Journal of Comprehensive Nursing Research and Care Volume 10 (2025), Article ID: JCNRC-212
https://doi.org/10.33790/jcnrc1100212Research Article
Effectiveness of a Registered Nurse and Licensed Practical Nurse Delegation Communication Simulation to Improve Teamwork in Role Differentiation
Valerie Braddock*, Skadi Rodewald
Department of Nursing, East Stroudsburg University, 200 Prospect Street, East Stroudsburg, Pennsylvania 18301-2999, United States.
Northampton Community College, 3835 Green Pond Rd, Bethlehem, PA 18020, United States.
Corresponding Author Details: Valerie Braddock, DNP, RN, CCRN-K, Associate Professor, Department of Nursing, East Stroudsburg University, 200 Prospect Street, East Stroudsburg, Pennsylvania 18301-2999, United States.
Received date: 26th March, 2025
Accepted date: 16th June, 2025
Published date: 19th June, 2025
Citation: Braddock, V., & Rodewald, S., (2025). Effectiveness of a Registered Nurse and Licensed Practical Nurse Delegation Communication Simulation to Improve Teamwork in Role Differentiation. J Comp Nurs Res Care 10(1): 212.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Registered Nurses (RNs) and Licensed Practical Nurses (LPNs) communication is critical for ensuring patient safety, improving the quality of care, and fostering cohesive healthcare teams. This study evaluated the impact of a collaborative simulation experience on nursing students' confidence in working together. As healthcare systems newly integrate LPNs into acute care settings, the need for RNs and LPNs to collaborate effectively has become important. However, communication gaps and misunderstandings about the scope of practice often affect teamwork that could lead to potential medical errors. To address this concern, a community college in Northeastern Pennsylvania implemented a simulation to improve communication, collaboration, and delegation between RN and LPN students. The study assessed pre- and post-simulation confidence levels related to communication, delegation, and teamwork through surveys. Surveys revealed that both RNs and LPNs identified increased comfort and confidence in communication and collaboration after the simulation. However, both groups also reported concerns during emergent situations such as feeling hesitant to delegate, possess poor communication skills, and overall lack a sense of urgency. Fortunately, all participants voiced the value of the experience and hoped for future similar simulation experiences. The students verbalized an appreciation for teamwork and areas for further improvement. This study suggests that simulation experiences can be an effective tool in enhancing communication and increase confidence in collaboration and delegation, but continued education and feedback are essential to ensure that these skills translate to realworld clinical settings.
Keywords: Registered Nurse, Licensed Practical Nurse, Communication, Confidence, Simulation
Introduction
Effective communication is the cornerstone of collaborative healthcare delivery, particularly within nursing teams composed of registered nurses (RNs) and licensed practical nurses (LPNs). The dynamic interplay between RNs and LPNs is pivotal for ensuring patient safety, enhancing care quality, and fostering a cohesive work environment. Miscommunication, the failure to collaborate, and the inability to delegate tasks to properly licensed personnel can lead to significant medical errors. The inability to communicate effectively ultimately jeopardizes the well-being of patients, reduces patient satisfaction, and leads to workplace inefficiencies [1]. Through recognition of the critical role of seamless communication in nursing practice, nursing schools need to integrate simulation experiences into their curricula. These simulations offer realistic, controlled environments where nursing students can hone on their so called ‘soft skills’ which are communication, collaboration, and delegation. It is imperative for the learner to understand the nuances of interdisciplinary collaboration, and prepare for the complexities of real-world healthcare settings within a safe learning environment. By prioritizing these experiential learning opportunities, nursing education programs can better equip future nurses with the competencies required to thrive in diverse clinical environments. The meaningful application of soft skills ultimately improves patient outcomes and fosters professional excellence. The purpose of this article is to evaluate if nursing students, both RNs and LPNs, feel more confident working with each other in a collaborative simulation experience.
