Journal of Public Health Issues and Practices Volume 5 (2021), Article ID: JPHIP-175
https://doi.org/10.33790/jphip1100175Review Article
Narrowing of the Racial Gap In Opioid-Involved Deaths: Implications for Public Health Policy and Practice
Peter J. Fos, Ph.D., D.D.S., M.P.H1*,Peggy A. Honoré, D.H.A2,Katrina P. Kellum, D.N.P3
1*Professor of Health Sciences and Research Professor, Minority Health and Health Disparities Research Cente, Dillard University, USA.
2Professor, LSU Health Sciences Center, School of Public Health & School of Medicine, Louisiana State University, USA.
3Assistant Professor, College of Nursing, Dillard University, USA.
Corresponding Author Details: Peter J. Fos, Ph.D., D.D.S., M.P.H. Professor of Health Sciences and Research Professor, Minority Health and Health Disparities Research Center, Dillard University, 2601 Gentilly Blvd., New Orleans, LA 70122, USA. E-mail: 2d0003@mail.tmh.org.tw
Received date: 15th December, 2020
Accepted date: 18th January, 2021
Published date: 20th January, 2021
Citation: Fos, P. J., Honoré, P.A., & Kellum, K.P. (2021). Trajectories Matching for Characterizing Patient’s Behavior in Policy Evaluation. J Pub Health Issue Pract 5(1): 175.
Copyright: ©2021, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Objectives: Opioid overdose death rates in the United States has been increasing over the past several years. This increasing trend has been seen in states across the country. Previous studies have highlighted that opioid-involved deaths have occurred mostly in non-Hispanic Whites. The objectives of this study were to (1) compare opioid deaths death trends in U.S. to a state, Louisiana, (2) compare opioid death trends in Louisiana urban and suburban areas, and (3) evaluate changes in the overall trends, as well as across race and gender, that may affect public health policy and practice.
Methods: Data were abstracted from secondary data sources, including the Louisiana Opioid Data and Surveillance System. Trends in opioid-involved deaths, drug-induced deaths, and opioid prescription by prescriber location were determined in the U.S. and Louisiana.
Results: The increasing trends in age-adjusted rate of opioidinvolved deaths in Louisiana has mimicked what has occurred in the United States. The crude rates of drug-induced deaths in the U.S. and Louisiana exhibited an increasing trend. However, the trend in opioid prescriptions had a decreasing trend. The crude rates were higher in non-Hispanic Whites, as well as in males. This trend is changing with the gap between opioid-involved deaths among non- Hispanic Whites and non-Hispanic Blacks narrowing, as well as between males and females.
Conclusions: The study confirmed that the opioid epidemic in the U.S. is also occurring in Louisiana. The changing trends in the rate of opioid-involved deaths indicate anarrowing of the gap between non- Hispanic Whites and non-Hispanic Blacks, and males and females, and that public health practice and health policy must address the future needs to mitigate the opioid epidemic.
Keywords: Opioids, Health Disparities, Minority Populations, Death Trends, Public Health Practice
Introduction
Opioid usage in the United States is an epidemic and a public health emergency. The increase in opioid usage began in the 1990’s when the Joint Commission on Accreditation of Health Care Organizations (JCAHO) identified pain management as a primary medical disorder. This coincided with OxyContin’s approval by the Food and Drug Administration with the assurance of manufacturers that it was not addictive [1]. OxyContin provided significant pain relief for patients but was intertwined with increased prescription and subsequent abuse by patients [2]. The opioid epidemic can be best described in three waves. The first wave started in the late 1990’s with increased prescribing of these type of opioids for pain management followed by a second wave in 2010 involving increased heroin abuse and synthetic opioid compounds. The third wave started in 2013 with the introduction of synthetic compounds such as fentanyl [3].
Unintended opioid overdose mortality rates in the United States has been increasing over the past several years. The increase has been significantly more evident in young and middle-aged adults [4]. From 2011 to 2016, opioid-involved deaths in North America increased from 33.3 deaths per million population to 130.7 deaths per million population. The most rapid increase in opioid overdose deaths occurred in the 25-35 age group, with men accounting for 67.5% of deaths [5]. Given this age group and increasing mortality rates there is an associated concern of potential years of life lost. It has been shown that opioid-dependent use was directly associated with almost one million disability-adjusted life years annually and nearly one million years of life lost in people under the age of 65 years [6].
