Journal of Mental Health and Social Behaviour Volume 7 (2025), Article ID: JMHSB-202
https://doi.org/10.33790/jmhsb1100202Review Article
Childhood Trauma, Substance Use, and Stigma: Pathways of Risk and Practices for Building Resilience
Noel Casiano1*, Jordan J. Oquendo2, and Nicholas Casiano3
1,3The Life Center of CT, Inc, 15-17 May Street, Hartford, CT 06105, United States.
2School of Public Policy, University of Connecticut, United States.
Corresponding Author Details: Noel Casiano, The Life Center of CT, Inc, 15-17 May Street, Hartford, CT 06105, United States.
Received date: 11th June, 2025
Accepted date: 11th September, 2025
Published date: 13th September, 2025
Citation: Casiano, N., Oquendo, J. J., & Casiano, N., (2025). Childhood Trauma, Substance Use, and Stigma: Pathways of Risk and Practices for Building Resilience. J Ment Health Soc Behav 7(2):202.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Childhood trauma is increasingly recognized as a significant precursor to a range of adverse psychological and behavioral health outcomes, including the development of substance use disorders (SUD). Individuals exposed to early life adversities—such as abuse, neglect, or household dysfunction—face heightened risks for long-term emotional dysregulation, maladaptive coping strategies, and disrupted neurobiological development. Compounding these risks, stigma surrounding both trauma and substance use presents a formidable barrier to treatment engagement, recovery, and reintegration. This literature review synthesizes empirical research examining the interconnections among childhood trauma, substance use, and stigma. Key findings underscore how traumatic childhood experiences influence substance use trajectories and how stigma, both societal and internalized, amplifies vulnerability and impedes recovery. The review advocates for trauma-informed prevention and intervention strategies that address the multifactorial impact of stigma and prioritize holistic, compassionate care. Recommendations for clinical practice, public health policy, and future research are provided to support individuals affected by these intersecting challenges. This review synthesizes findings from 45 empirical studies identified through a systematic search.
Keywords: Childhood Trauma, Substance Use, Stigma, Adverse Childhood Experiences (ACEs), Trauma-Informed Care, Recovery, Mental Health
Introduction
Childhood trauma, encompassing experiences of emotional, physical, or sexual abuse, neglect, or household dysfunction before the age of 18, has emerged as a critical determinant of long-term psychological, emotional, and behavioral health. A growing body of interdisciplinary research reveals a robust association between early adverse childhood experiences (ACEs) and the development of substance use disorders (SUD) in adolescence and adulthood. These early traumatic exposures disrupt normative neurodevelopmental trajectories, alter stress response systems, and significantly increase the risk for maladaptive coping mechanisms, including substance misuse.
The intersection of childhood trauma, substance use, and stigma represents a complex and multifaceted public health concern. Individuals who have endured trauma and later engage in substance use often face compounded stigma, both self-directed and socially imposed, which can further exacerbate psychological distress, hinder recovery efforts, produce isolation, and create barriers to accessing appropriate care. Stigma not only shapes societal attitudes and responses toward those with SUD but also contributes to internalized shame, marginalization, and underutilization of support services.
This literature review aims to synthesize current empirical findings on the interrelated dynamics of childhood trauma, substance use, and stigma. Drawing from studies across psychology, psychiatry, social work, and public health, the review highlights the importance of trauma-informed approaches in prevention, harm reduction, clinical intervention, and policy development. By deepening our understanding of how early trauma influences substance use trajectories and how stigma serves as a barrier to recovery, this work underscores the urgency of developing integrative, compassionate, empathetic, and evidence-based frameworks to address these intersecting challenges.
This literature review is grounded in the Trauma-Informed Care (TIC) framework, which emphasizes the recognition of trauma’s widespread impact and the importance of responsive care environments [1]. The TIC model serves as a guiding lens through which the interplay between childhood trauma, substance use, and stigma is examined. By applying this framework, the review highlights how early adverse experiences disrupt neurobiological development, increase vulnerability to addiction, and intersect with societal stigma, ultimately influencing pathways to recovery.
Method
Literature Search Strategy
This review utilized a systematic literature search to identify peerreviewed empirical studies that explore the relationships among childhood trauma, substance use, and stigma. Searches were conducted across multiple academic databases, including PubMed, PsycINFO, Scopus and Web of Science. Search terms included combinations of the following keywords: childhood trauma, adverse childhood experiences (ACEs), substance use, substance use disorder (SUD), addiction, stigma, recovery, and trauma-informed care. Boolean operators (AND/OR) were employed to refine results. Additionally, the reference lists of key articles were hand-searched to locate relevant studies that may not have appeared in the initial database queries.
Inclusion and Exclusion Criteria
Studies were eligible for inclusion if they met the following criteria: (a) published in a peer-reviewed journal between 2008 and 2024; (b) written in English; (c) examined at least two of the three focal constructs: childhood trauma or ACEs, substance use or SUD, and stigma; (d) included human participants aged 12 years or older; and (e) utilized quantitative, qualitative, or mixed-method research designs. Studies were excluded if they were dissertations, opinion pieces, theoretical commentaries, or if they focused solely on adult trauma without a connection to childhood experiences. Articles that did not address the concept of stigma in the context of trauma or substance use were also excluded.
Data Extraction and Thematic Synthesis
Following the initial screening of titles and abstracts, full-text reviews were conducted for all studies that met the inclusion criteria. In total, 45 empirical studies were selected for comprehensive analysis. Data extraction focused on study characteristics, sample demographics, definitions and measures of childhood trauma or ACEs, substance use behaviors or diagnoses, and the presence and type of stigma explored.
A thematic synthesis approach was employed to organize findings across diverse study designs and disciplinary perspectives. The analysis identified several overarching themes: (a) the psychological and neurodevelopmental consequences of childhood trauma; (b) trauma-related mechanisms contributing to substance use initiation and maintenance; (c) the role of both perceived and enacted stigma in treatment engagement and recovery outcomes; and (d) the efficacy of trauma-informed care models in addressing the needs of individuals with co-occurring trauma and substance use histories.
Quality Appraisal
To enhance methodological rigor, included studies were assessed using criteria adapted from the Critical Appraisal Skills Program (CASP) for evaluating both quantitative and qualitative research. Key quality indicators included the clarity of research objectives, appropriateness of study design, sampling methods, reliability and validity of measurement tools, data analysis techniques, and transparency of reporting. Studies that lacked sufficient methodological detail or exhibited notable bias were noted, though not excluded, in order to reflect the full scope of available evidence and acknowledge limitations in the current literature base.
Neurobiological and Psychological Consequences of Childhood Trauma
Childhood trauma is broadly defined as the experience of physical, emotional, or sexual abuse or neglect before the age of 16. Such experiences have been consistently linked to a range of adverse outcomes in adulthood, including increased risk of depression, anxiety, maladaptive coping behaviors, and impaired social functioning [2-4]. The developmental impact is particularly damaging, as it interferes with the formation of secure attachments and the development of emotional regulation and self-worth [5].
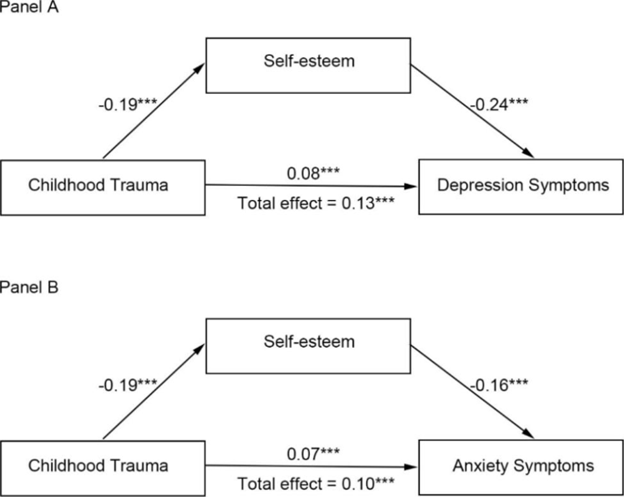
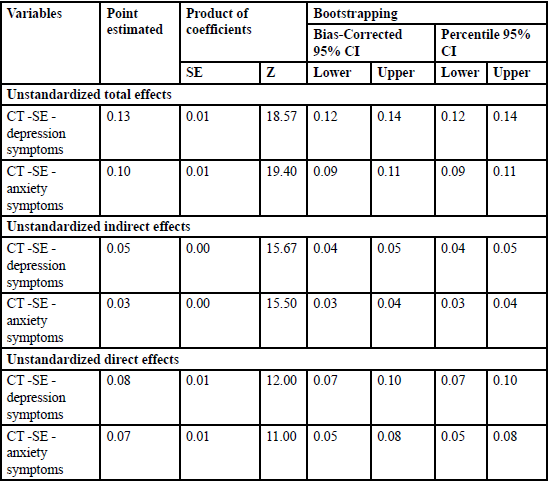
Berber Çelik and Odacı [6] found that individuals with a history of childhood trauma exhibited elevated symptoms of anxiety, depression, and stress, with low self-esteem acting as a mediating factor. These outcomes underscore the neuropsychological imprint of early trauma and its long-term effect on emotional and cognitive processing. Li et al. [2] further revealed a connection between childhood trauma, self-esteem, and higher risk for depression and anxiety. An example of their results below in Figure 1 and Table 1 that childhood trauma leads to higher risk of lower self-esteem and depression and anxiety symptoms, which according to Merrick et al.[4] can often lead individuals to engage in substance abuse behavior. Panels A and B demonstrate self-esteem mediating the effect of childhood trauma on depression and anxiety and an indirect path from childhood trauma to depression and anxiety symptoms, all being statistically significant. Table 1 shows the unstandardized total, direct and indirect effects of the two hypothetical models.
Pathways from Trauma to Substance Use
The Role of Early Life Stress and Adverse Childhood Experiences (ACEs)
Adverse Childhood Experiences (ACEs) include a range of traumatic events such as familial substance use, exposure to violence, neglect, and extreme poverty. These experiences are associated with significant mental health challenges in adolescence and adulthood, including increased susceptibility to substance misuse [4,7]. Longitudinal research demonstrates a clear, dose-response relationship between the number of ACEs and elevated risk for both mental health disorders and chronic medical conditions later in life [2,8].
The intersection of poverty with childhood trauma intensifies these risks. Children growing up in impoverished environments often encounter instability and uncertainty, which can compound emotional stress and contribute to long-term psychological vulnerability [9]. Inglis et al. [10] argue that stigma associated with poverty itself contributes to diminished mental well-being, creating a compounded risk profile for affected individuals. Davis et al. [11] highlighted how adolescents with multiple ACEs showed directional associations between increased cannabis use and heightened depressive symptoms. Furthermore, indicating a potentially self-medicating role of substance use in trauma survivors.
Mechanisms Linking Trauma and Substance Use Disorder (SUD)
The developmental consequences of early trauma can alter stress-response systems and neural pathways involved in reward, emotion regulation, and executive functioning, making individuals more susceptible to substance use [3]. Substance use may serve as a maladaptive coping mechanism for trauma-related distress. Li et al. [2] found that impaired emotion regulation and diminished self-esteem, both consequences of early trauma, significantly mediated the relationship between childhood trauma and adult psychopathology, including substance use.
Furthermore, ACEs contribute to the onset and progression of SUD by increasing psychological distress and reducing access to protective factors, such as supportive relationships and stable environments [4]. Preventative strategies focused on creating safe, nurturing communities and reducing family-level risk factors, are critical in mitigating the long-term consequences of ACEs throughout an individual’s life.
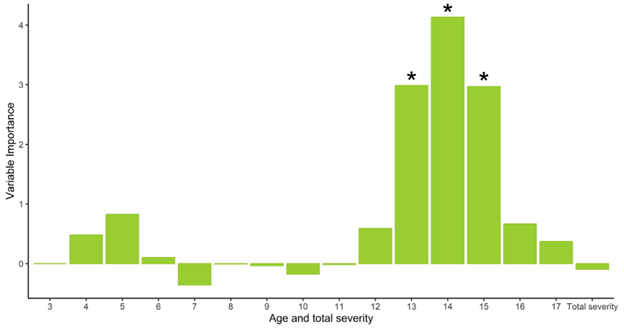
Cagdas Türkmen et al. [12] collected structural MRI data from 35 adults with alcohol use disorder (AUD) and 28 healthy controls along with a questionnaire and an interview to examine the impacts of ACEs on one’s cognitive ability to control their impulsive behaviors. MRI scans revealed reduced cortical thickness in brain regions involved with self-control for adults with AUD who experienced ACEs, suggesting that there is relevance in the association of ACEs and development and maintenance of AUD [12]. They also ran a permutation test of a random forest regression model for time-specific abuse severity from 3 to 17 years of age as a predictor of childhood trauma and brain areas associated with self-control. Figure 2 below shows that higher abuse severity between the ages of 13 and 15 was significantly important in predicting reduced cortical thickness in brain areas associated with self-control. One’s ability to have selfcontrol over impulsive behaviors such as alcohol or substance abuse could be a result of existing depression and anxiety symptoms that are present because of childhood trauma [3,4].
Stigma Typologies and Barriers to Treatment
While SUD is increasingly recognized as a chronic and treatable mental health condition, individuals with SUD face significant barriers to treatment due to pervasive societal stigma [13,14]. Stigmatization manifests through discrimination, stereotyping, and social exclusion, often shaped by cultural values and geographic location [15]. This stigma not only delays treatment-seeking behavior but also worsens mental health outcomes by reinforcing shame and social isolation.
Whipple et al. [14] demonstrated that individuals who perceived substance users as possessing weak character or as being able to quit on their own reported higher levels of substance use stigma, as measured by the Perceived Stigma of Substance Abuse Scale (PSAS). This stigmatization creates a feedback loop that discourages individuals from accessing care, further entrenching the cycle of addiction and marginalization [16].
Cost, fear of legal consequences, and anticipated discrimination are also significant treatment barriers [14]. Addressing stigma through community education, policy reform, harm reduction, and personcentered treatment approaches is essential to increase engagement in care and reduce the harms associated with SUD.
Resilience and Trauma-Informed Care Models
Recovery from childhood trauma and SUD is possible, particularly when treatment incorporates trauma-informed principles. These approaches prioritize safety, empowerment, trust, and collaborative decision-making. They also consider the pervasive effects of trauma and recognize the role of stigma in undermining recovery.
Integrated interventions that combine behavioral therapy, peer support, and social services have shown promise in reducing relapse rates and improving mental health outcomes. Cultivating resilience through supportive relationships, community resources, and strengths-based programming is vital in fostering long-term recovery.
Best Practices for Building Self-Esteem and Resilience
Evidence across developmental psychology, psychiatry, and social work consistently demonstrates that diminished self-esteem and limited resilience are central mediators linking childhood trauma to substance use vulnerability [2,6]. Accordingly, fostering self-esteem and resilience represents a critical target for both prevention and intervention. Best practices in this domain emphasize interventions that integrate trauma-informed care, strengths-based approaches, and community-centered support systems.
1. Trauma-Informed Cognitive and Behavioral Interventions
Cognitive-behavioral approaches, particularly those adapted within trauma-informed frameworks, have demonstrated efficacy in reshaping maladaptive self-perceptions and strengthening adaptive coping. Interventions such as trauma-focused cognitive behavioral therapy (TF-CBT) and dialectical behavior therapy (DBT) promote self-awareness, emotion regulation, and positive self-appraisal while simultaneously addressing trauma symptoms [5]. These modalities help individuals reframe internalized shame and foster healthier narratives about self-worth.
2. Strengths-Based and Empowerment-Oriented Models
Programs rooted in empowerment theory underscore the importance of recognizing and cultivating individuals’ existing competencies and coping strategies. Strengths-based models shift the clinical focus away from pathology toward growth, emphasizing personal agency, goal-setting, and incremental mastery experiences [17]. By reinforcing adaptive achievements, these models build a foundation of self-efficacy that buffers against relapse and reinforces recovery.
3. Relational and Community Supports
Secure, supportive relationships remain among the strongest predictors of resilience in trauma-exposed populations [18]. Peer mentoring, recovery-oriented mutual aid groups, and familybased interventions provide critical relational scaffolding for selfesteem development. Trauma-informed group interventions, when conducted in safe and non-stigmatizing contexts, reduce isolation, normalize experiences, and foster collective resilience. Clinicians are encouraged to intentionally incorporate family members and peers into treatment planning to strengthen social capital.
4. Integration of Mind-Body Practices
Emerging evidence supports the inclusion of somatic and mindfulnessbased practices as adjunctive strategies for resilience-building. Practices such as yoga, mindfulness meditation, and traumasensitive movement therapies have been linked to improved emotion regulation, stress tolerance, and positive self-concept [19]. These approaches reinforce the mind-body connection, counteracting trauma-related dysregulation and supporting holistic healing.
5. Addressing Stigma Through Identity Affirmation
Given the compounding effects of stigma on both trauma recovery and substance use outcomes, interventions that directly confront internalized stigma and affirm identity are essential. Psychoeducation, narrative therapy, and anti-stigma campaigns can help individuals externalize blame, reframe substance use as a health condition rather than a moral failing, and develop a more compassionate sense of self [14]. Reducing stigma at both the individual and community levels strengthens self-esteem and supports reintegration into society.
6. Culturally Responsive and Context-Specific Interventions
Finally, resilience-building practices must be adapted to the cultural, socioeconomic, and community contexts of individuals. Research highlights that resilience is not solely an individual trait but also a collective process shaped by cultural norms, faith traditions, and community values [17]. Interventions that integrate spirituality, cultural identity, and community strengths are particularly effective in marginalized or underserved populations, offering protective buffers against both trauma-related distress and stigma-related harms.
Taken together, these best practices highlight the importance of multi-level, integrative approaches to self-esteem and resilience building. By addressing the internalized effects of trauma, enhancing adaptive coping, and reducing stigma, these strategies contribute to sustainable recovery and improved long-term outcomes for individuals with histories of childhood adversity and substance use.
Implications for Clinical Practice
The integration of self-esteem and resilience-building practices into clinical care has significant implications for improving treatment engagement, retention, and recovery outcomes for individuals with histories of childhood trauma and substance use. First, clinicians should adopt trauma-informed assessment protocols that explicitly evaluate self-esteem, coping strategies, and resilience factors alongside substance use histories. Such assessments allow providers to identify protective strengths in addition to risk factors, thereby creating more balanced and empowering treatment plans.
Second, implementing multi-modal interventions that combine individual therapy, group work, and community-based supports is critical. For example, pairing trauma-focused CBT with peer recovery programs can simultaneously target trauma symptoms, maladaptive cognitions, and the relational isolation often perpetuated by stigma. Similarly, embedding mindfulness practices within outpatient or residential programs can offer clients immediate, experiential tools for stress regulation and self-reflection.
Third, clinical practice should prioritize collaborative goal setting to reinforce autonomy and agency. Engaging clients in shared decision-making around treatment priorities not only enhances motivation but also fosters the self-efficacy that underpins resilience. This collaborative approach is particularly effective in counteracting the powerlessness that often stems from both traumatic experiences and stigmatizing treatment environments.
Finally, providers must remain attentive to cultural humility and contextual sensitivity. Incorporating culturally relevant strengths such as spirituality, community rituals, or indigenous healing practices can enhance intervention effectiveness and ensure care resonates with clients lived realities. Clinicians are also encouraged to advocate at the systems level by supporting anti-stigma policies, equitable access to care, and funding for integrated trauma and addiction services.
In sum, embedding resilience and self-esteem enhancement within trauma-informed, culturally responsive frameworks offers a powerful pathway for recovery. By equipping clients with both intrapersonal resources and supportive environments, clinical practice can shift from a narrow focus on symptom reduction to a more holistic vision of healing, empowerment, and long-term well-being.
Policy Implications
Addressing the intertwined challenges of childhood trauma, substance use, and stigma requires more than clinical interventions; it necessitates structural and policy-level reform that fosters resilience and reduces systemic barriers to recovery. Evidence from trauma and addiction research underscores that resilience is not only cultivated individually but is also sustained within supportive social and institutional environments [17,18].
1. Expanding Trauma-Informed Systems of Care
Policymakers should prioritize the integration of trauma-informed principles across healthcare, education, juvenile justice, and social service systems. Training frontline providers, teachers, healthcare professionals, and case workers in trauma-informed practices can reduce retraumatization, improve engagement, and normalize resilience-building supports. Federal and state agencies could incentivize trauma-informed certification and continuing education for organizations serving high-risk populations.
2. Reducing Structural Stigma Through Public Education
Public stigma toward individuals with SUD often translates into structural discrimination, including punitive policies and inequitable access to services [14]. National and community-level anti-stigma campaigns that reframe substance use as a treatable health condition and emphasize recovery stories can help shift public perceptions. Media guidelines that avoid moralizing language and highlight resilience can further reduce stigma and encourage treatment-seeking.
3. Increasing Access to Integrated, Holistic Services
Resilience and self-esteem are best fostered in environments that provide consistent safety, stability, and opportunity. Policies that expand access to affordable housing, employment supports, childcare, and integrated behavioral health services can mitigate the social determinants that perpetuate trauma and relapse risk [9]. Bundling substance use treatment with trauma-informed mental health care ensures that clients receive holistic, coordinated support.
4. Culturally Responsive Policy Design
Policy frameworks must account for cultural diversity in how trauma is experienced, expressed, and healed. Federal and state funding streams should encourage the inclusion of culturally specific programming, such as faith-based initiatives, indigenous healing traditions, and community-led recovery networks. By legitimizing diverse approaches, policies can strengthen identity, belonging, and resilience among marginalized populations.
5. Long-Term Investment in Prevention
Finally, sustainable policy solutions must extend beyond treatment to prevention. Investing in early childhood programs that promote safe, stable, and nurturing relationships—such as home visiting, school-based social-emotional learning, and parenting support programs—can reduce ACE exposure and bolster resilience before substance use risk emerges. A preventive, developmental lens ensures that resilience-building is not only a recovery strategy but also a protective buffer throughout the lifespan.
Taken together, these policy directions highlight the importance of embedding resilience and self-esteem promotion within broader public health strategies. By shifting from punitive or fragmented responses to comprehensive, trauma-informed, and culturally grounded systems, policymakers can play a central role in dismantling stigma and fostering recovery-ready communities.
Limitations
This literature review has several limitations that should be considered when interpreting the findings. First, although a systematic search strategy was employed, the review is limited to studies published in English and between 2008 and 2024, which may have excluded relevant research published in other languages or outside this timeframe. This temporal and linguistic restriction could potentially bias the scope of included evidence.
Second, the majority of the included studies relied on selfreported data regarding childhood trauma, substance use, and stigma experiences. Such data are vulnerable to recall bias, social desirability effects, and underreporting, particularly given the sensitive and stigmatized nature of these topics. These biases may affect the accuracy and generalizability of the findings.
Third, the heterogeneity of study designs, populations, and measurement tools across the 45 studies presents challenges for synthesis. Variations in operational definitions of childhood trauma, substance use disorders, and stigma constructs limited the comparability of results and precluded meta-analytic techniques. Consequently, thematic synthesis rather than quantitative aggregation was used, which may limit the precision of effect estimations.
Fourth, the review primarily draws from cross-sectional and observational studies, which restricts causal inference regarding the pathways linking childhood trauma, substance use, and stigma. Longitudinal and experimental studies are needed to more definitively elucidate temporal sequences and mechanisms underlying these associations.
Fifth, while this review emphasized trauma-informed care frameworks, the included literature reflects predominantly Western contexts and healthcare systems. Cultural differences in trauma experiences, substance use patterns, and stigma perceptions may limit the applicability of findings to non-Western or marginalized populations.
Finally, publication bias may have influenced the available literature, as studies reporting significant or positive findings related to trauma, substance use, and stigma are more likely to be published than null or negative results. This bias could overstate the strength of observed associations.
Future research should address these limitations by incorporating diverse populations, standardized measurement approaches, longitudinal designs, and culturally sensitive perspectives to deepen understanding and improve intervention strategies.
Conclusion
The literature clearly indicates that childhood trauma, particularly Adverse Childhood Experiences (ACEs), is a profound and pervasive risk factor for the development of substance use disorders (SUDs) in adulthood. These early-life adversities disrupt neurodevelopmental processes, impair stress regulation systems, and increase vulnerability to maladaptive coping strategies such as substance misuse. Moreover, the compounding effects of social stigma associated with SUD further exacerbate the problem by creating significant barriers to treatment access, retention, and long-term recovery outcomes.
Addressing the public health burden of childhood trauma and substance use requires a comprehensive, multi-tiered approach that includes primary prevention of trauma exposure, public education to reduce stigma, and the implementation of trauma-informed care models in clinical, educational, and community-based settings. Such models not only recognize the widespread impact of trauma but also promote safety, empowerment, and healing across service systems.
Furthermore, the intersection of trauma, addiction, and stigma necessitates systemic change. This includes policy reform, crosssector collaboration, and culturally responsive interventions tailored to the needs of diverse populations. Clinicians, educators, policymakers, and researchers must work in concert to dismantle the structural inequities that perpetuate trauma and limit access to quality care.
Future research should continue to investigate the complex biological, psychological, and sociocultural mechanisms that mediate the relationship between childhood trauma and adult substance use. This includes longitudinal studies that identify early indicators of risk and resilience, as well as intervention studies that test the efficacy of integrative, strengths-based approaches. Importantly, the field would benefit from more research on protective factors such as faith, community support, and adaptive coping strategies that can buffer the negative effects of trauma and promote recovery.
Confronting the intertwined challenges of childhood trauma, substance use, and stigma is not only a clinical imperative but also a moral one. A trauma-informed, recovery-oriented, and equity-driven framework offers the most promising path forward for transforming care, enhancing outcomes, and fostering healing in individuals and communities alike.
Conflicts of interest:
The researcher declares no conflict of interest, and the study received no funding.
References
SAMHSA. (2014). SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. U.S. Department of Health and Human Services. View
Li, C., Fu, P., Wang, M., Xia, Y., Hu, C., Liu, M., Zhang, H., Sheng, X., & Yang, Y. (2023). The role of self-esteem and emotion regulation in the associations between childhood trauma and mental health in adulthood: a moderated mediation model. BMC Psychiatry, 23(1). View
Mandelli, L., Petrelli, C., & Serretti, A. (2015). The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. European Psychiatry, 30(6), 665–680. View
Merrick, M. T., Ford, D. C., Ports, K. A., Guinn, A. S., Chen, J., Klevens, J., Metzler, M., Jones, C. M., Simon, T. R., Daniel, V. M., Ottley, P., & Mercy, J. A. (2019). Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR. Morbidity and Mortality Weekly Report, 68(44), 999–1005. View
Greger, H. K., Myhre, A. K., Klöckner, C. A., & Jozefiak, T. (2017). Childhood maltreatment, psychopathology and wellbeing: The mediator role of global self-esteem, attachment difficulties and substance use. Child Abuse & Neglect, 70, 122– 133. View
Berber Çelik, Ç., & Odacı, H. (2020). Does child abuse have an impact on self-esteem, depression, anxiety and stress conditions of individuals? International Journal of Social Psychiatry, 66(2), 002076401989461. View
Karatekin, C., Mason, S. M., Riegelman, A., Bakker, C., Hunt, S., Gresham, B., Corcoran, F., & Barnes, A. (2023). Adverse Childhood Experiences (ACEs): An Overview of Definitions, Measures, and Methods. In Handbook of adverse childhood experiences: A framework for collaborative health promotion. (pp. 31–45). Springer International Publishing. View
Lin, L., Wang, H. H., Lu, C., Chen, W., & Guo, V. Y. (2021). Adverse Childhood Experiences and Subsequent Chronic Diseases Among Middle-aged or Older Adults in China and Associations With Demographic and Socioeconomic Characteristics. JAMA Network Open, 4(10), e2130143. View
Ridley, M., Rao, G., Schilbach, F., & Patel, V. (2020). Poverty, depression, and anxiety: causal evidence and mechanisms. Science, 370(6522). View
Inglis, G., Jenkins, P., McHardy, F., Sosu, E., & Wilson, C. (2022). Poverty stigma, mental health, and well-being: A rapid review and synthesis of quantitative and qualitative research. Journal of Community & Applied Social Psychology, 33(4), 783–806. View
Davis, J. P., Pedersen, E. R., Tucker, J. S., Prindle, J., Dunbar, M. S., Rodriguez, A., Seelam, R., & D’Amico, E. J. (2023). Directional associations between cannabis use and depression from late adolescence to young adulthood: the role of adverse childhood experiences. Addiction, 118(6). View
Cagdas Türkmen, Tan, H., Gerhardt, S., Bougelet, E., Bernardo, M., Machunze, N., Grauduszus, Y., Maurizio Sicorello, Traute Demirakca, Kiefer, F., & Vollstädt-Klein, S. (2024). The association between adverse childhood experiences and alterations in brain volume and cortical thickness in adults with alcohol use disorder. Addiction Biology, 29(9). View
National Institute of Mental Health. (2024, March). Substance use and co-occurring mental disorders. National Institute of Mental Health. View
Whipple, M. K., Boyke, H., Ferrier, R. C., & Horner, P. S. (2025). Examining the Relationship between Culture and Perceived Societal Substance Use Stigma in a Michigan-Based Mental Health & Addiction Focused Community. Substance Use & Misuse, 60(2), 176-187. View
Fischer, E. P., McSweeney, J. C., Wright, P., Cheney, A., Curran, G. M., Henderson, K., & Fortney, J. C. (2016). Overcoming Barriers to Sustained Engagement in Mental Health Care: Perspectives of Rural Veterans and Providers. The Journal of Rural Health, 32(4), 429–438. View
Bratberg, J., Simmons, A., Arya, V., Bhatia, A., & Vakharia, S. P. (2022). Support, Don’t Punish: Drug Decriminalization Is Harm Reduction. Journal of the American Pharmacists Association, 63(1). View
Ungar, M. (2019). Designing resilience research: Using Multiple Methods to Investigate Risk Exposure, Promotive and Protective Processes, And Contextually Relevant Outcomes for Children and Youth. Abuse & Neglect, Vol. 96,104098, ISSN 0145-2134. View
Masten, A. S., & Barnes, A. J. (2018). Resilience in children: Developmental perspectives. Children, 5(7), Article 98. View
van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking. View