Journal of Dermatology and Advanced Clinical Care Volume 3 (2025), Article ID: JDACC-105
https://doi.org/10.33790/jdacc1100105Case Report
The Effectiveness of Hybrid Peel (99% Spongilla spicules and 0.5% Beta Hydroxy Acids) in Treating Acne-Prone Skin: A Presentation of 4 Cases
Theressia Handayani1,2*, and Stefani Luziani3
1dr Theressia Anti-Aging Clinic, Yogyakarta, Indonesia.
2Bethesda Hospital, Yogyakarta, Indonesia.
3Faculty of Medicine, Universitas Udayana, Denpasar, Indonesia.
Corresponding Author Details: Theressia Handayani, dr Theressia Anti-Aging Clinic, Yogyakarta, Indonesia.
Received date: 07th March, 2025
Accepted date: 17th April, 2025
Published date: 19th April, 2025
Citation: Handayani, T., & Luziani, S., (2025). The Effectiveness of Hybrid Peel (99% Spongilla spicules and 0.5% Beta Hydroxy Acids) in Treating Acne-Prone Skin: A Presentation of 4 Cases. J Dermatol Adv Clin Care, 3(1): 105.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Acne vulgaris (AV) is a prevalent dermatological disorder, affecting over 90% of adolescents and persisting into adulthood in around 12–14% of individuals. Although this condition is generally regarded as mild, it imposes a significant economic and psychological burden on society. In the treatment of acne and acne lesions, chemical exfoliation is a frequently used procedure. Spongilla spicules have been used as dispersed microneedles to improve the penetration of various therapeutics and nanoparticles by disrupting the skin barrier. No research has discussed the effectiveness of hybrid peel contains 99% spongilla spicules and 0.5% Beta Hydroxy Acids (BHA) in treating acne-prone skin.
Case Report: Four subjects, aged 17-36, with varying degrees of acne, received the hybrid peel treatment. The dose administered during a single session was 3 mL of BHA 0.5% serum with 0.3 grams of Micro Spicules (silica) applied topically. Subsequently, a cell booster serum, face and neck mask, and sunscreen with SPF 50 are administered. Patients were subjected to three treatment sessions, with a two-week interval between sessions. The evaluation was conducted by observing the patient's facial skin condition and capturing photographs before and after three treatment sessions. The evaluation results indicated a considerable improvement in all subjects' acne and skin texture.
Conclusion: The hybrid peel, which contained 99% spongilla spicules and 0.5% beta hydroxy acids, effectively treated acne-prone skin.
Keywords: Hybrid Peel, Spongilla Spicules, Acne
Introduction
Acne vulgaris (AV) is a prevalent dermatological disorder, affecting over 90% of adolescents and persisting into adulthood in around 12–14% of individuals [1,2]. The pathophysiology of acne involves Propionibacterium acnes colonization, inflammation, increased keratinocyte proliferation in the follicular infundibulum, and hypersensitive androgen-responsive sebaceous glands. It is a disorder of the pilosebaceous units, clinically defined by seborrhea, comedones, papules, pustules, nodules, cysts, and, in certain instances, scarring [3,4]. Although this condition is generally regarded as mild, it imposes a significant economic and psychological burden on society. Quality of life is compromised as a result of patients' elevated levels of anxiety, depression, and low self-esteem. Consequently, the primary objective of treatment should be to enhance the quality of life and reduce the physical and esthetic burden of the disease through early intervention [5-7].
Acne can be treated with a combination of topical, systemic, chemical peels, dermabrasion, and light treatment. The approach to treatment may differ based on the severity and form of acne, as well as individual factors such as age, skin type, and medical history [3,7,8]. Retinoids, vitamin A derivatives, are used as topical therapies for mild to severe acne. However, topical retinoids may induce significant skin irritation, necessitating titration at the commencement of treatment to facilitate patient adaptation. Furthermore, topical retinoids and retinoid analogs present a risk of teratogenic effects. Tazarotene is classified as a pregnancy category X medication and is contraindicated in pregnant women [9].
Chemical peels, or chemical exfoliation, are cosmetic procedures that include the application of substances to the skin to eliminate the upper layers by controlled destruction of the epidermis, with or without affecting the dermis. This results in skin regeneration and remodeling, enhancing the texture of the skin's surface [1,2,10]. In the treatment of acne and acne lesions, chemical exfoliation is a frequently used procedure [11,12]. Based on the extent of penetration, chemical peels are categorized as superficial (epidermis papillary dermis), medium (papillary to upper reticular dermis), and deep (mid-reticular dermis). Dermatologists are increasingly using superficial and medium-depth chemical peels to treat acne vulgaris. Its distinct pathophysiological factors are targeted by their chemical properties [5].