The increase in drug overdose deaths has been seen among women [7]. The increase among women has been most significant in the 45- 54 and 55-64 age groups [8]. Opioid-involved deaths between 1999 and 2017 increased among women in the 30-64 years age group, particularly among women 55-64 years of age group [9]. From 1999 to 2017 the crude death rate from drug overdose among women aged 30-64 years increased from 6.7 deaths per 100,000 to 24.3 deaths per 100,000. Overall, there was a 1,643% increase in opioid-involved deaths [10].
The increase in opioid-involved deaths have occurred across all segments of the United States population. States with high prescription opioid dosages are at a higher risk for opioid overdose, which is a major cause ofopioid-involved deaths [11,12]. The risk is catalyzed by long-term prescribed opioid usage, especially after release from prison, completion of an inpatient drug rehabilitation program, and discharge from hospitalization [13]. Veteran populations who utilized the Veterans Health Administration have shown an increasing rate of opioid-involved deaths. From 2010 to 2016 the rate of opioid overdose among veterans increased from 14.47 per 100,000 person years to 21.08 per 100,000 person years [14].
The increase in opioid-involved deaths has been more pronounced in non-Hispanic Whites [15]. Recent studies have illustrated the increase in opioid-involved deaths in non-Hispanics Whites, especially in younger non-Hispanic Whites, may now be seen in non-Hispanic Blacks, as well as females, because of the use of drug combinations and synthetic-opioids, such as fentanyl [16-17]. During the past decade, especially since 2013, synthetic opioid usage has been the major cause of increases in opioid-involved deaths [18]. With the increase use of synthetic opioids the racial distribution of opioid-involved deaths began to change, especially in non-Hispanic Blacks [19-20]. Metropolitan areas, including fringe metropolitan areas, experienced a precipitous increase in opioid-involved deaths since 2013 [21-22].
This paper describes the study of the comparison of opioid deaths in Louisiana with the U.S. during a five-year period, 2014 through 2018. The comparison intended to determine whether the trends in Louisiana resembled what has occurred nationally. Additionally, an objective of the study was to evaluate whether the changing trend in opioid-involved deaths in non-Hispanic Blacks and females was occurring in Louisiana, as well.
Methods
The study focused on retrospective evaluation of data from several sources, including the Centers of Disease Control and Prevention and the Louisiana Opioid Data and Surveillance System [23]. The source of mortality data source was death certificates, using coding according to the Tenth Revision of the International Classification of Diseases (ICD-10) [24]. A death related to opioid usage and overdose are ICD-10 codes T40.0, T40.1, T40.2, T40.3, T40.4, and T40.6. The time-period selected was 2014 through 2018 to coincide with the point of proliferation of opioid usage and associated opioid-involved deaths. Additionally, an urban and suburban area in Louisiana were selected: Orleans and Jefferson Parishes. These parishes comprise most of the Greater New Orleans area, and have relatively large populations with diverse demographics.
Trends in the rates of opioid-involved deaths, drug-induced deaths, and opioid prescription by prescriber location were determined. Crude rates were calculated using the U.S. Census July 2019 population estimates [25]. Trends in opioid-involved deaths by race and gender were studied. Additionally, means and standard deviations were calculated using SPSS version 26.
The Mann-Kendall (M-K) statistical test, using Microsoft Excel, was used to evaluate trends. The M-K test has been previously used in health care to study blood stream infections, influenza seasonality, and cancer-associated complications [26-28].The M-K test is a nonparametric test used to statistically assess if there is a monotonic increasing or decreasing trend in a data set, over time. The null hypothesis is that there is no trend in the data, and the alternate hypothesis is that there was an increasing or decreasing trend. A no trend indicates that the data points are not correlated. A stable trend indicates that there have not been any changes, over time. The M-K test statistic, S, was calculated, as well as the coefficient of variation and p-values using a .05 level of significance [29].
