Journal of Public Health Issues and Practices Volume 9 (2025), Article ID: JPHIP-243
https://doi.org/10.33790/jphip1100243Research Article
Exploring the Effectiveness of Lavender Aromatherapy on Improving Sleep Quality Among Nurses
I-Ju Pan, Yi-Hui Liu*, and Si-Yi Yang
Department of Nursing, I-Shou University, No.8, Yida Rd., Jiaosu Village Yanchao District, Kaohsiung City 82445, Taiwan.
Corresponding Author Details: Yi-Hui Liu, Assistant Professor, Department of Nursing, I-Shou University, No.8, Yida Rd., Jiaosu Village Yanchao District, Kaohsiung City 82445, Taiwan.
Received date: 15th July, 2025
Accepted date: 28th August, 2025
Published date: 30th August, 2025
Citation: Pan, I. J., Liu, Y. H., & Yang, S.Y., (2025). Exploring the Effectiveness of Lavender Aromatherapy on Improving Sleep Quality Among Nurses. J Pub Health Issue Pract 9(2): 243.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: This study examined the effectiveness of an 8-week lavender aromatherapy intervention on improving sleep quality and modulating autonomic nervous system (ANS) activity among nurses working rotating shifts.
Methods: A quasi-experimental study was conducted in a hospital in southern Taiwan. Ninety-five nurses were randomly assigned to a lavender aromatherapy group (n=48) or a control group (n=47). The intervention group applied lavender essential oil to pillowcases nightly, while controls maintained usual routines. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) at baseline, week 4, and week 8, and physiological indicators of ANS activity were monitored weekly.
Results: Lavender aromatherapy significantly improved subjective sleep quality compared to controls, as reflected by reduced PSQI scores over time. Physiological outcomes showed consistent improvements, including reductions in blood pressure and heart rate, alongside increased heart rate variability and parasympathetic activity, indicating enhanced autonomic balance.
Conclusion: Lavender aromatherapy effectively improved sleep quality and ANS regulation among shift-working nurses. By lowering blood pressure, heart rate, and sympathetic activity while enhancing parasympathetic tone, this simple, non-pharmacological intervention demonstrates potential for mitigating sleep disturbances and stress-related cardiovascular risks in healthcare professionals. Incorporating lavender aromatherapy into workplace wellness initiatives may support the health and resilience of nursing staff. Future studies should explore combined complementary therapies and evaluate long-term benefits.
Introduction
In modern society, nurses play an indispensable role. They are responsible for patient care, the provision of medical services, and maintaining the operation of healthcare facilities. However, this work often comes with significant stress and heavy workloads, particularly in busy hospitals and emergency departments. Nurses frequently face high-pressure work environments, the need to respond to unexpected situations at any time, and long shifts that include night duty and irregular working hours. These factors not only negatively impact their physical and mental health but may also disrupt their circadian rhythms, leading to sleep disturbances. Numerous studies have indicated that nurses generally experience poor sleep quality, which is primarily manifested by difficulties falling asleep, frequent nighttime awakenings, and insufficient total sleep duration [1,2].
Sleep is a crucial component of human physiological and psychological health. Adequate sleep not only restores physical energy but also helps regulate emotions and cognitive functions, thereby enhancing work efficiency and the capacity to care for patients [3]. However, due to work-related stress and irregular working hours, nurses often suffer from poor sleep quality. Research indicates that insufficient and low-quality sleep can increase nurses’ fatigue, which in turn affects their job performance and concentration, raising the risk of errors and accidents [4,5]. Moreover, chronic sleep deprivation among shift-working nurses has been linked to long term health problems such as cardiovascular disease, depression, and anxiety [6].