Spongilla spicules are tiny, needle-like structures derived from Spongilla lacustris, a freshwater sponge in the phylum Porifera and the class Demospongiae [13]. Most sponges are composed of spicules that are typically calcareous or silicious and serve as structural support [14]. Spongilla spicules have been used as dispersed microneedles to improve the penetration of various therapeutics and nanoparticles by disrupting the skin barrier. In a dose-dependent manner, Spongilla spicules can physically disrupt the epidermis and remain within the skin for more than 72 hours, making them a safe, effective, and convenient skin delivery strategy [15].
No research has discussed the effectiveness of hybrid peel contains 99% spongilla spicules and 0.5% Beta Hydroxy Acids (BHA) in treating acne-prone skin. Therefore, we present a case series of acne vulgaris in a patient who had a topical application of a hybrid peel containing 99% spongilla spicules and 0.5% Beta Hydroxy Acids (BHA).
Case Report
The data were collected from patients who visited a private clinic. Each patient provided informed consent and agreed to the publication of the case. Clinical photographs were taken of four participants before treatment: three females (non-pregnant) and one male. The subjects' ages varied from 17 to 36. This study does not include all types of acne because it is a case report, and only four people were chosen to be reported. Adolescent and young adult patients who have not had treatment in the last three months and do not use antibiotics are among the eligibility criteria. In this study, the patient's hormonal status was not examined. The patient had no prior treatment for their acne issues.
The initial phase of the treatment is preparation, which includes cleansing and extraction. This phase aims to discharge skin impurities by cleansing and extracting comedones. Then, disinfect the treatment area. Mix an appropriate quantity of BHA 0.5% serum (3 mL) with 0.3 grams of Micro Spicules (silica). Apply drops of this mixture to cleansed skin using a spatula or swab. Gently press the spicule against the skin surface and into the pores using fingertips. Depending on the individual, a tingling sensation may be caused during the delivery process of spicules into the skin. Apply 2 mL of cell booster serum by gently pressing with fingertips to absorb into the skin, and avoid rubbing. Following this, apply a facial and neck mask to the treated area. Remove the mask sheet after 10 to 15 minutes. The final stage involves applying a sun cream with SPF 50 to the entire face using your fingertips to ensure gentle absorption. The severity of acne vulgaris was not graded in this study, and the lesions were documented using photographs.
The initial patient was presented in Figure 1. Mr. K, 17 years old, and has a history of acne that has not improved for the past three years. This patient has numerous blackheads and milia. The patient underwent hybrid peel treatment three times, with a two-week interval between sessions. The evaluation revealed a significant reduction in large pores, acne, uneven texture, and scarring.

Figure 1. Representative clinical photos of a 17-year-old patient before (A) after three hybrid peel treatments (B).
The second patient was presented in Figure 2. Miss V, 19 years old, has been suffering from acne since 14 years old. Many inflammatory lesions were present on the patient's facial skin. The patient underwent three sessions of hybrid peel treatment. The evaluation revealed that the number of active acne inflammatory lesions had decreased.
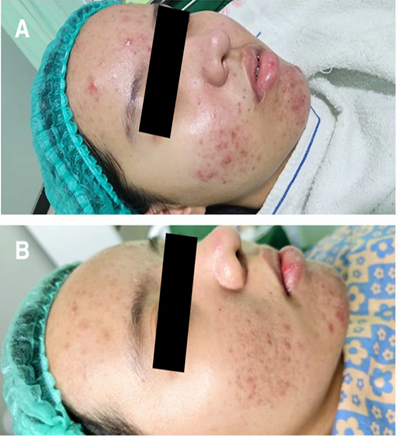
Figure 2. Representative clinical photos of a 19-year-old patient before (A) after three hybrid peel treatments (B).
The third patient was presented in Figure 3. Ms. S, a 25-year-old patient, has chronic acne that began during her adolescence. The patient has numerous acne lesions and an uneven skin texture. The hybrid peel treatment was administered to the patient three times, with a two-week interval between sessions. The evaluation results indicated that the acne had significantly improved, as well as the texture of the skin.

Figure 3. Representative clinical photos of a 25-year-old patient before (A) and after hybrid peel treatment (B).
The fourth patient was presented in Figure 4, Mrs. S, 36 years old, and has suffered from recurrent acne since her teenage years. The patient received a hybrid peel treatment in three sessions, with a two-week interval between sessions. Significant improvements in acne and scarring were observed following treatment.

