstrated that considering the error covariance of multiple respiratory indicators can enhance the accuracy of respiratory function assessments. These findings suggest that promoting physical activity may reduce depressive symptoms. Clinically, interventions combining physical activity with respiratory rehabilitation are indicated. Future research is expected to yield more comprehensive and generalizable insights through the verification of causal relationships, adjustments for confounding factors, and comparative studies across different cultural contexts.
Conflict of Interest
The authors declare that they have no personal, commercial, political, academic, or financial conflicts of interest related to the content of this submission.
References
Sofi, F., Valecchi, D., Bacci, D., Abbate, R., Gensini, G. F., Casini, A., & Macchi, C. (2011). Physical activity and risk of cognitive decline: A meta-analysis of prospective studies. Journal of Internal Medicine, 269(1), 107-117. View
Laurin, D., Verreault, R., Lindsay, J., MacPherson, K., & Rockwood, K. (2001). Physical activity and risk of cognitive impairment and dementia in elderly persons. Archives of Neurology, 58(3), 498-504. View
Ito, K., Kawayama, T., Shoji, Y., Fukushima, N., Matsunaga, K., Edakuni, N., ... Hoshino, T. (2012). Depression, but not sleep disorder, is an independent factor affecting exacerbations and hospitalization in patients with chronic obstructive pulmonary disease. Respirology, 17(6), 940-949. View
de Voogd, J. N., Wempe, J. B., Koëter, G. H., Postema, K., van Sonderen, E., Ranchor, A. V., & Sanderman, R. (2009). Chest, 135*(3), 619-625. View
Eisner, M. D., Blanc, P. D., Yelin, E. H., Katz, P. P., Sanchez, G., Iribarren, C., & Omachi, T. A. (2010). Influence of anxiety on health outcomes in COPD. Thorax, 65(3), 229-234. View
Sylvester, B. D., Mack, D. E., Busseri, M. A., Wilson, P. M., & Beauchamp, M. R. (2012). Health-enhancing physical activity, psychological needs satisfaction, and well-being: Is it how often, how long, or how much effort that matters? Mental Health and Physical Activity, 5(2), 141-147. View
Bize, R., Johnson, J. A., & Plotnikoff, R. C. (2007). Physical activity level and health-related quality of life in the general adult population: A systematic review. Preventive Medicine, 45(6), 401-415. View
Wilhelmson, K., Fritzell, E., Eklund, K., & Dahlin-Ivanoff, S. (2013). Life satisfaction and frailty among older adults. Health Psychology Research, 1(3), e32. View
Herridge, M. S., Tansey, C. M., Matté, A., Tomlinson, G., Diaz-Granados, N., Cooper, A., ... Canadian Critical Care Trials Group. (2011). Functional disability 5 years after acute respiratory distress syndrome. The New England Journal of Medicine, 364(14), 1293-1304. View
Giltay, E. J., Nissinen, A., Giampaoli, S., Zitman, F. G., & Kromhout, D. (2010). Low respiratory function increases the risk of depressive symptoms in later life in men. Psychosomatic Medicine, 72(1), 53-60. View
Sun, Y., Zhang, Y., Bai, W., & Liu, X. (2023). Relationship between depression severity and respiratory symptoms in US adults: A national cross-sectional study. Respiratory Medicine, 220, 107451. View
Fox, K. R. (2007). The influence of physical activity on mental well-being. Public Health Nutrition, 2(3a), 411-418. View
Hassmén, P., Koivula, N., & Uutela, A. (2000). Physical exercise and psychological well-being: A population study in Finland. Preventive Medicine, 30(1), 17-25. View
Suzuki, M., & Ikeda, T. (2024). Longitudinal relationship between physical activity levels and respiratory function in older individuals: A longitudinal study. Journal of Comprehensive Nursing Research and Care, 9(2), 202. View
Derom, E., van Weel, C., Liistro, G., Buffels, J., Schermer, T., Lammers, E., ... Decramer, M. (2008). Primary care spirometry. European Respiratory Journal, 31(1), 197-203. View
