Journal of Dermatology and Advanced Clinical Care Volume 3 (2025), Article ID: JDACC-104
https://doi.org/10.33790/jdacc1100104Case Report
Pseudo - Kaposi Sarcoma in a Young Obese Male
Jelica P. Vukicevic
Professor, School of Medicine, Department of Dermatovenereology, University of Belgrade, Belgrade, Serbia.
Corresponding Author Details: Jelica P. Vukicevic, Professor, School of Medicine, Department of Dermatovenereology, University of Belgrade, Belgrade, Serbia.
Received date: 20th February, 2025
Accepted date: 04th April, 2025
Published date: 07th April, 2025
Citation: Vukicevic, J. P., (2025). Pseudo - Kaposi Sarcoma in a Young Obese Male. J Dermatol Adv Clin Care, 3(1): 104.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Pseudo-Kaposi sarcoma (PKS) or Acroangiodermatitis (AAD) is a rare disease that is sometimes difficult to distinguish clinically and histologically from Kaposi sarcoma and includes two entities: Acroangiodermatitis of Mali which is associated with chronic venous insufficiency and occurs in old age, and, Stewart Blefarb and Adams syndrome (SBS) which occurs in younger people and is conditioned by arterio-venous malformations. Here is presented a young (31 years old), obese (120 kg) man with erythemo-brownish plaques in the lower legs that last for 4 years. Histopathological verification indicated lobular proliferation of capillaries and small lymphatics in the dermis. The perivascular infiltrate consisted of histiocytes, lymphocytes. Immunohistochemically, CD34 staining was positive in vascular endothelium and negative in interstitium cells.Staining for HHV8 was negative. The correlation of the clinical and immunohistological picture indicated Acroangiodermatitis of Mali.
Keywords: Acroangiodermatitis of Mali, Histopathology, Immunohistochemistry Kaposi Sarcoma, Promontory Sign
Introduction
Pseudo Kaposi sarcoma (PKS) or Acroangiodermatitis (AAD) (synonyms) is a benign disease characterized by the reactive proliferation of small blood vessels in the skin. It is divided into two groups: AAD of Mali, which is mainly associated with chronic venous insufficiency, and Stewart Blefarb and Adams syndroma (SBS) which is caused by some inherited and acquired vascular disorders. AAD of Mali occurs in the form of erythemo-brownish or purple papules, nodule, plaques and ulcerations on the lower extremities. Clinically, it is very reminiscent of Kaposi sarcoma (KS) whose incidence increases with the number of AIDS patients and therefore a clinicopathological correlation is needed for an adequate diagnosis of these two entities [1-5].
Case report
A 31-year-old man who complained of redness and pain in the left lower leg for 4 years was presented. According to the medical records, the patient was treated in hospital as panniculitis with erythromycin 500 mg 4 times a day for 2 weeks and than with doxycycline 2 x 100 mg a day for 2 weeks. 0.1% clobetasole dipropionate was applied topically. On examination, the patient is obese. On the front side of the left lower leg a purple, well demarcated plaque with a diameter of 10x15 cm was noticed, warm and painful on palpation. On the surface of the plaque several shallow ulcerations up to 1cm in diameter covered with crusts are noted. In the surrounding skin, predominantly below and medial to the lower part of the lesion, scattered livid macules were seen. From the upper part of the lesion towards the knee stretched the tattoo (Figure1). The following laboratory analyzes were performed: C- reactive protein 13.78 mg/l, glucose 6.9 mmol/l, HgA1C 6.3%, while complete blood count, urea, creatinine, hepatogram and ionogram were within normal limits. Antistreptolysin O titer, hepatitis B antigen, hepatitis C antibody, HIV 1 and 2 antibodies were negative, Mantoux test was positive and Quantiferon –TB Gold test negative. Chest X ray and ultrasound of the abdomen are within normal limits. Dopplerultrasonography of the vessels of the lower extremitie revealed mild degenerative changes in the walls of the arteries with normal blood flow.