Results
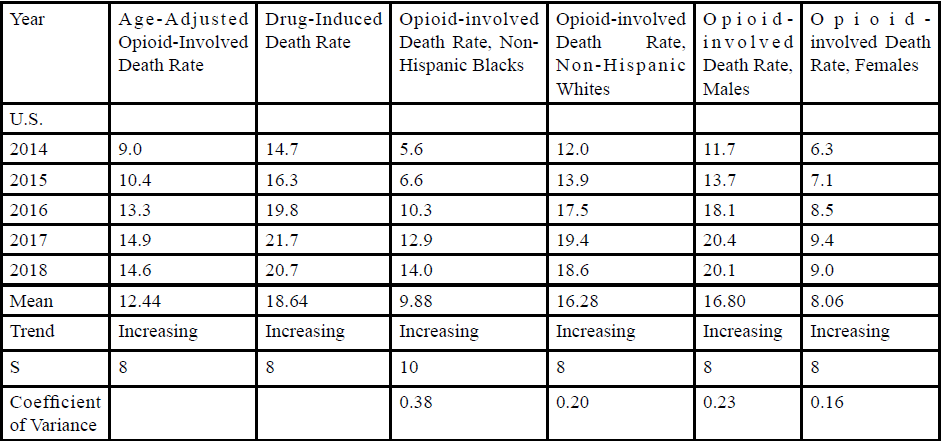
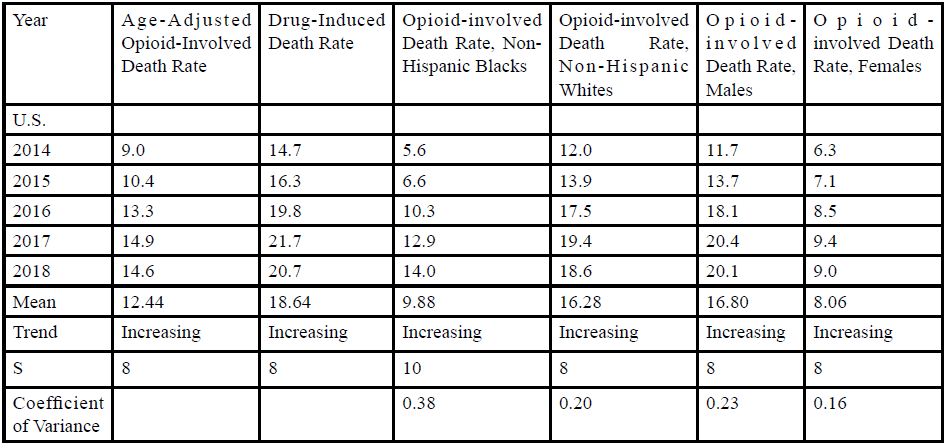
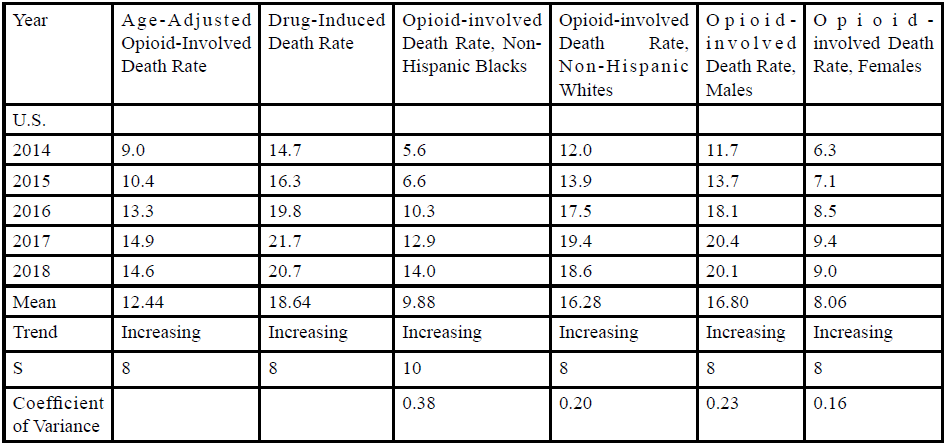
Overall, the opioid-involved death rates in U.S. and Louisiana have increased from 2014 through 2018 (Table 1). In the U.S.,the age-adjusted opioid-involved death rate in 2014 was 9.0 deaths per 100,000 population compared to 14.6 deaths per 100,000 in 2018. The M-K test identified an increasing trend, with a coefficient of variation of 0.21 and p-value <.05. In Louisiana, the age-adjusted opioid-involved mortality rate in 2014 was 5.43 deaths per 100,000, an increase to 7.28 deaths per 100,000 in 2018. This represents an 82% increase. The M-K test identified an increasing trend, with a coefficient of variation of 0.25 and a p-value <.01.
The drug-induced death rate in the U.S. and Louisiana showed a statistically significant increasing trend. The rate of increase was 41% in the U.S. and 49% in Louisiana. The age-adjusted druginduced death rate in the U.S. in 2014 was 14.7 deaths per 100,000 and 20.7 deaths per 100,000 in 2018. In Louisiana, the rate was 19.30 deaths per 100,000 and increased to 24.09 deaths per 100,000 in 2018. Trends in drug-induced death rates in the U.S. and Louisiana were increasing, with coefficients of variation equal to 0.21 and 0.16, respectively.