Review of Literature
As a result of the Covid-19 pandemic, healthcare facilities have been scrambling to ensure adequate staffing. The widespread loss of experienced RNs at the bedside, consequently required healthcare leaders to employ LPNs in the acute care setting [2]. Many of the currently employed registered nurses are not experienced in collaborating with LPNs or are familiar of a team model of nursing care delivery. It is recommended that for successful integration of Licensed Practical Nurses, the nursing faculty needs to ensure “relationship building, enhanced communication, frequent feedback, and collaboration” with RNs and LPNs is included in nursing program education [2]. Furthermore, RNs need to be aware of the LPN’s scope of practice so that they can collaborate and delegate care appropriately. According to the American Nurses Association statement on delegation, ”the delegated responsibility must lie within the parameters of the delegator’s authorized scope of practice under the Nursing Practice Act [3].” However, there are no specific guidelines as to the framework for this collaboration. In a literature review article published by Prentice et. al. [4], some basic guidelines for collaborative care and the importance of teamwork and collaboration are provided. But literature is lacking the evidence as to specific guidance that reflects positive or improved outcomes [4]. Nursing recognizes the need for the RN and LPN relationship. However, nursing lacks evidence to ensure effective relations that foster teamwork.
Simulated communication scenarios and activities have been proven effective methodologies to improve the clarity and effectiveness of communication in healthcare settings. When nursing students participate in high-fidelity simulation scenarios that foster communication skills, nursing students can identify the value of effective communication [5]. Furthermore, nursing students in emergency simulated experiences benefitted from the team communication experience which better prepared them for safe patient care [6]. Through a simulated experience, nursing students can work on their communication, collaboration, and delegation skills that help prevent medical errors when in clinical practice.
The failure to communicate effectively continues to be a serious cause of medical errors in the healthcare setting. Nursing students suffer from communication apprehension that can lead to poor patient outcomes [7]. Simulated experiences that foster communication skills and other soft skills can help with this apprehension. Due to changes in workload, technology, generational gap, lack of leadership, focus on individual performance, stress, and generally poor communication skills, effective communication is not prevalent at the bedside [1]. An increase in simulated teamwork communication experiences for nursing students would be beneficial.
Methodology
A community college in Northeastern Pennsylvania has both an RN and LPN accredited program. The college identified through the clinical-based curriculum that there is a lack of communication education and scope of practice awareness among different types of nursing disciplines. The focus on communication education is not equally addressed in the fundamental’s level of nursing among the programs. However, the LPN students have a greater awareness, including on their scope of practice, than their RN peers. This can be contributed to the fact that the learning content needs to be disseminated to the LPN students within a year versus to students in the two year RN program. It was also revealed that communication and collaboration is not regularly reinforced in clinical practice and simulation by each educator throughout each semester. On top of that, local community stakeholders expressed valid concerns that graduate nurses often fail to communicate effectively with other professionals and lack teamwork initiatives, which can have a detrimental impact on the patient. Consequently, a group of educators collaborated and created a specific simulation experience for this community college using Benner’s nursing theory from novice to expert as guide for simulation creation.
The concentration of the pilot simulation was on closing the communication gap, strengthen teamwork, and enhance the student's ability to provide quality and safe care through appropriate delegation. For this experience, both RN and LPN students needed to collaborate the care of a decompensating patient. A patient diagnosed with atrial fibrillation receiving a continuous intravenous heparin infusion who developed stroke-like symptoms was determined to be appropriate for this level of education. The patient in the emergent situation rapidly deteriorated and required prompt basic life support care. To enhance realism in simulation, a hybrid simulation style was selected. The scenario started with the standardized patient (SP) sitting in a chair showing symptoms. After the LPN and the RN determined the Rapid Response Team is needed, the standardized patient was switched to a high fidelity manikin. The incorporation of a SP allowed the simulation facilitators to evaluate the students’ ability to communicate with the patient and each other, make critical decisions, and demonstrate previously learning skills such as medication administration and maintaining patient safety.
The participants were selected from a student population enrolled in the second-semester medical-surgical course from both programs. These individuals were made aware of the pilot simulation approximately six weeks in advance and were instructed to complete and review previously lectured content related to the simulated topic. To avoid overloading the selected students with their regular assignments, the simulation coordinator provided specific readings and educational video clips on atrial fibrillation, stroke, and the effective Rapid Response Team (RRT). This was also necessary since the registered nursing students did not have had adequate electrocardiogram (ECG) education to date. However, their clinical instructor was actively involved in the study and provided hands-on ECG teaching at the clinical site. The participants also had access to a brief patient description and the learning objectives utilizing the National League for Nursing (NLN) format.
