Journal of Rehabilitation Practices and Research Volume 3 (2022), Article ID: JRPR-133
https://doi.org/10.33790/jrpr1100133Research Article
Comparison of the Validity of the Timed Up and Go Test (TUG) and Activities-specific Balance Confidence Questionnaire (ABC) to the ‘Gold Standard’ Berg Balance Scale (BBS) in Assessing Fall Risk in the Elderly Population
Hunter Leger, SPT, Reagan Tittle, SPT, Sankela Dowdell, SPT, Cody Thompson, PT, DPT, GCS
Alabama State University, 915 S. Jackson Street Montgomery, AL 36104, United States.
Corresponding Author Details: Cody Thompson, PT, DPT, GCS, DHSc, Associate Professor, Health Sciences, Alabama State University, United States.
Received date: 05th July, 2022
Accepted date: 02nd August, 2022
Published date: 04th August, 2022
Citation: Leger, H., Tittle, R., Dowdell, S., & Thompson, C., (2022). Comparison of the Validity of the Timed Up and Go Test (TUG) and Activities-specific Balance Confidence Questionnaire (ABC) to the ‘Gold Standard’ Berg Balance Scale (BBS) in Assessing Fall Risk in the Elderly Population. J Rehab Pract Res, 3(2):133.
Copyright: ©2022, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Background: Falls are ranked as the leading cause of death from unintentional injury among older adults in the United States. Approximately 25% of the older adults in the U.S. experience a fall each year, which leads to excessive healthcare costs. Falls lead to serious injuries such as broken bones and head injuries hospitalizing 800,000 patients a year [1]. Based on those statistics, identifying fall risk accurately and efficiently using balance assessments is pertinent to fall prevention in the geriatric population. Therefore, the purpose of this study is to compare the validity of the Timed Up and Go Test (TUG) and Activities-Specific Balance Confidence Questionnaire (ABC) to the Berg Balance Scale (BBS) in assessing the risk of falls in the elderly population.
Methods: The systematic review was conducted to highlight balance assessments including the Berg Balance Scale, Timed Up and Go Test, and Activities-specific Balance Confidence Questionnaire. Databases used in the electronic search were PubMed, Google Scholar, MedlinePlus, PTNow, PEDro, and EBSCOhost, and parameters were set at studies published from 2010 to 2021. All relevant studies were reviewed by assessing abstracts for inclusion. Studies in which participants completed and were scored on the three balance assessments were included. All participants completing the tests were required to be 65 years of age or older in order for the respective study to be included.
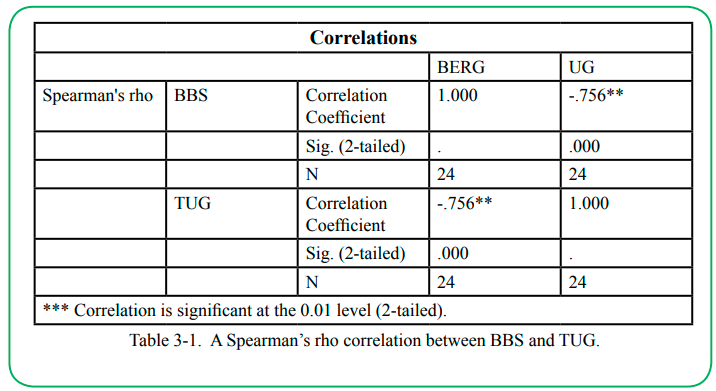
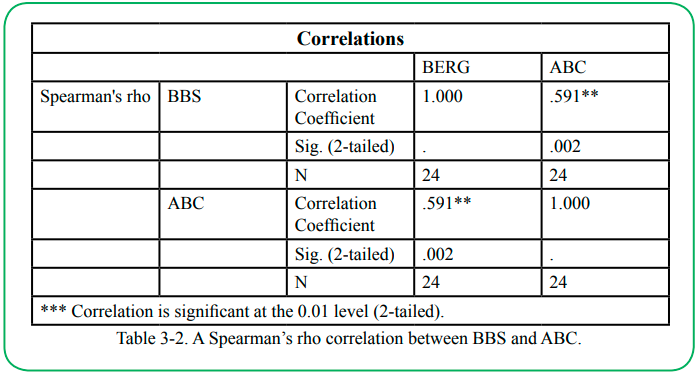
Results: 62 studies were identified for further review after the initial search. After a more extensive screening process, several studies were excluded for reasons such as study design, age of participants, or insufficient testing measures. 16 studies were included for data analysis with a total of 1,376 participants. The validity of the BBS, TUG, and ABC were measured in the 16 studies with strong negative correlation between BBS and TUG (rho (22) = -.756, p < .01), and moderate positive correlation between BBS and ABC (rho (22) = .591, p < .01).