Opioid-involved death rates across races in the U.S. has shown that non-Hispanic Whites have had higher rates than non-Hispanic Blacks (Table 1). The trends increased for both races, with non- Hispanic Blacks experiencing a greater increase than non-Hispanic Whites. The opioid-involved death rate in non-Hispanic Blacks was 5.6 deaths per 100,000 in 2014 and 14.0 deaths per 100,000 in 2018. In non-Hispanic Whites the opioid-involved death rate increased from 12.0 deaths per 100,000 in 2014 to 18.6 deaths per 100,000 in 2018. This increasing trend was also seen in Louisiana. The non- Hispanic Whites mean death rate was 7.22 per 100,000 in 2014 and 12.04 deaths per 100,000 in 2018. The non-Hispanic Black death rate increased from 2.17 deaths per 100,000 to 5.20 deaths per 100,000 from 2014 through 2018. The trends in the U.S. for non-Hispanic Whites and Blacks were increasing, with coefficients of variations of 0.20 and 0.38, respectively. The trends in Louisiana were also increasing, but the trend in non-Hispanic Blacks was not statistically significant.
Opioid-involved deaths are more prevalent in males than females in the U.S. The opioid-involved death rate for males increased 72% from 2014 through 2018. This was an increasing trend, with a coefficient of variation of 0.23 and a p-value <.05. The opioid-involved death rate for females was 6.3 per 100,000 in 2014 and 9.0 deaths per 100,000 in 2018, a 43% increase. This trend was increasing with a coefficient of variation equal to 0.16 and a p-value <.05. The increase in opioid-involved death rates was greater in males than females.
The opioid-involved death rate for males in Louisiana increased 59% from 2014 through 2018, an increasing rate with a coefficient of variation equal to 0.22. The death rate for females increased 83% from 2.63 deaths per 100,000 in 2014 to 4.82 deaths per 100,000 in 2018, an increasing trend with a coefficient of variation of 0.23. The opioid-involved death rate in males was 2.6 times greater than for females in Louisiana. However, the opioid-involved death rate in males increased 58% during the study period, compared to an 82% increase among females through 2018.
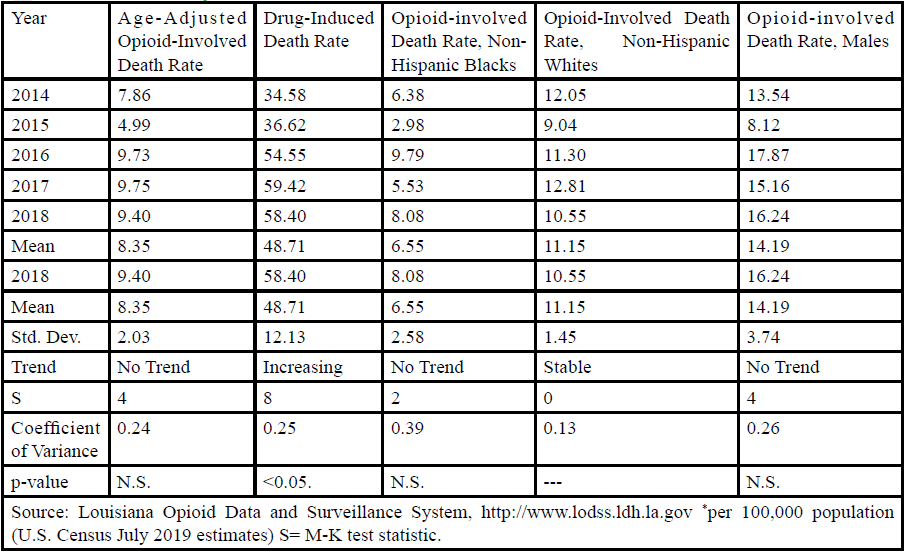
The City of New Orleans comprises Orleans Parish, and has a population of 390,144; 60.2% non-Hispanic Blacks and 34.0% non- Hispanic Whites. Jefferson Parish abuts New Orleans and can be considered a suburban area. Jefferson Parish has 423,493 residents, 62.9% non-Hispanics Whites and 28.0% non-Hispanic Blacks, which resembles the racial distribution of Louisiana. Table 2 shows age-adjusted opioid-involved death rates, drug-induced death rates, and the opioid-involved death rates among non-Hispanic Whites a Blacks in Orleans Parish.