Prior to the simulation, all 12 students signed a video and photography release form and were informed in detail why they have been selected to participate. They were instructed to complete a paper and pencil pre-confidence survey. Theses survey questions in addition to express their feedback were ask in the post-survey. The emphasis of these identical surveys is strictly on their confidence level in collaborating and communicating with other nursing members, which was utilized to compare and contrast the effectiveness of the scenario. These five RN students and seven LPN students have not been in direct contact while in the program. Not knowing the acquaintances caused heighten anxiety among most students, which was anticipated by the educators. In order to alleviate this feeling, two different teambuilding games were selected prior to the actual simulation experience. During a set time, students were grouped with a student from the other program and through vocalizing decisions, the group with the most stable and highest structure won the game. A participant educator further asked questions to evaluate if the students got to know each other during these teambuilding exercises, which they did. When a group was participating in the simulated experiences, the other students were participating in a team-building discussion session.
It is important to state that this was not the students’ first simulation experience, but their first encounter collaborating with a nurse from a different discipline. The students were split into two groups with a mix of RNs and LPNs at random. Those participants that demonstrated satisfactory in clinical practice were selected to be the LPN and RN providing patient-centered care as seen as with the team nursing model in practice. The other students became designated members of the Rapid Response Team with the exception of the Team Leader. Also, these students did not learn of their specific roles until the assigned nurses called the RRT. However, the role of the Team Leader was purposefully given to a nurse educator to aid in the students’ assessment of communication, collaboration, and teamwork in a critical situation when they receive vital verbal instructions in a high-stake situation. Additionally, the patient assigned nurses and the students in the role of the Documenter in the RRT received tools assisting with communication in healthcare.
Following the formalities, the environment orientation, and the teambuilding exercises in prebrief, the selected LPN of group one received the patient report. Upon entering the patient’s room, the nurse had a brief time to decide on decisions that ranged from assessing, administering or holding prescribed medications, ensuring safety, and reaching out to the assigned RN. Once the latter was notified, they too were expected to perform assessment and interventions appropriate for this event. Due to the nature of the patient’s health status, the RRT was correctly notified and the remainder participants entered the patient’s room who was now transitioned to the manikin. The Team Leader performed the in-depth neurological assessments since the students were not familiar with the NIH-Stroke Scale. In addition to receiving and implementing specific verbal orders such as administering intravenous fluid and placing the simulated patient in the backboard and apply the ECG leads, the Team Leader also acted as the CPR coach (cardiopulmonary resuscitation) to guide the participants. The emergency event concluded with an order to transfer the patient to a higher level of care. Thereafter, each student of this group expressed their emotions and experience in writing in a separate location while the other participants of group two started their simulation experience. No changes were made for the second encounter.
For this study, the entire student encounter was documented. But only the audio-video recording of the actual patient encounter was reviewed with every participants in the debrief session. The simulation coordinator facilitated a meaningful discussion while the standardized patient and actively participating educators provided additional constructive feedback. The capture of every simulation aspect as well as the reflection and the Documenter forms and the surveys all were very critical to the educators. These elements assisted the educators to debrief, to evaluate students’ performances and to identify existing student needs at a later time. It was determined that teaching modifications are imperative to achieve course outcomes.