Conclusions: The Timed Up and Go test may be an effective and valid tool assessing balance and a participant’s fall risk. It has been shown to have a strong correlation with the Berg Balance Scale. Meanwhile, the Activities-specific Balance Confidence Questionnaire, a subjective measure, has a moderate correlation with the Berg Balance Scale indicating that it is capable of identifying fall risk but not as accurately or efficiently as the Timed Up and Go Test. This research advocates for the appropriateness of the TUG test and ABC questionnaire, and therefore widens clinicians’ choices of valid balance assessment tools during fall risk examinations.
Keywords: Berg Balance Scale, Timed Up and Go Test, Activities-specific Balance Confidence Questionnaire, Elderly, Balance, Falls
Background
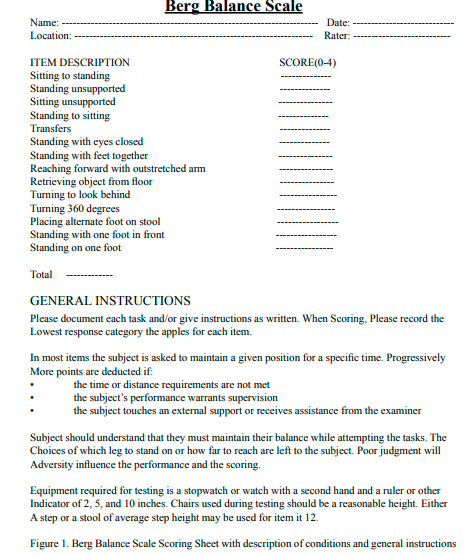
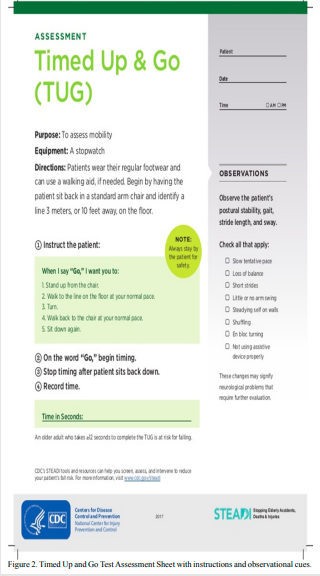
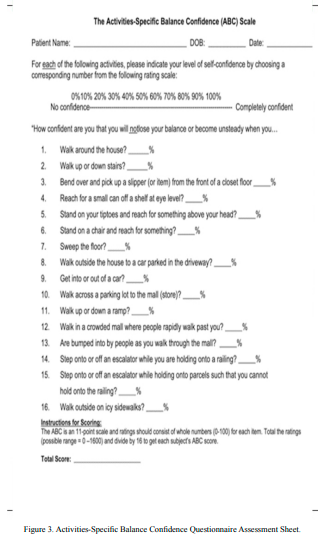
Falls are ranked as the leading cause of death from unintentional injury among older adults in the United States. Approximately 25% of the older adults in the U.S. experience a fall each year, which leads to excessive healthcare costs. Consequently, health-care spending topped $50 billion in 2015 for fall related injuries, 6% of all Medicare payments and 8% of all Medicaid payments [1-3]. Therefore, one would suggest that if this problem is not addressed through improving fall risk assessments and prevention the healthcare cost will continue to climb. Along with an extensive financial burden, falls cause serious injuries for the elderly population. One out of five falls causes a serious injury such as broken bones or a head injury. Also, 3 million older people are treated in the emergency departments for fall-related injuries and 800,000 patients are hospitalized due to a hip fracture or head injury [6]. Every 20 minutes, an older adult dies from a fall [7]. It was reported in 2018 more than 30,000 older adults died from falls, which is approximately 88 older adults every day [8-11]. Based on those statistics, identifying fall risk accurately and efficiently using balance assessments are pertinent to fall prevention in the geriatric population. One would suggest that there is a specific urge for clinicians to improve in identifying fall risk in the geriatric population in order to implement evidence-based interventions to decrease that risk. If the TUG test and the ABC questionnaire are found to be similar in validity to the BBS, both assessments could be used by clinicians in place of the BBS while yielding similar results. This could also allow for improved time management for the clinician and improved patient adherence. The assessments used in this study included the BBS, TUG, and ABC questionnaire. According to Langley and Mackintosh, the Berg Balance Scale shown in (Figure 1) is considered to be the “gold standard” for assessing balance [12-17]. It involves static and dynamic activities with 14 items that are scored from 0-4 with a total score of 56. It takes 15-20 minutes to administer and has a 91% sensitivity and 82% specificity for older adults [29] and the intraclass correlation coefficient (ICC) is .97 [4,5]. The Timed Up and Go test shown in (Figure 2) assesses balance and strength. The participant is instructed to sit in a straight back armchair and on the command “go” the participant stands up, walks 3 meters at a comfortable safe pace, turns, and returns to the chair and sits down [18-20]. The participant should have one trial run before the timed test, however multiple trials may lead to skewed results. The time to administer the test is less than 3 minutes with a cut-off score of greater than 13.5 seconds in community-dwelling adults [31]. The reliability index is ICC=.90 [5] and it has a 87% sensitivity and specificity [30]. Lastly, the Activities-specific Balance Confidence Questionnaire shown in (Figure 3), is a self- report (subjective) measure of a patient’s level of confidence in performing various activities without losing balance or becoming unsteady (balance self-efficacy). It consists of 16 various ambulatory activities, on a 11-point scale, ranging from 0-100% for each of 16 items [21-24]. A score of 0 = no confidence and a score of 100 = complete confidence. 