The trends in Orleans Parish were similar as in the U.S. and Louisiana. The drug-induced death rate increased from 34.58 deaths per 100,000 to 58.40 deaths per 100,000 in 2018. This trend is increasing, with a coefficient of variation of 0.25 and a p-value <.05. Opioid-involved death rates in non-Hispanic Blacks slightly increased and the M-K test found no trend. Opioid-involved death rates in non-Hispanic Whites decreased from 12.05 deaths per 100,000 in 2014 to 10.55 deaths per 100,000 in 2018. This represents a stable trend, indicates that there was no significant change in death rates over the study period.
Jefferson Parish had a higher age-adjusted opioid-involved death rate than the state, Orleans Parish, and the U.S. (Table 3). The age adjusted opioid-involved death rate was 14.87 per 100,000 in 2014 and 29.16 deaths per 100,000 in 2018. This represented a statistically significant increasing trend in opioid-involved death rates. The drug induced death rate was also higher in Jefferson Parish. The mean drug-induced death rate was 36.76 deaths per 100,000 population and the standard deviation is 5.25. The drug-induced death rate increased nearly 70%, from 34.58 deaths per 100,000 in 2014 and 58.40 deaths per 100,000 in 2018. This represents an increasing trend, with a coefficient of variation equal to 0.25.
The opioid-involved death rate in Jefferson Parish among non-Hispanic Blacks doubled from 2014 through 2018, from 8.26 deaths per 100,000 to 16.52 deaths per 100,000, an increasing trend. Among non-Hispanic Whites the opioid-involved death rate in 2014 was 20.89 deaths per 100,000 and 35.76 deaths per 100,000 in 2018,an increasing trend with a coefficient of variation of 0.26 and a p-value <.05. This represents a 72% increase, less than the increasing trend among non-Hispanic Blacks. The opioid-involved death rate among males increased from 23.03 deaths per 100,000 in 2014 to 42.69 deaths per 100,000 in 2018. Among females, the opioid-involved death rate in 2014 was 7.14 deaths per 100,000 and 16.07 deaths per 100,000 in 2018. The trends are increasing among males and females, with coefficients of variation of 0.30 for both genders.
Table 4 presents the crude rate, per 100 population, of opioid prescriptions. During the study period the mean crude rate in the U.S. was 64.62 opioid prescriptions per 100 population. In Louisiana, the mean crude rate was 109.0 per 100. In the two metropolitan areas, the crude rate was 137.2 per 100 in Jefferson Parish and 89.8 per 100 in Orleans Parish. The crude rate in the U.S. decreased from 75.6 prescriptions per 100 to 51.4 prescriptions per 100.
Louisiana also experienced a decrease, from 118 to 96 prescriptions per 100. Jefferson Parish saw a decrease from 145 to 121 prescriptions per 100, with the decrease in Orleans Parish from 103 to 68 prescriptions per 100. The decreasing trends were statistically significant in the U.S., Louisiana, Jefferson Parish, and Orleans Parish.
Discussion
As has been previously reported, the United States has experienced an increasing trend in the rate of opioid-involved deaths, as has been seen in Louisiana over the past several years [30]. The third wave with the use of synthetic opioids, such as fentanyl and fentanyl analogs, became very prevalent the year before the study period began. Studies have shown that inadvertent contamination of heroin has resulted in a 50 times more potent fentanyl. This is likely a contributing factor in the increase in opioid related deaths. Additionally, research suggests that combination of fentanyl and heroin use is occurring at a younger age and with riskier behaviors such as combining with other drugs, more frequent use, and higher doses [32].
Opioid usage and opioid-involved death rates for both metropolitan and fringe metropolitan areas have been increasing for many years [32]. The opioid-involved death rate increased 62% in the U.S. and Louisiana had a slightly greater increase of 82 percent. The urban and suburban areas had statistically significant trends, and the rate nearly doubled in the fringe suburban area.
Drug-induced death rates increased in all study areas. The increase was 41% in the U.S. and 48% in Louisiana. The urban area’s (Orleans Parish) rate increased 69%, which was double the rate increase in Jefferson Parish. The increasing trends in all study areas were statistically significant. The difference in the rate increase between Orleans and Jefferson Parish may be an indication that an increasing proportion of non-Hispanic Blacks are overdosing and dying because of opioid usage.