Figure 4. Representative clinical photos of a 36-year-old patient before (A) and after three hybrid peel treatments (B)
After three treatment sessions, we observed a more pronounced decrease in the presence of acne, including pustules, papules, and comedones. All patients' skin conditions improved. The adverse effects identified in this study were solely mild, including erythema and pruritus. The follow-up period for patients ranged from 4 to 12 weeks. No recurrence was observed in patients; however, further follow-up is necessary to determine the potential for recurrence.
Discussion
Acne vulgaris can be managed through various treatment modalities [7]. The chemical peel is widely regarded as the most cost-effective, established, safe, and non-invasive cosmetic procedure. Combination peels enable clinicians to use lower concentrations of single ingredient peels while simultaneously combining the synergistic effects of agents to achieve rapid and increased results [1]. Sponges are multicellular marine organisms supported by a hard skeleton and feature soft tissue suspended in a jelly-like proteinaceous matrix. The deposition of calcium carbonate or silicon dioxide [16,17] regulates the skeletal structure.
Spongilla spicules have been documented as a natural dermabrasive option for addressing many skin issues, such as hyperpigmentation, superficial scars, sun-damaged skin, fine wrinkles, enlarged face pores, and comedones. Massaging spongilla spicules onto the skin helps the epidermal layers be mechanically separated, decreasing keratinocyte cohesiveness [16]. Spongilla spicules possess the capability to exfoliate the epidermal layer and enhance acne conditions. The microdermabrasion impact of spongilla spicules cleaner enhances pore keratinization in acne-prone skin and suppresses the proliferation of Propionibacterium acnes, hence ameliorating acne lesions. Spongilla spicules work similarly to microneedles in that they make tiny holes in the skin. Compared to conventional microneedle roller pins, these spicules are much tiny and are about a sixth the size of skin pores. They pierce the dermis to improve the transport of active substances and stimulate microcirculation [13,17].
The composition of 99% Spongilla spicules and 0.5% Beta Hydroxy Acid (BHA), which has also been used in skincare product formulation, has been studied in relation to acne treatments. By combining chemical and physical exfoliation methods, acne has been effectively treated. The choice of 0.5% BHA is strategic to balance efficacy and skin tolerance. Salicylic acid, a lipophilic BHA, penetrates deep into pores to dissolve sebum and exfoliate dead skin cells. Higher concentrations, such as 1% or 2%, may increase the risk of skin irritation, especially when combined with physical exfoliants like Spongilla spicules. Therefore, 0.5% is selected to minimize potential adverse effects while maintaining therapeutic benefits [18].
According to a study conducted by Lee et al., the prevalence of cysts, pustules, and cysts decreased in all 14 clinicians who participated after three weeks, and the acne grade improved substantially after seven weeks. In particular, the treatment enhanced 78.5% of pores, 71.4% of acne, and 95.7% of acne scars. As the duration of the research increased, the quality of the acne lesion improved. This study has determined that the microdermabrasion effect of a spongilla spicule enhances the pore keratinization of acne skin and impedes the proliferation of skin bacteria (Propionibacterium acnes)[17].
Numerous studies have been conducted to enhance the penetration of drugs and cosmetics through the epidermis. Microneedles have been developed in a variety of forms for transdermal drug delivery, for instance. Also, micro-needle patches have been employed in recent years to enhance drug delivery, increase skin permeability, and for various cosmetic purposes. Inadequate skin penetration and distress are common issues with this technology, often resulting in low compliance [8,19,20]. The topical application of spongilla spicules delivers hydrophilic biomacromolecules to the skin in a painless, effective, and sustained manner. This method may also create new opportunities for the transdermal/dermal delivery of a diverse array of therapeutics [14,15]. Research is still being conducted on the use of Spongilla spicule or microneedling treatments in conjunction with other therapies. Although certain combinations may increase effectiveness, there is a higher chance of negative side effects. Adjunctive treatments should be considered with clinical judgment, customized to meet the needs of each patient, and carried out under expert supervision [18].
The application strategies of spongilla spicules treatment could be adjusted to optimize the balance between efficacy and safety in accordance with the diseases targeted and treatment requirements. Spongilla spicules' topical application is a prospective platform technology for various medical and cosmetic applications [14]. Conducting further research with a larger sample size and long-term follow-ups is imperative.
Conclusion
The hybrid peel, which contained 99% spongilla spicules and 0.5% beta hydroxy acids, effectively treated acne-prone skin.
Conflict of interest:
The authors declare no conflict of interest.
Patient Consent
The patient provided written informed consent before receiving any study-related procedures and to use their image or clinical history for publication.
Funding
The authors personally fund this study.