80% equals high level of physical functioning , 50-80% equals moderate level and less than 50% equals low level [25-28]. It has a 84.4% sensitivity & 87.5% specificity, and the cut-off score for fall risk equals less than 67% [16]. The expected outcome for this study is for the findings to demonstrate a strong correlation of the TUG and ABC with the BBS resulting in a significant relationship between the assessments. This could add to the body of knowledge within rehabilitative research on balance assessment tools to detect fall risk in the elderly population. Therefore, the objective of this study is to compare the validity of the Timed Up and Go Test (TUG) and Activities-Specific Balance Confidence Questionnaire (ABC) to the Berg Balance Scale (BBS) in assessing the risk of falls in the elderly population [32-33].
Methods
Search strategy
A literature search was conducted to locate studies that met the eligibility requirements. Databases used in the electronic search were PubMed, Google Scholar, MedlinePlus, PTNow, PEDro, and EBSCOhost, and parameters were set at studies published from 2010 to 2021. Search terms were as follows: Berg Balance Scale, BBS, Timed Up Go, TUG, ABC, elderly, balance. There was no methodological filter used for study design. All relevant studies were reviewed by assessing abstracts for inclusion. The reference lists of each study were also assessed using backwards searching to discover additional relevant articles. The three student researchers conducting this study independently searched the literature and extracted data from the included studies. The final studies included in this review were 100% agreed upon by all three student researchers and the research advisor.
Inclusionary and exclusionary criteria
Studies in which participants completed and were scored on the three balance assessments were included. All participants completing the tests were required to be 65 years of age or older in order for the respective study to be included. All participants also had to be able to complete each test independently. Studies were excluded if all three tests were not completed or if any alternative form of either test was used. Although a methodological filter was not used in the literature search, studies were excluded from this research if they were designed as systematic reviews or meta-analyses. Studies were also excluded if any of the participants had a cognitive impairment that hindered their participation or if they had undergone any form of lower extremity arthroplasty within the 12 weeks prior to completion of the balance assessments.
Data extraction and analysis
The following information was extracted from each study: number, sex, and mean age of participants with standard deviation, and mean BBS, TUG, and ABC scores with standard deviation. The student researchers independently extracted information from the final studies. Since the tests observed in this review included a combination of ordinal and interval data, a Spearman’s rho correlation was utilized to determine the statistical significance of the relationship between tests. Scores of 0 to 0.3 were considered to show no relationship, 0.3 to 0.5 were weak, 0.5 to 0.7 were moderate, and 0.7 and above were strong.