When reviewing racial differences in the opioid epidemic it is interesting to observe the opioid-involved death rates among non- Hispanic Whites and non-Hispanic Blacks. The percent increase in opioid-involved death rates among non-Hispanic Blacks was the same in the U.S. and Louisiana. The increase was 150% in the U.S. and 140% in Louisiana. Among non-Hispanic Whites the increase in opioid-involved death rates in Louisiana was greater than in the U.S. However, the increase in non-Hispanic Blacks was three times greater in the U.S. compared to non-Hispanic Whites. This was also seen in Louisiana where the increase in opioid-involved death rates in non-Hispanic Blacks was double the increase in non-Hispanic Whites.
The increase in the opioid-involved death rate among non-Hispanic Blacks was greater than non-Hispanic Whites in Orleans Parish. In fact, the death rate among non-Hispanic Whites decreased from 2014 through 2018. This similar trend was observed in Jefferson Parish where the opioid-involved death rate was double the rate in non- Hispanic Whites. The death rate in non-Hispanic Whites increased, but to lesser extent than among non-Hispanic Blacks.
There are many reasons that may contribute to the increase in opioid involved death rate in non- Hispanic Blacks. Non-Hispanic Blacks in the U.S. are overall undertreated for pain in comparison to non-Hispanic Whites. Additionally, non-Hispanics Blacks are given lower quantities of pain medicine for similar reports of pain [33]. Pain medication is less likely to be prescribed to non-White minorities than their White counterparts. This may lead to possible insufficient treatment of pain [34]. This may account for the increase in deaths in non-Hispanic Whites during the first wave of the opioid epidemic since they were more likely to be prescribed opioids. It is also possible that non-Hispanic Blacks are more likely to go to illicit forms of pain relief such as heroin and fentanyl when the medical community do not adequately address their pain management needs.
The trend in gender differences trends has begun to change. The opioid epidemic is predominantly affecting males, but more and more females are using, overdosing, and dying from opioids. In the U.S., the opioid-involved death rate increase continues to be greater in males. But, the gap in differences is beginning to narrow. Interestingly, in Louisiana the increase in the opioid-involved death rate in females was greater than for males. Males in Louisiana had a mean opioid-involved death rate that was 3 times greater than in females, but on the state-level the increase in death rates among females has nearly double the rate in males. In Jefferson Parish the opioid-involved death rate was more than 3 times higher in males, but the increase in opioid-involved death rates among females was greater. Due to low number, data on the opioid-involved death rates in females was not available for Orleans Parish.
Research has been done on the variation of prescribing patterns among primary care providers on the county level [35]. Studies have shown that the rate of opioid prescriptions by prescriber has decreased over the past five years. In the U.S., a 32% decrease has been observed, and a 19% decrease in Louisiana. The rate of prescriptions decreased in both Orleans and Jefferson Parish. These decreasing trends are statistically significant and a good sign in battling the opioid epidemic, and hopefully decreasing opioidinvolved death rates. However, it is telling that in 2018, in Louisiana and Jefferson Parish, after decreasing for four years, the crude rate per 100 population was more than one opioid prescription for every person in the population. This illustrates that work needs to be done to fully address the opioid epidemic in the U.S.
This study confirms the need to continue existing policies and practices to combat the opioid epidemic, as well as to create new ones. Policy recommendations include the following: a) strengthen state Prescription Drug Monitoring Program (PDMP) policies to increase timely (e.g., real-time) reporting by pharmacies and mandate proactive routine use by health care providers; b) strengthen federal and state policies and funding to increase workforce credentialing for substance abuse counseling with specific attention to ensure that minority and female populations participate in such training opportunities; c) establish policies for enhanced public health agency surveillance through data monitoring that includes analysis by race, ethnicity, and gender, as well as reporting to appropriate health officials any potential patterns in the population of prescription drug misuses; d) implement policies, whether government or institutional based for the education of health care providers on implicit biases when treating patients presenting with complaints of pain.
Conclusions
Over the past several years the increase in the rate of opioidinvolved deaths trends among non-Hispanic Blacks has been greater than non-Hispanic Whites, indicating that the gap is narrowing. As this continues, it is imperative to address opioid abuse in both races. To a lesser extent, the narrowing of the gap between males and females was seen in Louisiana, which may be considered what will occur in the future across the U.S.
On a larger scale, the public health system needs to be aware of what the future holds, in order to appropriately address the opioid epidemic. Policies, prevention interventions, and programs that aid with treatment and recovery must be targeted to non-Hispanic Blacks, as well as non-Hispanic Whites. While crude rates of opioid prescription per 100 population have decreased there is still much work to be done to mitigate opioid-related deaths in the U.S. and Louisiana.
Acknowledgements:
Research reported in this article was supported, in part, by the National Institute of Minority Health and Health Disparities of the National Institute of Health under grant number S21MD1007136.