Results
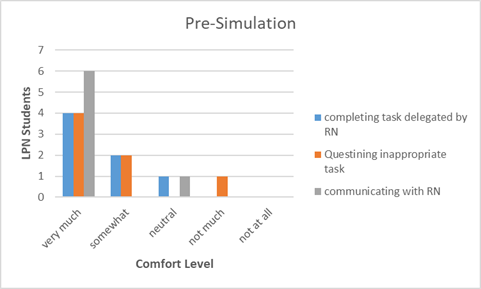
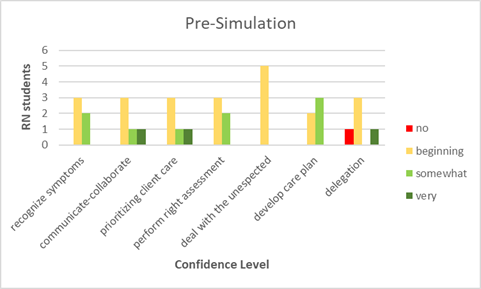
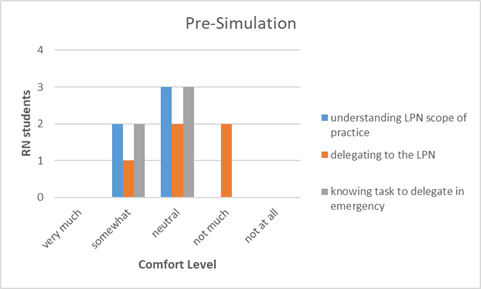
The pre-simulation and post-simulation confidence surveys were scored in tables to compare and contrast both results of that of the RNs and LPNs. The most significant finding was that both groups lacked confidence after the simulation was completed. The RNs stated having beginning confidence when identifying emergent situations and prioritizing care. However, these scores decreased according to the post-survey analysis. This can also be identified with the results of the LPN students. When reviewing the results of the communication and delegation questions specific to the RNs, most of the RN students felt more comfortable delegating and communicating with the LPNs. Similarly, the LPNs students felt more comfortable communicating and collaborating more with the RN students after their simulation encounter.
An informal debriefing session was conducted after the simulated experience to discuss performance and lessons learned. The overall feedback was that the students appreciated the simulated experience and had a greater appreciation for teamwork and communication. The facilitator also identified some positives and areas of improvement for each group as well. The instructors identified that there was poor communication with the Team Leader. All initial assigned patient nurses provided a report of the decompensated patient that was considered ineffective. The nurses failed to take notes from the patient report and lacked critical thinking to utilize the patient’s electronic health record to assist with providing efficient report when the RRT arrived. Furthermore, there were challenges with delegation and teamwork. The students "froze" many times or became so focused on a particular task that they were not engaged in the overall experience. The two students that were appointed to the role of the Documenter both struggled with appropriate documentation. Missed documentation ranged from recording assessment findings and also inform the Team Leader regularly. Lastly, there was an overall lack of urgency with the simulation in both groups. The participants were hesitant to ask for help in an emergent situation. This was discussed in detail within the debriefing session.
Below are tables that summarize the findings of the surveys.
Limitations of Study
This was a pilot simulation and the topic of the scenario was determined appropriate for the participants’ academic level. Nevertheless, areas of improvement were identified, such as clearer role assignments and ensuring that students know the equipment’s location and proper usage of the defibrillator in more detail. This would have limited the learners’ anxiety when encountering an unprecedented clinical situation. Additionally, the students had not worked with a standardized patient before this experience. They informally identified this to be a factor that affected their underperformance. Furthermore, the RN students were not synchronous in their curriculum with that of the LPN students. This discrepancy hindered some of these students from identifying the patient’s problem promptly and selecting appropriate nursing interventions. The sample size of students selected was small and the study was only conducted in a single Community College. Participants were predominantly female and there was not an equal number of RN and LPN students enrolled in the study.
Conclusion
The overall effectiveness of this simulation study improved collaboration and communication between the RN and the LPN students. During debriefing, students verbalized that they understand the need for clear communication and teamwork. They recognized that soft skills are imperative in providing quality and safe patient care and require recurrent practice and application in practice. The RN students expressed the role of the LPN is valuable to the nursing profession but they admitted that they would require formal education on delegation earlier in their studies. As for the LPN students, they also verbalized that making recommendations and questioning tasks the RN might delegate to them is necessary so that well-coordinated patient care can be delivered. Although the objectives of the simulated experience was not to evaluate performances of basic nursing skills in an emergency, it was determine that the educators need to foster and review soft skills more regularly and also modify their education on safely transferring the patient with unilateral unsteady gait.