Results
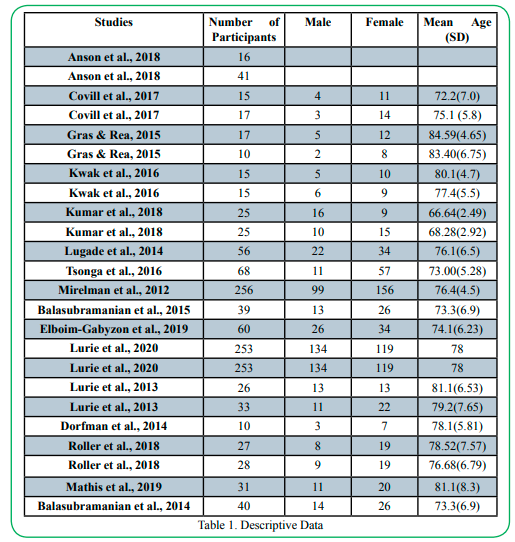
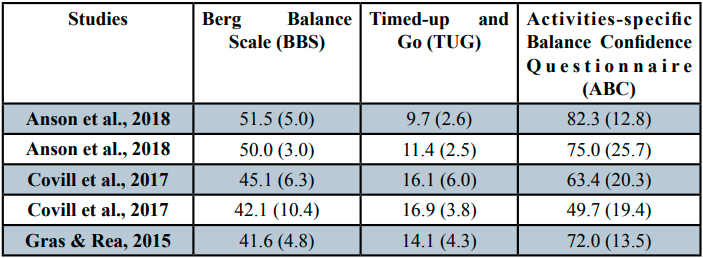
This section will provide an overview of the findings from the systematic review including a summary of the included studies (Table 1) presenting the authors, number of participants, number of male and female participants included in each study, and mean age of participants with standard deviations. The mean scores and standard deviations for the BBS, TUG, and ABC in each included study are provided in (Table 2). The study selection and validity between the balance assessments are also analyzed and reported on.
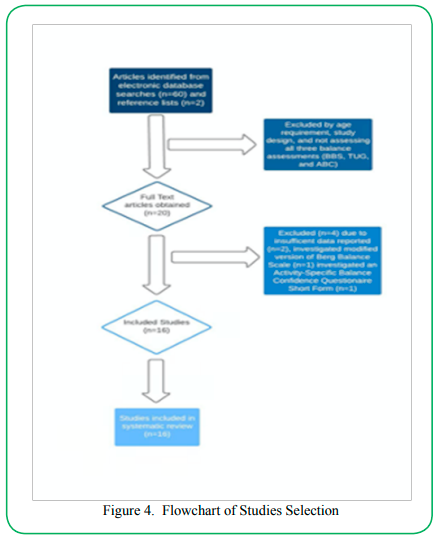
Study Selection
62 studies were identified for further review after the initial search. After a more extensive screening process, several studies were excluded for reasons such as study design, age of participants, or insufficient testing measures. Researchers narrowed it down to 20 studies, and then excluded 4 more: one for utilization of the ABC-Short form, two for insufficient presentation of data, and one for utilization of a modified Berg Balance Scale. 16 studies were included for data analysis with a total of 1,376 participants. The flow of studies is presented in (Figure 4).
BBS vs. TUG
A Spearman’s rho correlation coefficient was calculated for the relationship between participants’ BBS and TUG score. A strong negative correlation was found (rho (22) = -.756, p < .01), indicating a significant relationship between the two variables. Participants who score higher on the Berg tend to complete the TUG in less time. Details can be found in (Table 3-1).
BBS vs. ABC
A Spearman’s rho correlation coefficient was also calculated for the relationship between participants’ BBS and ABC scores. A moderate positive correlation was found (rho (22) = .591, p < .01), indicating a significant relationship between the two variables. Participants who score higher on the Berg tend to have higher confidence in not losing their balance during activities on the ABC Questionnaire. Details can be found in (Table 3-2).
