Journal of Dermatology and Advanced Clinical Care Volume 2 (2024), Article ID: JDACC-103
https://doi.org/10.33790/jdacc1100103Case Report
A Rare Case of Generalized Rruptive Xanthoma
Jelica P. Vukicevic
Professor, School of Medicine, Department of Dermatovenereology, University of Belgrade, Belgrade, Serbia.
Corresponding Author Details: Jelica P. Vukicevic, Professor, School of Medicine, Department of Dermatovenereology, University of Belgrade, Belgrade, Serbia.
Received date: 18th July, 2024
Accepted date: 12th August, 2024
Published date: 14th August, 2024
Citation: Vukicevic, J. P., (2024). A Rare Case of Generalized Rruptive Xanthoma. J Dermatol Adv Clin Care, 2(1): 103.
Copyright: ©2024, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Eruptive xanthoma (EX) is a benign rare dermatosis and it’s considered that EX is reported more in the literature than in clinical practice. It’s associated with metabolic imbalance caused by hypertriglyceridemia and unregulated type 2 diabetes. Lipids present in a larger amount in serum leak through of capillaries into the dermis where they are phagocytosed by macrophages and typical foam cells are formed. This localized accumulation of lipids in the dermis is bases for the appearance of EX [1-3]. It is very important to know that these metabolic disorders can lead to numerous complications (diabetic coma, lipemia retinalis, fatal complications of acute pancreatitis, damages of coronary arteries), and quick diagnosis and therapy are very important [4].
Case report
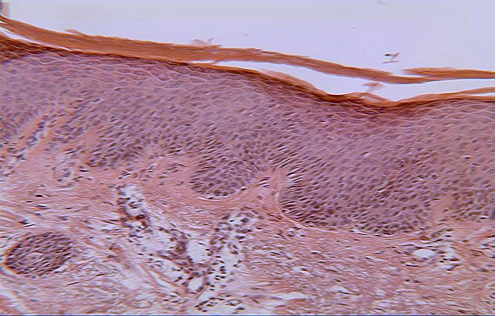
Herein was presented 43-year-old man from outpatient clinic who complained of a sudden skin rash that appeared 3 days ago. The following data were significant in his medical history: alcoholism, high blood pressure, hyperlipidemia, poorly controlled and unregulated diabetes type 2, arthritis urica. Type 2 diabetes and hyperlipidemia were diagnosed 2 years ago. According to the endocrinologist’s medical documentation, the glicemic values were up to 8,1 mmol/L, triglicerides 11, 4 mmol/L and holesterol 6,1 mmol/L. The drugs, he was treated with, include simvastine 20 mg daily, atenolol, NSAIDs. Antidiabetic diet, diet for hyperlipidemia and hyperuricaemia were also advised. The patient did not mention similar metabolic diseases in the family, especially elevated cholesterol levels (VLDL) since childhood and cardiovascular attacks in young family members. He stated that the rash was preceded by stress and the consumption of large amounts of alcohol. On examination, the patient was obese with pale-erythematous to erythematous-brownish papules 1 to 5 mm in diameter on the neck (Fig.1a), trunk and extremities (Fig.1b, 1c), more on the extensor surfaces. These papules were not accompanied by subjective symptoms such as itching, pain, burning. The patient complained of dull pain in the epigastrium. Also, swelling with pain in the right toe was noticed. Laboratory analyses were as follows: SE 10 mm/h (0-20 mm/h), complete blood count without pathological changes, triglycerides 97.1 mmol/L (<1,70 mmol/L), glucose 12 mmol/L (3,9-6,1 mmol/L), cholesterol 23.5 mmol/L (0,00-5,20 mmol/L), acidum uricum 665.9 mmol /L (210-452 mmol/L). In the urine sediment, proteinuria+, hyaline cylinders. Histopathology, staining with hematoxylin and eosin (H & E ), revealed foamy histiocytes in papillary and reticular dermis and extracellular loose lipids that indicated the diagnosis of EX (Fig.2) (H & E, ×100). Ultrasound of the abdomen didn’t show pathological lesions. The patient was hospitalized in the Clinic for metabolic disorders.
Discusion
Eruptive xanthoma is a rare disease with a prevalence of 18 cases per 100.000 inhabitants [4]. Elevated triglyceride values are the basis for the appearance of EX, and it is estimated that 8.5% of patients with high triglycerides level developing this condition [5]. Hypertriglyceridemia is associated with high concentrations of chylomicrons and very low density lipoproteins (VLDL). High concentrations of trigycerides may be familial due to decreased lipolysis caused by lipoprotein lipase deficiency or may be secondary (diabetes, obesity, estrogen therapy, alcoholism, renal insufficiency). Secondary hypertriglyceridemia can be, also, a aftermath of therapy with retinoids, cyclosporine, tacrolimus, corticosteroids, some HIV medications. Decreased lipolysis may be also acquired (diabetes, beta blockers, hypothyroidism) [2]. Cutaneous xanthomas appear when lipids are deposited in the dermis within macrophages, known as foam cells, and in the extracellular matrix.