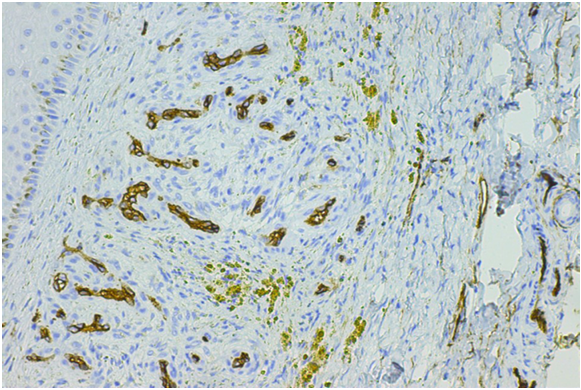
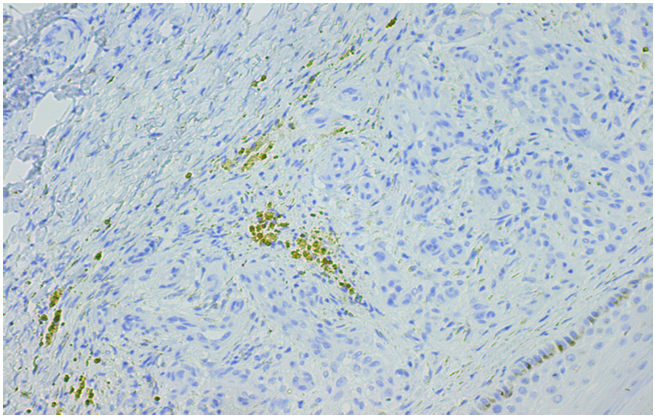
Deep veins are unchanged and without signs of deep vein thrombosis. The saphena magna and the snaphena parva veins are normal in appearance with competent valves. In both legs, higher to the left, there is an enlarged network of superficial venous vessels with no signs of fresh venous thrombosis. In the distal parts of the left leg, edema is visible. A biopsy of the lesion was taken, and histopathological analysis indicated acanthosis and spongiosis in the epidermis.In the dermis, lobular proliferation of capillaries, dilated irregular dermal lymphatics and multiple fibroblasts and lymphocytic infiltrate in the interstitium. Hemosiderophages and focal extravasation of erythrocytes are also visible (Figure 2). The results of immunohistochemical staining of proliferated capillaries in the dermis indicated CD34+; CD31+; factor VIII+; D2-40-; HHV8- (Figure 3a,b), while the results of staining of dermal lymphatics were as follow: CD34+; CD31+; factor VIII+; D2-40+; HHV8(-). The patient denied other disorders, as well as hereditary ones. Erythromycin 4x 500 mg per day, elastic bandage, and a local emollient ointment were introduced into the therapy. In one of the following controls, deterioration of the condition and appearance of the same lesion on the right lower leg were noticed. Oval scars appeared along the medial edge of the lesion on the left leg and previously livid macule in the surrounding lower and medial part took a brownish color. On the right lower leg, at the level of the lesion on the left leg,there was a brown plaque measuring about 6x6cm of irregular shape surrounding with livid eritema. Nearby, a brownish, oval plaque measuring about 2x2cm with a scar in the center was present.Edema of the lower legs was visible without clinically pronounced varicose veins (Figure 4). The femoral, popliteal and pedal pulses were well felt. Due to worsening of the skin lesions, the introduction of dapson into the therapy was proposed, but the patient refused it.
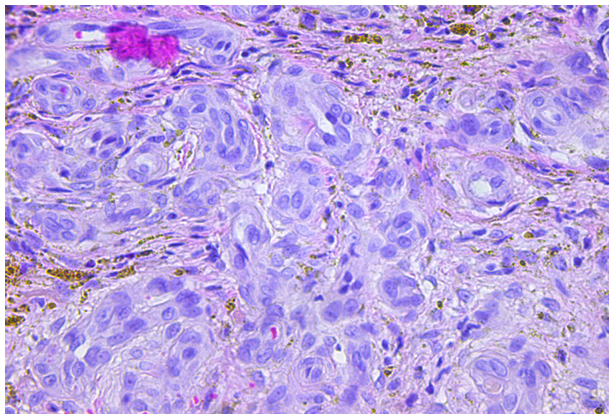
Figure 2. Histopathology in papilary and reticular dermis revealed lobular capillaries proliferation, irregular dermal lymphatics with fibroblasts and histiocytes in the interstitium.( H and E, x 200).