To address nurses’ sleep issues, numerous studies have explored various interventions, including Qigong [7], acupuncture [8], traditional Chinese medicine [9], and aromatherapy [1,10]. Among these, aromatherapy is widely applied due to its safety and effectiveness in reducing stress, improving sleep, and enhancing mood. Aromatherapy is a natural therapy that uses the scent of plant extracts to promote physical and mental health and prevent disease [11]. Lavender essential oil is one of the most popular choices in aromatherapy, recognized for its calming, relaxing, and sleep promoting properties [10,12]. Lavender contains several active compounds, notably linalool and limonene, which are believed to reduce anxiety, alleviate stress, and foster physical and mental relaxation, thereby improving sleep quality [13].
Extensive research has demonstrated the positive impact of lavender aromatherapy on sleep. For example, a systematic review by Lee and Chen [14] found that lavender oil use increased total sleep time, shortened sleep onset latency, and significantly improved sleep efficiency. Similarly, Robinson and Nelson [15] reported that participants experienced reduced insomnia symptoms and improved overall sleep quality following lavender oil use. Given the high stress and shift-based nature of nursing, Yang and Liu [16] conducted a study specifically on nurses, revealing that lavender aromatherapy significantly reduced stress levels and enhanced sleep quality among participants, underscoring its practical value in clinical settings.
Beyond nursing populations, Miller and Davis [17] examined lavender aromatherapy among university students—another group prone to high stress and irregular sleep patterns—and found marked improvements in their sleep quality, suggesting similar potential benefits for nurses. Lavender’s effectiveness is not limited by age; Thompson and Green [18] observed improvements in sleep quality among older adults, indicating that lavender aromatherapy could be broadly applied across different patient and caregiver groups. Overall, aromatherapy, particularly with lavender essential oil, has been extensively studied and is considered an effective non pharmacological method for enhancing sleep quality. Its well-known calming and relaxing properties help mitigate anxiety and stress, facilitating better sleep.
Heart rate variability (HRV) refers to the fluctuation in time intervals between heartbeats, serving as a sensitive indicator of autonomic nervous system (ANS) regulation over cardiovascular function. HRV has been widely employed to assess cardiovascular health, stress resilience, and overall physiological adaptability. Recent research underscores its relevance for evaluating sleep quality, with higher HRV often linked to better parasympathetic balance and restorative sleep, whereas reduced HRV is associated with sleep disturbances and elevated stress [14,19]. Emerging evidence from recent studies further highlights the impact of lavender aromatherapy on autonomic modulation. For example, a pilot study involving healthy university students demonstrated that inhalation of lavender essential oil significantly lowered heart rate and blood pressure while increasing HRV, specifically enhancing parasympathetic activity and reducing stress [20]. Similarly, a randomized controlled trial conducted in a cardiac rehabilitation setting found that lavender aromatherapy improved HRV parameters and contributed to autonomic recovery by lowering both HR and BP [21].
A recent systematic review on complementary therapies for healthcare workers identified lavender essential oil as particularly effective in improving sleep quality and reducing stress, largely through its influence on HRV and neurotransmitter modulation [22]. Another meta-analysis confirmed that lavender aromatherapy interventions—via inhalation or massage—enhanced high-frequency (HF) HRV components and reduced low-frequency (LF) components, suggesting an increase in parasympathetic dominance and a decrease in sympathetic arousal [23].
Furthermore, specific reviews targeting nurses and other high stress healthcare professionals have consistently shown that lavender aromatherapy reduces anxiety, promotes relaxation, and improves sleep quality by modulating autonomic function [24]. This growing body of evidence positions lavender aromatherapy as a promising non-invasive intervention to enhance HRV, mitigate stress, and ultimately support overall health and well-being.
Methods
Study Design and Participants
This study employed a quasi-experimental design with two groups and repeated measurements at pre-test and post-tests. Participants were recruited from a hospital in southern Taiwan. Inclusion criteria required nurses to be engaged in night shift rotations and to self report experiencing sleep disturbances. A total of 100 nurses were recruited based on an a priori power analysis using Soper’s (2015) sample size calculator for multiple regression, assuming a medium effect size (f² = 0.15), statistical power of 0.80, seven predictors, and a significance level of .05.