Conflict of interests:
The authors declare no conflict of interest.
References
Chhabra, N., &, Leikin, J.B. (2017). The Joint Commission and the opioid epidemic. JAMA, 318(1):91-92. doi:10.1001/ jama.2017.6694.View
Coplan, P.M., Chilcoat, H.D., Bulter, S.F., Sellers, E.M., Kadakia, A., Harikrishnan, V., …, Dart, R.C. (2017). The effect of an abuse-deterrent opioid reformulation (OxyContin) on opioid abuse-related outcomes in postmarketing setting. ClinPharmacolTher, 100(3):275-286. doi:10.1002/cpt.390.View
Ciccarone, D. (2019). The triple wave epidemic: Supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy, 71:183-188. doi:10.1016/j.drugpo.2019.01.010.View
Office of the Assistant Secretary for Planning and Evaluation. Opioid abuse in the U.S. and HHS actions to address opioiddrug related overdoses and deaths.https://aspe.hhs.gov/basicreport/ opioid-abuse-us-and-hhs-actions-address-opioid-drugrelated- overdoses-and-deaths. Accessed on March 10, 2020.View
Rudd, R.A., Seth, P., David, F., & Scholl, L. (2016). Increases in drug and opioid-involved overdose deaths – United States, 2010-2015. MMWR, 65(5051):1445-1452. doi:10.15585/ mmwr.mm6555051e1.View
Degenhardt, L., Charlson, F., Mathers, B., Hall, W.D., Flaxman, A.D., Johns, N., & Vos, T. (2014). The global epidemiology and burden of opioid dependence: results from the global burden of disease 2010 study. Addiction, 109(8):1320-133. doi:10.111/ add.12551.View
Centers for Disease Control and Prevention. (2011). Vital signs: overdoses of prescription opioid pain relievers – United States, 1999-2008. MMWR, 60(43):1487-1492. https://www.cdc.gov/ mmwr/preview/mmwrhtml/mm6043a4.htm.View
Mazure, C.M., & Fiellin, D.A. (2018). Women and opioids: something different is happening here. Lancet, 392:9-11. doi:10.1016.S0140-6736(18)31203-0.View
Centers for Disease Control and Prevention (2013). Vital signs: overdoses of prescription opioid pain relievers and other drugs among women – United States, 1999-2010. MMWR, 62(26):537- 542. https://www.cdc.gov/preview/mmwrhtml/mm6226a3.htm.View
VanHouten, J.P., Rudd, R.A., Ballesteros, M.F., & Mack, K,A. (2019). Drug overdose deaths among women aged 30-64 years – United States, 1999-2017. MMWR, 68(1):1-5. doi:10.15585/ mmwr.mm6801a1.View
Dasgupta, N., Funk, M.L., Proescholdbell, S., Hirsch, A., Ribisl, K.M., & Marshall, S. (2016). Cohort study of the impact of highdose opioid analgesics on overdose mortality. Pain Med,17(1): 85-98. doi:10.111/pme.12907View
Gomes,T., Mamdani, M.M., Dhalla, I.A., Paterson, J.M., & Juurlink, D.N. (2011). Opioid dose for chronic pain and drugrelated mortality in patients with nonmalignant pain. Arch Intern Med,171(7): 686-691. doi:10.1001/archintermed.2001.117.View
Binswanger, I.A., Blatchford, P.J., Mueller, S.R., & Stern, M.F. (2013). Mortality after prison release: Opioid overdose and other cause of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med, 159(9):592-600. doi:10.7326/0003- 4819-159-9-201311050-00005.View
Strang, J., McCambridge, J., Best, D., Beswick, T., Beam, J., Rees, S., & Gossop, M. (2003). Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow-up study. BMJ, 326(7396):959-960. doi:10.1136/bmj.326.7336.959.View
Rudd, R.A., Aleshire, N., Zibbell, J.E., & Gladden, R.M. (2016). Increases in drug and opioid overdose deaths: United States, 2000-2014. MMWR, 64(50): 1378-1382.https://www.cdc.gov/ mmwr/preview/mmwr/mmwrhtml/mm645013.htm.View
Dart, R.C., Surratt, H.L., Cicero TJ, Parrino, M.W., Severtson, S.G., Bucher-Bartelson, B., & Green, J.L. (2015). Trends in opioid analgesic abuse and mortality in the United States. N Eng J Med, 372(3):241-248.doi:10.1056/NEJMsa1406143.View
Alexander, M.J., Kiang, M.V., & Barbieri, M. (2018). Trends in Black and White opioid mortality in the United States, 1979-2015. Epidemiol, 29(5):707-715. doi: 10.1097/ EDE.0000000000000858.View
Jones, C.M., Einstein, E.B., & Compton, W.M. (2018), Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. JAMA, 319:1819-21. doi:10.1001/ jama.2018.2844.View
Paulozzi, L.J., Budnitz, D.S., & Xi, Y. (2006). Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf, 15:618-627.doi:10.1002/pds.1276.View
Shiels, M.S., Freedman, N.D., Thomas, D., & Berrington de Gonzalez, A. (2018). Trends in U.S. drug overdose deaths in non-Hispanic black, Hispanic, and non-Hispanic white persons, 2000-2015. Ann Intern Med,168:453-5. doi:10.7326/M17-1812.View
Mack, K.A., Jones, C.M., & Ballesteros, M.F. (2017). Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas – United States. MMWR SurveillSumm, 66(No. SS-19). Doi:10.15585/mmwr.ss661a1.View
Colon-Berezin, C., Nolan, M.L., Blackman-Forshay, J., & Paone, D. (2019). Overdose deaths involving fentanyl and fentanyl-analogs – New York City, 2000-2017. MMWR, 68:37- 40. doi:10.15585/mmwr.mm6802a3.View
Louisiana Department of Health. Louisiana Opioid Data and Surveillance System. http:///ldh.la.gov/index.cfm/page/3192. Accessed October 1, 2020.
World Health Organization. International Classification of Diseases; Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death: Tenth Revision (ICD-10). Geneva, Switzerland, WHO. http://apps.who.int/ classifications/icd10/browse/2016/en.View
United States Census Bureau. U.S. Census Bureau Quickfacts. https://www.census.gov/quickfacts. Accessed October 1, 2020.
Zipursky, A.R., Yoon, E.W., Emberley, J., Bertelle, V., Kanungo, J., Lee, S.K., & Shah, P.S. (2019). Central-line-associated blood stream infections and non-central-line associated blood stream infection surveillance in Canadian tertiary neonatal intensive care units. J Pediatr, 208:176-182e6. doi:10.1016/j. peds.2019.12.011.
Moa, A.M., Adam, D.C., & MacIntyre, C.R. (2019). Interseasonality of influenza in Australia. Influenza Other Respir Viruses, 13(5):459-464. doi:10.111/irv.12642.View
Almohammed, O.A., Lai, L., Khanfar, N.M.,Bleidt, B., & Aljadhey, H. (2019). Trends in cancer-associated venous thromboembolism (VTE) in the United States (2005-2014). Thromb Res, 182:110-115. doi:10.1016/j.thromres.2019.08.013View
Aziz, J.J., Ling, M, Rifai, H.S., Newell, C.J.,& Gonzales, J.R. (2005). MAROS: a decision support system for optimizing monitoring plans. Groundwater, 41(3): 355-367. doi:10.111/j.1745-6584.2003.tb02605.x.View
School, L., Seth, P., Kariisa, M., Wilson, N., & Baldwin, G. (2019). Drug and opioid-involved overdose deaths, United States, 2013- 2017. MMWR, 67(51-52):1419-1427. doi:10.15585/mmwr. mm.67515e1.View
Dowell, D., Noonan, R.K., & Houry, D. (2017). Underlying factors in drug overdose deaths. JAMA, 318(23):2295-2296. doi:/10.1001/jama.2017.15971.View
Garcia, M.C., Hellig, C.M., Lee, S.H., Faul, M., Guy, G., Iademarco, M.F,…,& Gray, J. (2019). Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using electronic health record system – United States, 2014-2017. MMWR, 68(2):25-30. doi:10.15585/mmwr. mm6802a1.View
Hoffman, K.M.,Trawalter, S., Axt, J..R, & Oliver, M.N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceeding of the National Academy of Sciences of the United States, 113(16):4296-4301. doi:10.1073/ pnas.1516047113.View
Santoro, T.N., & Santoro, J.D. (2018). Racial bias in the US opioid epidemic: A review of the history of systemic bias and implications for care. Cureus, 10(12):e3733. doi:10.7759/ cureus.3733.View
Guy, G.P., Zhang, K., Bohm, M.K., Losby, J., Lewis, B., Young, R., …, Dowell, D. (2017). Vital signs: Changes in opioid prescribing in the United States, 2006-2015. MMWR, 66(26):697-704. doi:10.15585/mmwr.mm6626a4.View