In addition to EX, there are 4 types of xanthomas. One of the most common is xanthelasma characterized by ring-shaped, soft, eyelid plaques that may or may not be associated with hyperlipidemia [6]. Tendon xanthomas are associated with genetically determined hypercholesterolemia. They are nodular deposits of cholesterol in the tendons, commonly on the dorsal surfaces of the hands and the achilleas tendon. Plane xanthomas are usually presented by localised (especially on the palms) or generalised yellowish macules or slightly elevated plaques often with a central white area. Verruciform xanthoma is characterized by a proliferative lesion of the oral cavity.
Skin lesions in EX are in the form of yellowish- pink or brownish papules with 1 to 5 mm in diameter, scattered simetrically on the arms, legs, back, mainly on their extensor surfaces. Herein is shown generalized XE with characteristic papules on the neck, trunk and extremities. Papules are asymptomatic or may be accompanied by pruritus, tenderness, or a burning sensation. Koebner's phenomenon can be positive [3,7,8]. EX can appear on the skin associated with other dermatoses. Virath R, et al. presented a case of EX and Granuloma annulare, while Ahn JY, et al. described EX in Mycosis fungoides [9,10].
In the differential diagnosis should be considered disseminated granuloma annulare, generalized eruptive histiocytoma and non Langerhans cell histiocytosis.
EX is an important clinical sign for physicians because hypertriglyceridemia can lead to acute pancreatitis, cardiovascular events and treatment should be started early [4]. The essence of this therapy is decreasing the levels of fat and glucose in the blood, reducing body weight. Witztum JL. et al., presented a new drug developed by antisense technology effective in treating patients with familial chylomicronemia syndrome [11].
Conclusion
Here is presented a rare case of generalized eruptive xanthoma in a patient with type 2 diabetes, hyperlipidemia and uric arthritis. The apperance of the rash was preceded by stress and alcohol abuse. Urgent and adequate treatment can prevent life-threatening complications.
Conflict of interest:
The authors have no conflicts of interest to declare that are relevant to the content of this article.
References
Hsueh, Y. C., Chou, C. L., Lee, T. I., (2019). Diabetic dyslipidaemia with eruptive xanthoma. Cleve Clin J Med; 86(9):575.
Kashif, M., Kumar, H., Khaja, M., (2016). An unusual presentation of eruptive xanthoma. Medicine; 95(37):1-3. View
Tang, K., Wu, M., Li, J., (2023). Eruptive Xanthomas. Jama Dermatol; 159(4):449. View
Ohtaki, S., Ashida, K., Matsuo, Y., et al. (2022). Eruptive xanthomas as a marker for metabolic disorders: A specific form of xanthoma that reflects hypertriglyceridemia. Clin Case Rep; 10: e05671 View
Vangara, S. S., Klingbeil, K. D., Fertig, R. M., et al. (2018). Severe hypertriglyceridemia presenting as eruptive xanthomatosis. J Family Med Prim Care; 7:267-70. View
Lee, S. Y., & Sheth, C. A., (2019). Eruptive xanthoma associated with severe hypertriglyceridemia and poorly controlled type I diabetes mellitus. J Community Hosp Intern Med Perspect; 9(4):344-6. View
Zhao, C., & Li, H., (2023). Eruptive xanthoma associated with hypertriglyceridemia and diabetes. Clinical; 52(6). View
Zaremba, J., Zaczkiewicz, A., Placek, W., (2013). Eruptive xanthoma. Postep Derm Alergol; XXX,6:399-402. View
Virath, R., Mehta, S., Balai, M., et al. (2021). Eruptive xanthoma and Granuloma annulare in association with metabolic disorder. Indian J Dermatol; 66(2):199-201. View
Ahn, J. Y., Cho, S. H., Seo, S. J., et al. (2006). Eruptive xanthoma in Mycosis fungoides; 18(2):82-85.
Witztum, J. L., Gaudet, D., Freedman, S. D., Alexander, V. J., Digenio, A., Williams, K. R., et al. (2019). Volanesorsen and triglyceride levels in familial chylomicronaemia syndrome. N Engl J Med; 381(6):531-42. View