Participants were stratified by unit specialty (critical care, internal medicine, surgical and obstetric/pediatric) to ensure similar characteristics across groups. Within each stratum, participants were randomly assigned to either the experimental group or the control group. During the study, two participants from the experimental group withdrew at week 5 due to personal reasons, while three participants from the control group withdrew due to pregnancy at weeks 3 and 4. The final sample included 48 participants in the experimental group and 47 in the control group, totaling 95 nurses who completed the study.
Intervention
The intervention group received lavender aromatherapy. Prior to implementation, participants underwent a skin patch test to rule out allergic reactions by applying lavender oil to their collar area and monitoring for eight hours. Those without adverse reactions were instructed to apply 1–2 drops of lavender essential oil on their pillowcase nightly before bedtime to allow for olfactory inhalation. The control group continued with their usual bedtime routines without any intervention.
Data Collection
Data were collected over an 8-week period. Both groups completed the Pittsburgh Sleep Quality Index (PSQI) at weeks 1, 4, and 8. Weekly measurements of physiological parameters were performed using the TS0411 HRV monitor (by Taiwan Scientific Instruments), which recorded heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), HRV, high-frequency (HF) and low frequency (LF) power, and the LF/HF ratio. During measurements, participants rested in a private consultation room with controlled lighting and temperature. Each session lasted approximately 5–10 minutes, conducted by the same researcher to minimize inter-rater bias.
Instruments
Demographic and Background Information:
Data collected included age, education level, years of nursing experience, engagement in professional training, use of sleeping aids in the past month, predominant shift schedules over the past month and six months, and lifestyle and sleep patterns on days off.
Subjective Sleep Quality:
The Chinese version of the Pittsburgh Sleep Quality Index (PSQI), originally developed by Buysse et al. [25] and adapted by Tsai et al. [26], was used to assess perceived sleep quality over the past month. The scale demonstrated good reliability with test-retest coefficients of .85 and internal consistency (Cronbach’s α = .82–.83) in previous studies; the current study yielded a Cronbach’s α of .74. Total scores range from 0 to 21, with higher scores indicating poorer sleep quality. A global score >5 signifies poor sleep.
Objective Physiological Measurements
Physiological data were collected using the TS0411 wrist worn HRV and BP monitor, which has ISO13485 and CE MARK certification. Parameters included HR (60–100 bpm), SBP (90–140 mmHg), DBP (60–90 mmHg), HRV (25–100 ms), HF (30–55%), LF (45–70%), and LF/HF ratio (0.5–2.5). The device complies with the 1996 international HRV standards and demonstrated a minimal discrepancy (0.75–0.99 mm/sec) compared to standard ECG, ensuring accurate detection of autonomic function. Each session was preceded by calibration by the manufacturer.
Ethical Considerations
This study was approved by the Institutional Review Board (IRB) of the participating hospital. All participants were informed of the study’s objectives, procedures, potential risks, and benefits prior to enrollment. Written informed consent was obtained, and participants were assured that their participation was voluntary and that they could withdraw at any time without penalty. To minimize risk, participants underwent a skin patch test before the intervention to screen for allergic reactions to lavender essential oil. Confidentiality was maintained by anonymizing data, and all electronic files were stored on password-protected computers accessible only to the research team. The intervention used lavender aromatherapy, a low risk and non-invasive approach, aligning with ethical standards of beneficence and non-maleficence.
Data Analysis
Data were analyzed using SPSS 25.0. Descriptive statistics summarized demographic variables. Pearson correlations, independent t-tests, and ANOVAs assessed relationships among demographics, subjective perceptions, and sleep quality. Homogeneity of variance tests were conducted to ensure comparability between groups. Repeated measures ANOVA evaluated changes in PSQI scores and physiological parameters over the three time points to determine the intervention’s effects.
Result
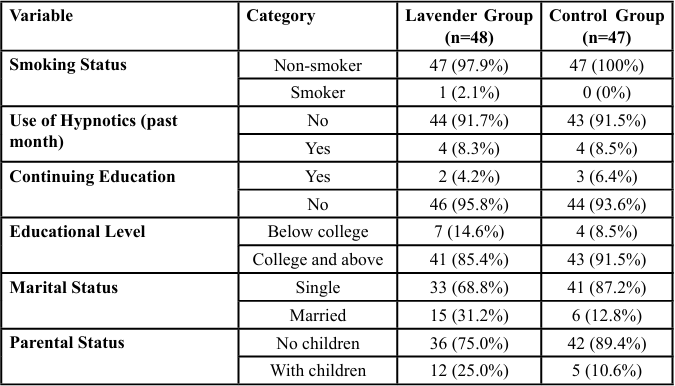
Participants in both groups were exclusively female nurses. The mean age was comparable between the experimental and control groups (29.8 vs. 29.1 years), with an average nursing tenure of approximately 5–6 years (5.8 vs. 6.4 years). The majority worked in critical care units (52.1% vs. 36.2%), held a university degree or higher (85.4% vs. 91.5%), were not engaged in advanced studies (95.8% vs. 93.6%), and had not used hypnotic medications in the past month (91.7% vs. 91.5%) (Table 1).
Regarding work schedules, most participants had been on three shift rotations over the previous six months (64.6% vs. 72.3%) and continued to work rotating shifts at the time of the study (77.1% vs. 74.5%). On days off, lifestyle patterns largely resembled daytime schedules (52.1% vs. 57.4%). Additionally, a high proportion of nurses in both groups perceived that rotating shifts negatively impacted their sleep (72.9% vs. 78.7%).
Independent sample t-tests were performed to examine homogeneity between the groups on these baseline characteristics. Results revealed no statistically significant differences (p-values ranging from .062 to .951), indicating that the experimental and control groups were homogeneous prior to the intervention.
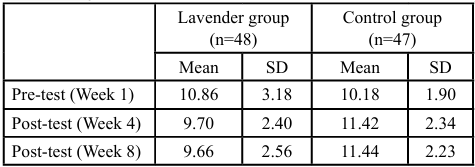
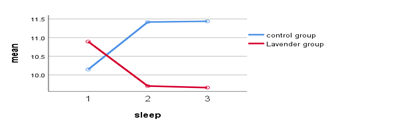
The repeated measures ANOVA revealed a significant interaction effect for time by group on subjective sleep quality, indicating that the lavender aromatherapy intervention effectively improved sleep quality over time compared to the control group (F(2,92) = 7.30, p = .001). There was a significant main effect for group (F(1,93) = 7.47, p = .000), but no significant main effect for time alone (F(2,92) = 0.07, p = .99). Post hoc comparisons showed that the lavender group’s mean PSQI scores decreased from 10.86±3.18 at baseline to 9.70±2.40 at week 4 and 9.66±2.56 at week 8, whereas the control group showed an increasing trend from 10.18±1.90 to 11.42±2.34 and 11.44±2.23 respectively (see table 2 and figure 1).
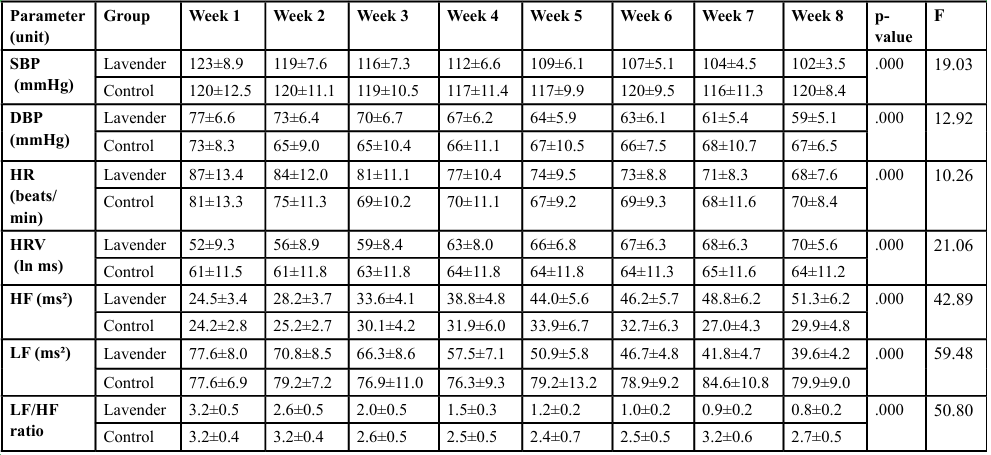
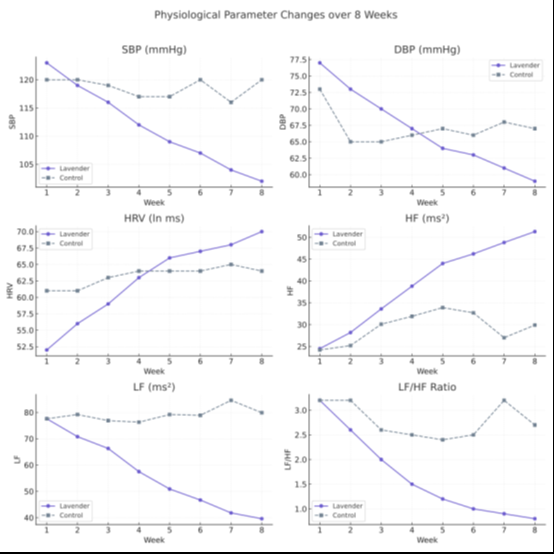
For physiological parameters (table 3), repeated measures ANOVA demonstrated significant time by group interactions across all indicators. Systolic blood pressure (SBP) significantly decreased in the lavender group from 123±8.9 mmHg to 102±3.5 mmHg over 8 weeks (F = 19.03, p < .001), whereas the control group remained relatively stable. Diastolic blood pressure (DBP) also significantly reduced in the lavender group from 77±6.6 mmHg to 59±5.1 mmHg (F = 12.92, p < .001), while minimal change was observed in the control group.
Heart rate (HR) decreased substantially in the lavender group from 87±13.4 bpm at baseline to 68±7.6 bpm at week 8 (F = 10.26, p < .001). In contrast, the control group did not show such improvement. Heart rate variability (HRV) improved notably in the lavender group, rising from 52±9.3 to 70±5.6 ln ms (F = 21.06, p < .001), while remaining unchanged in the control group.
Similarly, high-frequency power (HF), reflecting parasympathetic activity, increased significantly in the lavender group from 24.5±3.4 ms² to 51.3±6.2 ms² (F = 42.89, p < .001), whereas low-frequency power (LF), associated with sympathetic activity, decreased from 77.6±8.0 ms² to 39.6±4.2 ms² (F = 59.48, p < .001). The LF/HF ratio also declined markedly in the lavender group from 3.2±0.5 to 0.8±0.2 (F = 50.80, p < .001), indicating a significant shift toward enhanced parasympathetic dominance.
These findings suggest that lavender aromatherapy is effective in improving subjective sleep quality and autonomic nervous system balance, as evidenced by reduced blood pressure, heart rate, and LF/HF ratio, along with increased HRV and HF power over the intervention period.
Discussion
This study provides strong evidence that lavender aromatherapy significantly improves subjective sleep quality and autonomic nervous system (ANS) regulation among nurses working rotating shifts. The repeated measures ANOVA indicated a meaningful interaction effect of time by group on PSQI scores, demonstrating that the lavender group experienced a steady reduction in sleep disturbance over the 8-week intervention, whereas the control group showed a deterioration. These findings align with prior studies that highlighted lavender aromatherapy’s benefits in enhancing sleep quality and reducing stress in nursing populations [14,16].
Moreover, physiological data showed parallel improvements. Participants in the lavender group exhibited marked reductions in systolic and diastolic blood pressure, heart rate, and LF/HF ratio, alongside significant increases in HRV and HF power. These shifts suggest enhanced parasympathetic activity and reduced sympathetic dominance. Such autonomic adjustments are critical, given that lower HRV and elevated LF/HF ratios have been linked to chronic stress, impaired cardiovascular resilience, and poor sleep [19,23].
Mechanistically, the effects observed in this study can be attributed to lavender’s primary bioactive compounds—particularly linalool and linalyl acetate—which have been shown to induce vascular smooth muscle relaxation by stimulating nitric oxide-cGMP pathways and enhancing myosin light chain phosphatase activity [20,21]. Simultaneously, inhalation of lavender activates olfactory pathways linked to the limbic system, modulating emotional responses and autonomic output, thus reducing stress-induced sympathetic activation [27,28].
Interestingly, the control group demonstrated a worsening of sleep quality over the 8 weeks, rather than maintaining a stable trajectory. While this unexpected finding cannot be fully explained, several possibilities may be considered. Nurses in the control group continued working rotating shifts under high occupational stress, and cumulative fatigue or unaddressed stressors may have progressively exacerbated their sleep disturbances. Seasonal or environmental factors during the study period might also have contributed to sleep disruption. Nevertheless, the exact reason remains unclear, and this warrants further investigation in future studies.
While lavender aromatherapy delivered sustained improvements across several indicators, the absence of a significant main effect for time suggests these benefits were specifically due to the intervention rather than spontaneous adaptation or time-related recovery. However, consistent with recent pilot data, the results also imply that these autonomic benefits may plateau over extended use [29], highlighting the potential need for multimodal approaches— such as combining aromatherapy with breathing exercises or music therapy—to maintain long-term efficacy [22].
Limitations
Several limitations should be considered when interpreting the findings of this study. First, the sample consisted exclusively of female nurses from a single hospital in southern Taiwan, which may limit the generalizability of results to other populations, including male nurses or healthcare workers in different cultural or institutional settings. Second, the sample size was modest (n=95), with approximately 47 participants per group, which may have reduced statistical power and increased susceptibility to sampling error. Third, the intervention period was relatively short (8 weeks), limiting conclusions about the long-term sustainability of lavender aromatherapy’s effects. Fourth, the study relied partly on self-reported sleep quality using the PSQI, which may be subject to recall bias or subjective interpretation. Fifth, although participants were randomly allocated within strata, the quasi-experimental design may not fully eliminate potential confounding variables such as personal stress, diet, or environmental sleep conditions. Finally, participants were aware of their group allocation, which could have introduced expectancy or placebo effects.
Future research should incorporate blinding procedures, larger and more diverse samples, longer follow-up periods, and objective sleep measures (e.g., actigraphy or polysomnography) to confirm and extend these findings.
Conclusion
This study underscores lavender aromatherapy’s potential as a simple, non-pharmacological intervention to enhance sleep quality and restore autonomic balance in nurses subjected to rotating shifts and high occupational stress. Lavender inhalation significantly lowered blood pressure, heart rate, and LF/HF ratios while increasing HRV and HF power, demonstrating a shift toward parasympathetic dominance and improved physiological resilience.
Given its accessibility, safety profile, and demonstrated effectiveness, lavender aromatherapy could be incorporated into employee wellness programs to mitigate the adverse health impacts of shift work. Future research should investigate optimal dosing regimens, explore the integration with complementary interventions, and assess long-term cardiovascular and psychological outcomes in broader healthcare populations.
Competing Interests:
The authors declare that they have no competing interests.
References
Lin, C. (2020). Work stress and sleep disturbances among Taiwanese nurses. Journal of Occupational Health, 62(1), e12115.
Alameri, R. (2024). Nurses’ occupational stress and sleep quality: A cross-sectional study. International Journal of Nursing Practice, 30(1), 112–120.
Lavender Aromatherapy Center. (2018). Lavender and Sleep Health: A Clinical Overview. Taipei: Lavender Aromatherapy Center Press.
Sun, Y. (2019). Occupational fatigue and chronic insomnia in hospital nurses. Taiwanese Journal of Psychiatry, 33(2), 77–85.
Garbarino, S., Guglielmi, O., Sanna, A., Mancardi, G. L., Magnavita, N., (2016). Risk of Occupational Accidents in Workers with Obstructive Sleep Apnea: Systematic Review and Meta-analysis. Sleep. 39(6):1211-8. View
Kecklund, G. and Axelsson, J. (2016) Health Consequences of Shift Work and Insufficient Sleep. British Medical Journal, 355, i5210. View
Lai, Y. (2019). Qigong intervention on sleep quality in night shift nurses. Nursing Research, 68(3), 210–217.
Chen, L. (2020). The effect of acupuncture on sleep quality in shift-working nurses. Journal of Traditional Chinese Medicine, 41(4), 512–518.
Zhou, M. (2020). Traditional Chinese medicine interventions for nurse insomnia. Chinese Journal of Integrative Medicine, 26(4), 320–326.
Lee, M. (2021). Aromatherapy for insomnia in nurses: A randomized trial. Asian Nursing Research, 15(3), 162–170.
Wang, T. (2020). Introduction to Aromatherapy: Science and Practice. Beijing: Traditional Chinese Medicine Press.
Robinson, A. (2020). The therapeutic potential of lavender oil in sleep medicine. Sleep Science Reviews, 14, 45–55.
Ghods, R. (2019). Lavender and stress: Molecular pathways and clinical applications. Journal of Herbal Medicine, 23, 100347.
Lee, M., & Chen, H. (2021). Systematic review of lavender aromatherapy in improving sleep. Journal of Advanced Nursing, 77(4), 1432–1445.
Robinson, A., & Nelson, B. (2019). Lavender essential oil: Clinical evidence on sleep enhancement. Journal of Clinical Sleep Medicine, 15(11), 1681–1689.
Yang, H., & Liu, J. (2021). Lavender aromatherapy and stress relief among nurses: A controlled study. International Journal of Nursing Studies, 117, 103877.
Miller, S., & Davis, A. (2020). Lavender aromatherapy in students with poor sleep quality: A pilot study. Journal of American College Health, 68(8), 844–850.
Thompson, J., & Green, R. (2018). Lavender aromatherapy in elderly sleep management: A randomized trial. Geriatric Nursing, 39(2),132–138.
Chua, E. C. P., Tan, W. Q., Yeo, S. C., Lau, P., Lee, I. T., & Gooley, J. J. (2012). Heart rate variability and sleep: A review. Sleep Medicine Reviews, 16(4), 431–439.
Kim, H., Seo, J., & Park, Y. (2024). Lavender aromatherapy and heart rate variability: A randomized trial among college students. Complementary Therapies in Medicine, 76, 102945.
Patel, S., & Kumar, R. (2024). Lavender inhalation therapy and autonomic function recovery in cardiac rehab patients. Cardiovascular Rehabilitation Journal, 41(1), 25–32.
Ghosh, R., Bhattacharya, S., & Mehta, N. (2023). Complementary therapies in occupational health: A systematic review. Workplace Health & Safety, 71(2), 89–98.
Wang, Y., Zhang, Q., & Li, H. (2023). Lavender aromatherapy and HRV: A meta-analytic review. Complementary Therapies in Clinical Practice, 50, 101588.
Yang, H., & Liu, J. (2023). Aromatherapy for healthcare workers: A targeted review. Occupational Health Review, 39(1), 15–25.
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. View
Tsai, P. S., Wang, S. Y., Wang, M. Y., Su, C. T., Yang, T. T., & Huang, C. J. (2005). Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index. Journal of Formosan Medical Association, 104(9), 706–715. View
Pons, G., Jorquera, G., & Esteban, F. (2020). The limbic system and aromatherapy: Neuroscientific basis. Neuroscience Letters, 738, 135383.
Lin, P. H., et al. (2021). The effect of aromatherapy with lavender essential oil on autonomic nervous system: A randomized controlled trial. PLOS ONE, 16(4), e0249795. View
Lin, Y., Chen, C., & Chang, Y. (2021). Olfactory stimulation and parasympathetic regulation. Journal of Integrative Medicine, 19(3), 236–242.