Authors contributions
TH, SL: conceptualization. TH, SL: methodology. TH, SL: investigation and resources. TH, SL: Original draft of the manuscript. TH, SL: visualization. TH, SL: validation, review, and manuscript editing. The final manuscript was read
References
Calvisi, L., (2021). Efficacy of a combined chemical peel and topical salicylic acid-based gel combination in the treatment of active acne. J Cosmet Dermatol; 20: 2–6. View
Chen, X., Wang, S., Yang, M., Li, L., (2018). Chemical peels for acne vulgaris: A systematic review of randomised controlled trials. BMJ Open; 8. View
Măgerușan Șoimița, E., Hancu, G., Rusu, A. (2023). A Comprehensive Bibliographic Review Concerning the Efficacy of Organic Acids for Chemical Peels Treating Acne Vulgaris. Molecules. 28. View
Chilicka, K., Rogowska, A. M., Szyguła, R., Dzieńdziora Urbińska, I., Taradaj, J., (2020). A comparison of the effectiveness of azelaic and pyruvic acid peels in the treatment of female adult acne: a randomized controlled trial. Sci Rep; 10. View
Castillo, D. E., Keri, J. E., (2018). Chemical peels in the treatment of acne: Patient selection and perspectives. Clin Cosmet Investig Dermatol; 11: 365–372. View
Zhao, J., Wang, Y., Jiang, L., Mu, Y. Z., (2020). The application of skin care product in acne treatment. Dermatol Ther. 33. View
Habeshian, K. A., Cohen, B. A., (2020). Current issues in the treatment of acne vulgaris. Pediatrics; 145. View
Zhang, J., Lin, P., Guo, C., Ma, C., Liu, Y., Wang, Y., et al. (2023). Effects and safety of fire needle adjuvant chemical peels therapy in acne vulgaris: a systematic review and meta-analysis. Journal of Dermatological Treatment. 34. View
Draghici, C-C., Miulescu, R-G., Petca, R-C., Petca, A., Dumitrașcu, M., Șandru, F., (2021). Teratogenic effect of isotretinoin in both fertile females and males (Review). Exp Ther Med; 21. View
Chandrashekar, Vadlamudi, S. L., Shenoy, C. (2021). Safety of Performing Superficial Chemical Peels in Patients on Oral Isotretinoin for Acne and Acne-Induced Pigmentation. Jpurnal of Clinical and Aesthetic Dermatology; 14 (11). View
Kontochristopoulos, G., Platsidaki, E. (2017). Chemical peels in active acne and acne scars. Clin Dermatol; 35: 179–182. View
Al-Hamamy, H. R., AL-Dhalimi, M. A., Abtan, A. F. (2021). Evaluation of treatment of acne scars with 25% trichloroacetic acid chemical peel followed by manual dermasanding. J Cosmet Dermatol; 20: 1750–1755. View
Łukowiak, M., Van Soest, R., Klautau, M., Pérez, T., Pisera, A., Tabachnick, K. (2022). The terminology of sponge spicules. J Morphol. 283: 1517–1545. View
Zhang, S., Ou, H., Liu, C., Zhang, Y., Mitragotri, S., Wang, D. et al. (2017). Skin Delivery of Hydrophilic Biomacromolecules Using Marine Sponge Spicules. Mol Pharm; 14: 3188–3200.
Zhang, C., Duan, J., Huang, Y., Chen, M., (2021). Enhanced Skin Delivery of Therapeutic Peptides Using Spicule-Based Topical Delivery Systems. Pharmaceutics. View
Tansathien, K., Suriyaaumporn, P., Charoenputtakhun, P., Ngawhirunpat, T., Opanasopit, P., Rangsimawong, W. , (2019). Development of Sponge Microspicule Cream as a Transdermal Delivery System for Protein and Growth Factors from Deer Antler Velvet Extract. View
Lee, C. H., Choi, B. S. (2019). Improvement of Facial Acne on Skin with 3% Spicule. Asian Journal of Beauty and Cosmetology; 17: 397–410. View
Măgerușan Șoimița, E., Hancu, G., Rusu, A. (2023). A Comprehensive Bibliographic Review Concerning the Efficacy of Organic Acids for Chemical Peels Treating Acne Vulgaris. Molecules. 28. View
Ha, J. M., Lim, C. A., Han, K., Ha, J. C., Lee, H. E., Lee, Y., et al. (2017). The effect of micro-spicule containing epidermal growth factor on periocular wrinkles. Ann Dermatol; 29: 187 193.
Ishfaq, F., Shah, R., Sharif, S., Waqas, N., Jamgochian, M., Rao, B., (2022). A Comparison of Microneedling versus Glycolic Acid Chemical Peel for the Treatment of Acne Scarring. Journal of Clinical and Aesthetic Dermatology; 15 (6). View