Discussion
The purpose of this study was to compare the validity of the TUG and ABC to the BBS in assessing fall risk in the elderly population. The researchers hypothesized, when compared, that the TUG and ABC would yield a strong correlation and significant relationship with the BBS. The results of the TUG against the BBS confirmed the hypothesis, as a significant relationship and strong correlation of (-.756) was found. The ABC also was found to have a significant relationship with the BBS but only yielded a moderate correlation of (.591), which did not fully meet the acceptance criteria of the hypothesis. Overall, the results of this study suggest both the TUG and ABC are appropriate in assessing fall risk in the elderly population when compared to the “gold standard” BBS.
There were several limitations found within the current study. The main limitation of this study was the inability to monitor testing. The researchers suspect issues with interrater and intrarater reliability were present. Interrater reliability being that quantifications could not be made regarding administrators performing testing in the same manner, and intrarater reliability being that quantifications could not be made on the consistency of each administrator’s performance throughout the study. Due to the ABC being purely a subjective test, the inability to ensure patient honesty when filling out the questionnaire became a limitation. Along with this, patients may have answered based on overconfidence or under confidence and, in general, may have had limited insight into their overall balance abilities. The researchers also found many inconsistencies in the way the TUG was administered, and therefore were not able to identify and further inspect the consistency of the TUG criteria that was used throughout the study.
In today’s aging society, fall prevention is likely one of the most important assets in the medical world. In order to provide the best and most appropriate care, clinicians must have adequate tools to assess which older adults are more likely to experience falls and why. The TUG, which takes approximately three minutes to complete, may be used in the place of more invasive and time-consuming tests, such as the BBS, to yield similar results. The ABC is a simple subjective test that can be completed by the patient and may in fact yield similar results to an objective measure such as the BBS.
Future research on the proposed topic could be beneficial by expanding the body of knowledge available for clinicians regarding adequate tools for assessing fall risk. One recommendation the researchers propose is conducting a more detailed and consistent controlled trial. Researchers performing testing may improve the reliability of testing, particularly interrater reliability, by decreasing the number of administrators and ensuring a standardized method of testing is being used. Though this study is highly generalizable among the geriatric population, which meets the intended purpose, the researchers suggest future research may benefit from testing more specific diagnoses to determine if the findings are applicable to each, therefore incorporating diagnosis homogeneity into the research.
Conclusion
The TUG and ABC each prove to be valid in assessing fall risk in the elderly population and are advantageous because both are time-efficient and easy to administer with very little equipment required. This research advocates for the appropriateness of the TUG test and the ABC questionnaire, and therefore widens clinicians’ choices of valid balance assessment tools during fall risk examinations.
Acknowledgement
The authors would like to thank our research advisor, Cody Thompson, PT, DPT, GCS, and Ladarius Woods, PT, DPT, PhD for his assistance in reviewing the paper and data analysis.
Conflict of interest:
The authors declare no conflict of interest.
References
American Physical Therapy Association (APTA), (2018). Study: falls among US adults 65 and older cost $50 billion in 2015. https://www.apta.org/news/2018/03/09/study-falls-among-us-adults-65-and-older-cost-$50-billion-in-2015View
Anson, E., Thompson, E., Odle, B. L., Jeka, J., Walls, Z. F., & Panus, P. C. (2019). The influences of age, obesity and adverse drug effects on balance and mobility testing scores in ambulatory older adults. Journal of Geriatric Physical Therapy, 41(4), 218-229. doi:10.1519/JPT.0000000000000124.View