Steptoe, A., Breeze, E., Banks, J., & Nazroo, J. (2013). Cohort profile: The English Longitudinal Study of Ageing. International Journal of Epidemiology, 42(6), 1640–1648. View
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. View
Dinas, P. C., Koutedakis, Y., & Flouris, A. D. (2011). Effects of exercise and physical activity on depression. Irish Journal of Medical Science, 180(2), 319-325. View
Sieniawska, D., Sieniawska, J., & Proszowska, P. (2024). The impact of physical activity on depression treatment: A literature review. Quality in Sports, 14, 52858. View
Abdulrasool, M. D., Joda, E. O., & Alawady, A. A. (2020). The effect of psycho-physiological sports proposed in terms of the hormone endorphins serotonin and their relative results on mental fitness in the aged. Annals of Tropical Medicine and Public Health, 23(13B), 231-369. View
Mura, G., & Carta, M. G. (2013). Physical activity in depressed elderly: A systematic review. Clinical Practice and Epidemiology in Mental Health, 9, 125-135. View
Hossain, M. N., Lee, J., Choi, H., Kwak, Y. S., & Kim, J. (2024). The impact of exercise on depression: How moving makes your brain and body feel better. Physical Activity and Nutrition, 28(2), 43-51. View
Marsh, H. W., Hau, K. T., & Wen, Z. (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Structural Equation Modeling, 11(3), 320-341. View
Wei, H., Liu, B. P., & Jia, C. X. (2024). Association and biological pathways between lung function and incident depression: A prospective cohort study of 280,032 participants. BMC Medicine, 22, 160. View
Beller, J., Safieddine, B., Sperlich, S., Tetzlaff, J., & Geyer, S. (2024). Socioeconomic differences in limited lung function: A cross-sectional study of middle-aged and older adults in Germany. International Journal for Equity in Health, 23, 138. View
Wang, Y., Liu, M., Yang, F., Chen, H., Wang, Y., & Liu, J. (2024). The associations of socioeconomic status, social activities, and loneliness with depressive symptoms in adults aged 50 years and older across 24 countries: Findings from five prospective cohort studies. The Lancet Healthy Longevity, 5(9), 100618. View
Iovino, P., Nolan, A., De Maria, M., Ausili, D., Matarese, M., Vellone, E., & Riegel, B. (2023). The influence of social support on self-care is mediated by self-efficacy and depression in chronic illness: Key findings from the ‘SODALITY’ observational study. Aging & Mental Health, 27(4), 820-828. View
Berk, M., Köhler-Forsberg, O., Turner, M., Penninx, B. W. J. H., Wrobel, A., Firth, J., ... Marx, W. (2023). Comorbidity between major depressive disorder and physical diseases: A comprehensive review of epidemiology, mechanisms, and management. World Psychiatry, 22(3), 366-387. View
Ma, Y. H., Shen, L. X., Li, Y. Z., Leng, Y., Yang, L., Chen, S. D., ... Yu, J. T. (2023). Lung function and risk of incident dementia: A prospective cohort study of 431,834 individuals. Brain, Behavior, and Immunity, 109, 321-330. View
Bamrotia, J., Joshi, A. N., Paralikar, S., Kathrotia, R., Patel, V. K., & Rajendran, R. (2024). Effects of different types of physical activity on respiratory health parameters in elderly males: A cross-sectional study. Cureus, 16(5), e59759. View
Grande, G., Li, Y., Trevisan, C., Rizzuto, D., Kalpouzos, G., Ding, M., ... Qiu, C. (2024). Lung function in relation to brain aging and cognitive transitions in older adults: A populationbased cohort study. Alzheimer's & Dementia, 20(8), 5662-5673. View
Fettes, L., Bayly, J., Chukwusa, E., Ashford, S., Higginson, I., & Maddocks, M. (2024). Predictors of increasing disability in activities of daily living among people with advanced respiratory disease: A multi-site prospective cohort study, England UK. Disability and Rehabilitation, 46(20), 4735-4744. View