Discusion
Pseudo Kaposi sarcoma or acroangiodermatitis is a rare dermatosis that is sometimes difficult to distinguish clinically and histologically from KS. The term AAD was established by Mali in 1965, and this form of disease occurs more often in older men with chronic venous insufficiency (6). In 1967, Stewart Blefarb and Adams described the same changes in a patient with arteriovenus malformation (7), while in 1970 Echart noticed the clinical and histopathological similarity of AAD with KS and established the term Pseudo-Kaposi sarcoma. AAD of Mali is associated with chronic venous insufficiency and increased venous pressure. Increased venous pressure and chronic venous insufficiency lead to hypoxia, damage to endothelial cells, increased capillary permeability and penetration of blood cells into the perivascular spaces with the appearance of edema, reactive neovascularization, consequent inflammation. Rarely occurs in chronic renal insufficiency treated with haemodialysis, after kidney transplantation, in cases of limb paralysis or amputation stumps. Individual cases of spontaneous occurrence of this disease are also described [1-4]. Clinically, it occurs in the form of erythemolivid papules, nodules, and plaques that can exudate. Cutaneous lesions are on the lower extremities, bilaterally in the chronic stages of the disease, most often on the lower legs and dorsums of the feet, more often in the elderly. In SBS, arteriovenous malformations are present at birth, the lesions are unilateral, and in addition to the skin, internal organs are also affected. As the clinical picture of AAD of Mali resembles KS, it is necessary to do a histopathological analysis of the lesions, and, in particular, immunohistochemical analyses that allow the final differentiation between AAD and KS.The histological picture of AAD and KS is very similar in the early stages of the disease and is characterized by reactive lobular proliferation of the small vessels in the papillary and reticular dermis with erythrocyte exastravasation and hemosiderin deposits in the edematous perivascular spaces [1,3]. In addition, in the perivascular spaces, hyperplasia of fibroblasts and the presence of an inflammatory cellular infiltrate consisting of lymphocytes, eosinophils and histiocytes are observed. Horizontally positioned spindle cells can also be seen. In the deep dermis, thickened venules may be present. KS is characterized by a promontory sign [8], where newly formed small vessels appear in the larger vascular spaces. Also, proliferated vessels in AAD are separated by small zones of edema, while in KS they lie back to back to each other [8,9]. Mild fibroblast proliferation occurs in AAD and KS, but these fibroblasts are CD34+ in KS and negative in AAD [10]. KS is also characterized by atypia of endothelial cells, grouped branched hyperchromatic, polymorphic spindle cells, as well as the presence of plasma cells in the inflammatory infiltrate. Staining at HHV/8 was negative and with CD 34 staining sufficient to immunohistochemically rule out Kaposi sarcoma (11). AAD of Mali treatment includes: dapson, erythromicin, doxycycline in the systemic treatment, elastic bandage and corticosteroid ointments topicaly [5,12,13].
Conclusion
A rare case of a young, obese man who, due to long-term elevated venous pressure in the small pelvis and lower extremities, with consequent enlargement of the network of superficial blood vessels, developed AAD of Mali, a disease that occurs more often in the elderly with chronic venous insufficiency and which, due to its clinicopathological similarity to KS, requires adequate diagnostic procedures.
Conflict of interest:
The authors declare no conflict of interest.
References
Chea, E.P., Rutt, V.L., Levin, J., McClain, R., Purcell, S. M.(2019). Acroangiodermatitis of Mali and Stewart-Bluefarb syndroma. Cutis,103,336-339.View
Singh, S.K.,&Manchanda, K.( 2014). Acroangiodermatitis ( Pseudo-Kaposi sarcoma). Indian Dermatol Online J, 5(3),323- 325. View
Lugović, L., Pusic, J., Situm, M., Buljan, M., Bulat, V., Sebetić, K., (2007). Acroangiodermatitis (Pseudo-Kaposi sarcoma): Three case reports. Acta Dermatovenerol Croat,15,152-157. View
Li, Y., Li, W., Zhang, M., Yang, X., Li D.(2013). Pseudo- Kaposi,s sarcoma: A rare case and review. Clin Cosmet Investig Dermatol,16,1319-1323.
Mehta, A.A., Pereira, R.R,, Nayak, C.S., Dhurat, R.S.(2010). Acroangiodermatitis of mali: a rare vascular phenomenon. Indian J Dermatol Venereol Leprol, 76 (5), 553-556. View
Mali, J.W., Kuiper, J.P., Hamers A.A. (1965). Acro- angiodermatitis of the foot. Arch Dermatol, 92 (5), 515-518. View
Bluefarb, S.M., Adams, L.A. (1967). Arteriovenous malformation with angiodermatitis, stasis dermatitis simulating Kaposi´s disease. Arch Dermatol, 96,176-181 View
Fernandez- Florens, A., Rodriguez R. (2010).Promontory sign in a reactive benign vascular proliferation. Am J Dermatopathol, 32 (7), 700-703. doi: 10.1097/DAD.06013e3181cf0ae5. PMID: 20577080 View
Kharkar, V., Gutte, R., M., Khopkar, U., Mahajan, S., Chikhalkar, S. (2009).Kaposi's sarcoma: a presenting manifestation of HIV infection in an Indian. Indian J Dermatol Venereol Leprol, 75 (4), 391-393. doi:10.4103/0378-6323.53137. PMID:19584466 View
Konitakis, J., Narvaez, D., Claudi A. (1996). Expression of the CD34 antigen distinguishes Kaposi,s sarcoma from Pseudo Kaposi,s sarcoma (acroangiodermatitis). Br J Dermatol, 134,44-46. View
Fernandez, R., Verea M. M., Martinez, W., Yebra- Pimentel, M.T., Fonseca E. (2007). Bilateral Pseudo Kaposi sarcoma in upper limbs. Actas Dermosifiliogr, 268-270. View
Hayek, S., Atiyeh, B., Zgheib, E. (2015). Sewart- Bluefarb syndroma: review of the literature and case report of chronic ulcer treatment with heparin sulfate (Cacipliq20). Int Wound J, 12,169-172. View
Rashkovsky, I., Gilead, L., Schamroth, J., Leibovici, V. ( 1995). Acro-angiodermatitis: Review of the literature and report of a case. Acta Derm Venereol, 75(4),475-478. View