Balasubramanian, C. K. (2015). The Community Balance and Mobility Scale alleviates the ceiling effects observed in the currently used gait and balance assessments for the community-dwelling older adults. Journal of Geriatric Physical Therapy, 38(2), 78-89. doi:10.1519/JPT.0000000000000024View
Balasubramanian, C. K., Boyette, A., & Wludyka, P. (2015). How well do functional assessments of mobility and balance discriminate fallers and recurrent fallers from non-fallers among ambulatory older adults in the community? Physiotherapy Canada, 67(2), 184–193. doi:10.3138/ptc.2014-19 View
Berg, K. O., Maki, B. E., Williams J. I., Holliday, P. J., & Wood-Dauphinee, S. L. (1992). Clinical and laboratory measures of postural balance in an elderly population. Archives of Physical Medicine and Rehabilitation, 73(11), 1073-1080. https:// pubmed.ncbi.nlm.nih.gov/1444775/View
Centers for Disease Control and Prevention. (2017). Facts About Falls. https://www.cdc.gov/falls/facts.htmlView
Centers for Disease Control and Prevention. (2017). Fact Sheet: Falls are a Major Threat for Your Patients. https://www.cdc. gov/steadi/pdf/STEADI-FactSheet-MajorThreat-508.pdfView
Centers for Disease Control and Prevention. (2020). Fact Sheet: Older Adult Falls - A Growing Problem That can be Prevented. https://www.cdc.gov/steadi/pdf/STEADI_ ClinicianFactSheet-a.pdfView
Covill, L. G., Utley, C., & Hochstein, C. (2017). Comparison of Ai Chi and impairment-based aquatic therapy for older adults with balance problems: A clinical study. Journal of Geriatric Physical Therapy, 40(4), 204-213. doi:10.1519/ JPT.0000000000000100View
Dorfman, M., Herman, T., Brozgol, M., Shema, S., Weiss, A., Hausdorff, J. M., & Mirelman, A. (2014). Dual-task training on a treadmill to improve gait and cognitive function in elderly idiopathic fallers. Journal of Neurologic Physical Therapy, 38(4), 246-253. doi:10.1097/NPT.0000000000000057View
Elboim–Gabyzon, M., Agmon, M., Azaiza, F. (2019). Psychometric properties of the Arabic version of the Activities-Specific Balance Confidence (ABC) scale in ambulatory, community-dwelling, elderly people. Clinical Interventions in Aging, 14, 1075-1084. doi:10.2147/CIA.S194777View
Gras, L. (2015). Improving balance of older adults by walking, education , and Wii™ Bowling. Jacobs Journal of Physical Rehabilitation Medicine, 1(1), 1-5. https://jacobspublishers.com/ uploads/article_pdf/45/scientific_45_628_25052019040352. pdfView
Hartley, G., Kirk-Sanchez, N. (2013). Fall risk in community-dwelling elders. American Physical Therapy Association (APTA).https://www.apta.org/patient-care/evidence-based-practice-resources/clinical-summaries/fall-risk-in-community-dwelling-elder
Kumar, C., Chaubey, V., Pathan, N., & Aswar, V. M. (2018). Wii Fit plus balance board to improve balance, mobility and confidence in elderly fallers: A randomized clinical trial. Scholars Journal of Applied Medical Sciences (SJAMS), 6(12), 4715-4724. doi:10.21276/sjams.2018.6.12.17
Kwak, C. J., Kim, Y. L., & Lee, S. M., (2016). Effects of elastic-band resistance exercise on balance, mobility and gait function, flexibility and fall efficacy in elderly people. The journal of Physical Therapy Science, 28(11), 3189-3196. doi:10.1589/ jpts.28.3189View
Lajoie, Y., & Gallagher, S. P. (2004). Predicting falls within the elderly community: Comparison of postural sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence (ABC) Scale for comparing fallers and non-fallers. Archives of Gerontology and Geriatrics, 38(1), 11-26. doi:10.1016/s0167-4943(03)00082-7. View
Langley, F. A., & Mackintosh, S. F. H. (2007). Functional balance assessment of older community dwelling adults: A systematic review of the literature. The Internet Journal of Allied Health Sciences and Practice, 5(4). https://nsuworks. nova.edu/cgi/viewcontent.cgi?article=1174&context=ijahspView
Looking for the activities-specific balance confidence (abc) scale form? Download it for free! (n.d.). Retrieved March 30, 2021, from https://www.formsbank.com/template/205748/the-activities-specific-balance-confidence-abc-scale-form.htm
Lugade, V., Lin, V., Farley, A., & Chou, L. S. (2014). An artificial neural network estimation of gait balance control in the elderly using clinical evaluations. PLoSONE, 9(5), e97595. doi:10.1371/journal.pone.0097595View
Lurie, J. D., Zagaria, A. B., Ellis, L., Pidgeon, D., Gill-Body, K. M., Burke, C., Armbrust, K., Cass, S., Spratt, K. F., & McDonough, C. M. (2020). Surface perturbation training to prevent falls in older adults: A highly pragmatic, randomized control trial. