Journal of Public Health Issues and Practices Volume 9 (2025), Article ID: JPHIP-241
https://doi.org/10.33790/jphip1100241Research Article
Perception of Factors Affecting Medication Adherence Among Older Adults: Challenges and Strategies in Primary Health Care in Brazil
Marina Celly Martins Ribeiro de Souza²*, Natália de Cássia Horta¹, Marco Aurélio Santos Pereira², and Celeste de Aguiar Cardoso²
1Pontifical Catholic University of Minas Gerais – Betim campus, Brazil.
2Home institution: The College of New Jersey, United States.
Corresponding Author Details: Marina Celly Martins Ribeiro de Souza, RN, PhD, CNE, CHPN, Professor, Department of Public Health, The College of New Jersey, 2000 Pennington Road, Ewing, NJ 08628, United States.
Received date: 15th July, 2025
Accepted date: 22nd August, 2025
Published date: 25th August, 2025
Citation: Souza, M. C. M. R., Horta, N. C., Pereira, M. A. S., & Cardoso, C. A., (2025). Perception of Factors Affecting Medication Adherence Among Older Adults: Challenges and Strategies in Primary Health Care in Brazil. J Pub Health Issue Pract 9(2): 241.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The high prevalence of chronic noncommunicable diseases (NCDs) among older adults in Brazil presents substantial challenges to medication adherence—an essential component for ensuring therapeutic effectiveness. Adherence is influenced by a range of factors, including socioeconomic status, cultural beliefs, cognitive decline, and health conditions, all of which demand close attention from professionals in Primary Health Care (PHC). Objective: To analyze the challenges faced by PHC professionals in addressing low medication adherence among older adults with NCDs in a municipality within the Metropolitan Region of Belo Horizonte, Minas Gerais. Methods: This action research was conducted in two stages. The first involved a descriptive phase using an electronic questionnaire distributed to professionals from 38 Basic Health Units (UBS), focusing on their perceptions of medication adherence and their interest in participating in focus groups. The second phase involved conducting two focus group sessions with both care and management professionals. The study adhered to the Standards for Reporting Qualitative Research (SRQR), and the data were analyzed using thematic content analysis, following Bardin’s methodological framework. Results: A total of 131 professionals responded to the questionnaire, the majority being women (87%), aged 40–49 years, with 71.8% affiliated with the Family Health Strategy. Only 15.3% had received specific training in older adult health. Eight professionals participated in the focus group discussions. The primary challenges identified included lack of family support (33.6%), low levels of education (23.7%), complexity of therapeutic regimens (9.9%), limited access to medications (6.9%), and forgetfulness (6.9%). Additional barriers reported were popular beliefs, socioeconomic vulnerability, side effects, self-medication, dementia, and alcohol use. Most professionals attributed non-adherence to a combination of intentional and unintentional causes, such as perceived “cure” due to asymptomatic conditions, cognitive impairment, and shortcomings in comprehensive PHC care. Conclusions: Medication adherence among older adults with NCDs is a multifactorial issue influenced by both social determinants of health and intrinsic aspects of aging. The lack of family support, low education levels, and regimen complexity emerged as central barriers. Strengthening the professional–patient relationship, providing specific training on older adult health, and implementing intersectoral strategies are essential measures to improve clinical outcomes within the scope of Primary Health Care.
Key words: Medication Adherence; Older Adults; Primary Health Care; Health Personnel.
Introduction
The prevalence of chronic noncommunicable diseases (NCDs) is high among the older adult Brazilian population, with 58.3% living with more than one NCD and 34.4% with three or more [1]. Among the main NCDs, we highlight hypertension, chronic back problems, diabetes mellitus, arthritis or rheumatism, heart disease, depression, cancer, stroke, asthma, and chronic pulmonary disease. In this context, a key determinant of favourable treatment outcomes prescribed by health professionals is patient medication adherence. Multiple factors influence adherence to pharmacotherapy, which are grouped in the literature as intentional and unintentional [2].
Regarding patient-related factors—such as health status and social and economic conditions—the literature indicates associations between race, marital status, occupation, education, income, age, family and social support, and medication adherence [3]. For instance, with increasing age, older adults are more likely to experience cognitive decline and reduced functional capacity, contributing to non-adherence. Furthermore, older adults in poorer health often receive more prescriptions and may fail to adhere due to financial limitations. Consequently, numerous components influence medication adherence, and it is essential for health professionals to be equipped to identify factors related to the illness experience, medication use, and patient understanding of their health status to promote adherence and enhance health outcomes [3,4]. This article aims to analyze the challenges encountered in addressing low medication adherence in the management of chronic diseases among older adults within the framework of Primary Health Care. Although the determinants of non-adherence are widely discussed in the literature, there remains a gap in understanding how health professionals especially those working in primary care in Latin American contexts perceive these barriers and implement strategies to address them. This study fills this gap by bringing forward the perspectives of frontline health workers in Brazil, contributing to a more contextualized and practice-oriented understanding of medication adherence challenges among older adults.
Methods
This study employed action research methodology, comprising an initial descriptive phase involving voluntary participation of professionals from 38 Basic Health Units (UBS) in a municipality within the Metropolitan Region of Belo Horizonte, MG. The subsequent phase included focus group discussions and the collaborative production of educational videos, engaging professionals from both management and care sectors.
The study followed the Standards for Reporting Qualitative Research (SRQR), using the EQUATOR Network checklist [5]. Initially, a pilot test of the proposed research form was conducted as a data collection tool with three collaborating professionals from the municipality of Juatuba-MG—two physicians and one nurse—between March 20 and 30, 2024. The contributions of these professionals resulted in the following adjustments: inclusion of the CHW (Community Health Worker) position and inclusion of the average response time in the invitation to participate in the research. A total of 1,890 primary health care (PHC) professionals were invited, representing 113 family health teams, 26 oral health teams, and 15 multidisciplinary teams. The online questionnaire comprised three sections: in the first, an Informed Consent Form was provided and identification data of the participant were collected, such as email, full name, age group, education level, field of training, and workplace.
In the second section, with the aim of understanding the professional’s perspective on medication adherence, questions were asked such as whether the professional or their team has previously discussed, reflected on, or addressed the topic within their health unit. It also explores how these professionals perceive elderly patients’ adherence to prescribed medications, highlighting the main facilitators and barriers involved. Additionally, this section investigates the influence of social, demographic, economic, and clinical factors on adherence. It seeks to determine whether non-adherence is typically intentional (a conscious choice) or unintentional, and which unintentional factors are considered most significant. The survey further asks whether any actions or strategies are currently being implemented in the health unit to improve adherence and what specific practices are used in daily work. Finally, it invites suggestions for measures that could be adopted by teams within the health unit to strengthen medication adherence among older adults and provides space for open comments and reflections on the topic. In the third section, an invitation to participate in focus groups was extended.
It was distributed via WhatsApp and email, supported by UBS managers and municipal administrators. Over a three-month period, strategies to enhance participation included weekly WhatsApp reminders to UBS managers (minimum five messages per unit), support from municipal technical advisors, and sharing of the survey link among PHC professionals.
The second phase occurred in May and June 2024, with two focus group sessions. Sixty-five professionals who expressed interest via the initial form were invited. The research protocol was approved by the Research Ethics Committee of PUC Minas (Approval No. 69037123.0.0000.5137). A descriptive analysis was conducted to characterize the participants using frequencies and proportions of categorical variables relating to challenges in medication adherence among older adults. Thematic content analysis of focus group data followed Bardin’s (1979) framework, identifying themes and subthemes relevant to individual, community, and structural dimensions of social determinants of health and their connection to health-disease-care processes [6].
Results
Between April 1 and July 4, 2024, 131 professionals completed the questionnaire. Eight participated in the focus group sessions held on May 23 and June 12. Four duplicate responses were excluded. The largest age group was 40–49 years (38.2%), and 87% of respondents were female. In terms of race, 54.2% identified as mixed-race, 31.3% as white, 13.7% as Black, and 0.7% as Asian. Among respondents, 55.7% held a university degree and 29.8% had completed high school.
Regarding professional roles, 71.8% were part of the Family Health Strategy teams, while 28.2% were support professionals. In terms of experience, 53.4% had worked in PHC for over 10 years, 11.5% for 6–10 years, 21.4% for 1–5 years, and 13.7% for under one year. The most represented professions were Community Health Agents (32.8%), nurses (16.8%), physicians (16%), dentists (3.8%), social workers (3.8%), nutritionists (2.3%), nursing assistants (2.3%), occupational therapists (1.5%), and other professions (each 0.8%): art educators, endemic disease control agents, oral health technicians, psychologists, physiotherapists, and physical education professionals.
Only 15.3% reported having any training in older adult health: 35% completed courses up to 50 hours, 14.9% up to 100 hours, 12.9% up to 180 hours, and 3.2% up to 360 hours. Additionally, 12.9% held postgraduate or specialization qualifications, and 3.2% had a master’s degree in older adult health. Among physicians, 33.3% were Family and Community Physicians, 52.3% general practitioners, 4.7% gynecologists/obstetricians, and 4.7% were nutritionists.
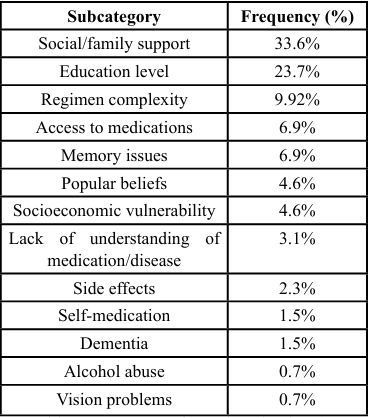
Challenges to Medication Adherence Among Older Adults
Participants reported several adherence challenges, summarized below:
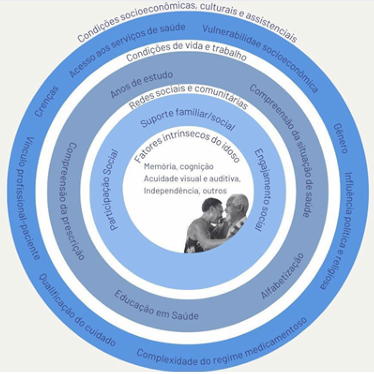
Respondents’ perspectives were analysed within the framework of Social Determinants of Health (SDH), encompassing individual factors, social/community support networks, and macro-structural contexts [7].
Regarding individual factors, participants highlighted that low educational levels among older adults hamper their ability to understand medical prescriptions or to appreciate the significance of medication adherence:
“First, a significant number of older adults can’t read. Another issue is they’re unaware of the health risks caused by missing medication; I don’t know if it’s due to lack of information or ignorance. Many are afraid of medication.” — Respondent A
Lack of understanding of the relevance of medication for disease management—such as for diabetes or hypertension—was noted, with some patients believing they are cured upon seeing favourable lab results and discontinuing treatment:
“The lack of understanding about the importance of correct medication use… many older adults stop taking antihypertensives because they measure blood pressure at home and it’s ‘good,’ so they feel the medication is unnecessary.” — Respondent C
Beliefs and cultural practices also influenced adherence, e.g., reliance on divine healing or alternative therapies:
“Some patients believe in ‘divine healing as the only option’… leading to intentional non-adherence.” — Respondent D
Regimen complexity—particularly polypharmacy—was cited as a major challenge. Older adults frequently struggle with managing multiple medications, confusing pills based on packaging, and by disruptions in pharmaceutical supply:
“They don’t keep track of the medication schedule… Sometimes they take them all together in a pot.” — Respondent Y
Memory deficits were also a significant obstacle.
Family support was emphasised as a key facilitator, especially for those who live alone or lack adequate support networks.
Access challenges emerged from medication unavailability in the Brazilian public health system (REMUME/SUS) and financial barriers. Additional intrinsic factors mentioned included polypharmacy, cognitive decline, dementia, visual impairment, and benzodiazepine misuse.
Quality and continuity of care in Primary Health Care were identified as structural determinants; high physician turnover weakens patient provider relationships, and routine prescription renewals without proper clinical evaluation were criticised:
“Prescription renewals without prior assessment… poor practice.” — Respondent F
“It’s not about quantity but quality of visits…” — Respondents Z and W
Among sociodemographic factors influencing adherence, respondents cited social/family support (90.1%), health conditions (74%), economic factors (67.9%), education (60.3%), patient- provider relationship (45.8%), beliefs/culture (42%), and age (35.9%). Factors less frequently mentioned included sex (14.5%), employment (10.7%), health insurance (6.9%), marital status (6.1%), and race (1.5%).
Regarding clinical conditions, polypharmacy (74%), multimorbidity (70.2%), psychiatric conditions (61.8%), chronic pain (43.5%), insomnia (35.1%), and hearing impairment (25.2%) were identified. Of the professionals, 59.5% attributed non-adherence to synergistic intentional and unintentional causes, 33.6% to unintentional causes, and 6.9% to intentional causes.
Among unintentional determinants, polypharmacy (77.1%), insufficient social support (72.5%), medication unavailability in SUS (61.8%), cognitive decline (59.5%), physical limitations (44.3%), regimen complexity (32.8%), deficient PHC coordination (20.6%), and poor service access (9.2%) were reported.
Intentional non-adherence was mainly due to perceived lack of need (85.5%), side effect concerns (51.9%), fear of adverse effects (45%), disbelief in efficacy (40.5%), cultural/religious issues (35.9%), and inadequate patient–provider relationships (23.7%).
Discussion
Key Findings
This study reveals that medication adherence challenges among older adults are multifaceted, involving individual, social, economic, and health system factors. Low education impedes understanding of prescriptions; misinterpretations based on clinical test results lead to premature treatment cessation. Polypharmacy exacerbates complexities in regimen adherence, especially in the absence of familial support. Limited access to medications, coupled with socio- economic constraints, further compounds adherence challenges. Clinical conditions including chronic and psychiatric illnesses also pose significant barriers. Social determinants such as family and community support are critical to mitigate these issues.
Strengths and Limitations
A major strength of this study is the participation of professionals from all 38 UBS units in the municipality, providing comprehensive insights from an urban context. Limitations include a modest 131 responses from 1,890 invited professionals and an overrepresentation of Community Health Agents, potentially limiting the generalizability.
Comparison with Existing Literature
The findings of this study are closely aligned with the Latin American literature on factors influencing medication adherence among older adults. The lack of family support, highlighted by healthcare professionals as one of the main barriers, is also strongly evidenced by Sanabria and Guzmán in a study conducted in Bolivia, where the absence of emotional and practical support increased the likelihood of non-adherence to treatment. Additionally, both studies point to polypharmacy and the presence of chronic diseases as recurring challenges in the medication management of older populations [8].
In the Chilean context, Figueroa et al. emphasize the importance of health literacy as a key factor in adherence, supporting the observation that low educational levels and limited understanding of medication use and its importance hinder therapeutic compliance. Forgetfulness, frequently cited by Brazilian professionals, is also identified in the Chilean study as a significant cause of non-adherence, especially among older adults managing multiple medications [9].
Fhon et al., in Peru, add relevant data to the discussion by identifying that more than half of the elderly participants did not adhere to their pharmacological treatment. However, the study highlights that factors such as retirement status and a history of stroke (CVA) may facilitate adherence, revealing important clinical nuances [10]. In Cuba, Díaz- Soto et al.also reinforce the impact of polypharmacy and chronic non-communicable diseases such as hypertension and diabetes and draw attention to self-medication and forgetfulness as key barriers, which were similarly reported by Brazilian healthcare professionals. Additionally, they note a gender-related aspect: although women consume more medications, men are less adherent a contrast to the Bolivian findings, which indicate higher non-adherence among women [11].
Implications for Practice and Further Research
Improving medication adherence among older adults requires personalized, multidisciplinary, community-integrated strategies. PHC professionals should be empowered with patient-centred approaches that strengthen therapeutic alliances, enhance health literacy, simplify regimens, and foster social support. Public policies should prioritise educational and social programs, such as community groups and day centres, to support adherence and reduce related complications.
Conflict of Interest Statement
The authors declare no conflicts of interest related to this research. Celeste de Aguiar Cardoso and Marco Aurélio Santos Pereira are medical students at the Pontifical Catholic University of Minas Gerais (PUC Minas), Brazil. Natália de Cássia Horta, a nurse, is a faculty member at PUC Minas, Brazil. Marina Celly Martins Ribeiro de Souza, also a nurse, is a faculty member at The College of New Jersey, United States.
References
Romero, D., & Maia, L. (2020). Health Tomorrow: Discussion Papers 90: The Epidemiology of Aging: New Paradigms. Sergio Arouca National School of Public Health, Oswaldo Cruz Foundation. View
Brazilian Institute of Geography and Statistics. (2024). National Health Survey. View
Schnorrerova, P., Matalova, P., Wawruch, M. (2024). Medication adherence: measurement methods and approaches. Bratisl Lek Listy. 125(4):264-273. View
Pereira, E., Mendonça, L.A. (2024). Difficulties encountered in adherence to antihypertensive treatment in the elderly. COGNITIONIS Scientific Journal. 7(2):e458.
O’Brien, B.C., Harris, I.B., Beckman, T.J., Reed, D.A., Cook D.A. (2014). Standards for Reporting Qualitative Research. Academic Medicine. 89(9):1245–51. View
Bardin, L. (1977). Content analysis. Lisbon: Edições 70. View
GEIB, L. T. C. (2012). Social determinants of elderly health. Ciência & Saúde Coletiva, v. 17, n. 1, p. 123–133. View
SANABRIA C, GUZMÁN F. (2018). Adherencia farmacoterapéutica en pacientes geriátricos del Hospital Santa Bárbara in Sucre - Bolivia. Revista Ciencia, Tecnología e Innovación [Internet]. [cited 2025 Aug 19];16(17):983–90. View
Figueroa Saavedra, C. S., Otzen Hernández, T. F., Figueroa Delgado, V., Sanhueza, P., Candia, J., Figueroa Saavedra, C. S., et al. (2020). Association between health literacy and adherence to medications among older adults. Revista médica de Chile [Internet]. May 1 [cited 2022 Jul 20];148(5):653–6. View
Roberto, J., Pilar del, Gideany Maiara Caetano, Giovanna Sara Cáceda-Ñazco, Alexandre, Zoila Esperanza Leitón-Espinoza. (2024). Factors associated with adherence to antihypertensive agents in the older adult. Revista CUIDARTE. Jan 1;15(2). View
Teresa, D. S. M., Elena, Carbonell, M., Alfonso, B., Miguel, C. M. J., Teresa, D. S. M., et al. (2021). El consumo de medicamentos en pacientes de la tercera edad. Revista Cubana de Medicina [Internet]. [cited 2025 Aug 19];60(2).