In conclusion, this simulation study offered beginner and expert participants an opportunity to apply soft skills and previously learned content in an emergency situation. Albeit the limitations and mediocre outcomes achievement, this simulation scenario has been incorporated into the nursing curriculum in both programs since the study was conducted. The lead faculty members of the nursing programs have made adjustments based on the study’s findings but more appreciation and revamping is necessary to address the concerns revealed. It is noteworthy that a discussion with other healthcare program directors of the Community College and a local university has been set in motion. These individuals also stated that their students struggle with communication and teamwork among other disciplines in the clinical setting. Continuous feedback and evaluation will need to be collected and analyzed to adapt the simulation to the growing needs of the healthcare community.
This and similarly designed scenarios would be beneficial at the pre-licensure level and among interdisciplinary teams. Nursing students need to be aware of the roles and scope of practices of other healthcare team members. Simulationists must be mindful of, in example, respiratory therapy, physical and occupational therapy, sonography, and dieticians, when designing an interdisciplinary simulation scenario since they regularly collaborate with nursing. Again, this would be beneficial for the future nurses and other healthcare professionals but it would mainly reduce the medical errors and enhance patient outcomes.
The results of the simulated experience highlighted the need to provide RN and LPN collaborative experiences so that the students feel more confident and comfortable communicating and working with each other in clinical practice. Furthermore, continued education and experiences needs to be provided to both types of nursing students on the proper care of the decompensating patient. Perhaps more frequent simulations with a focus on communication, delegation, and teamwork would be more valuable in nursing education while also including other members of healthcare disciplines and universities to enhance further the collaboration development among students.
Based on this simulation, follow-up surveys after graduation and licensure acquisition should be administered to determine if the simulated experience helped in the transition to bedside patient care. It is the authors’ recommendation to distribute surveys at the six month level and then again at one-year post-graduation to the novice nurses. This would determine if the former students felt now more comfortable working with either the licensured RN or LPN in practice. The data of these follow up surveys would also be beneficial in altering the questions to better meet the currently enrolled student's needs. Lastly, consideration of adding other members of the healthcare team to simulated experiences would be useful to ensure better collaboration of care.
Acknowledgement
The authors would like to sincerely thank Dr. Judy Rex, Thomas Rush, Susan Bush, and Christine Collado for initiating the study and their continuous guidance throughout. Their expertise and recommendations contributed to the study’s success. We are also grateful to the LPN and RN students who participated in this study and brought the deficits to light. Additionally, we express gratitude to the professional lab assistant Cindy Martin and the Northampton Community College Pocono IT team members for an uninterrupted flow of the simulation experience. Finally, we appreciate the collaboration with Antoinette McCreary and Brad Briddes who added realism to the experience as the standardized patient.
Conflict of interest
The authors of this research declare no competing interest regarding this study.
References
Barve, M. (2025, April 2). Why today's generation of nursing staff struggles with teamwork in patient care—Causes, impact, and solutions. LinkedIn.
Desir, M., Langhourn, D., Green, J., & Tao, H. (2023). The impact of a Licensed Practical Nurse–Registered Nurse care delivery model on the work environment. Nurse Leader, 22(1), 95–103. View
American Nurses Association. (2019). National guidelines for nursing delegation (Effective 04/01/2019) [Position Statement].
Prentice, D., Moore, J., Crawford, J., Lankshear, S., & Limonges, J. (2020). Collaboration among registered nurses and licensed practical nurses: A scoping review of practice guidelines. Nursing Research and Practice. View
Arrogante, O., Ortuño-Soriano, I., Fernandes-Ribeiro, A., Raurell-Torredà, M., Jiménez-Rodríguez, D., & ZaragozaGarcía, I. (2025). The impact of high-fidelity simulation training on first-year nursing students' attitudes toward communication skills learning: A quasi-experimental study. Clinical Simulation in Nursing, 101. View
Bourke, S., McKenna, L., Cooper, S., & Lam, L. (2024). Contextual determinants impacting final year nursing students' emergency team communication during deteriorating patient simulations: A grounded theory study. Nurse Education Today, 138. View
Morris, D. (2023). Communication barriers for nursing students: Communication apprehension, emotional intelligence, and perceived communication competence. Teaching and Learning in Nursing, 18(3). View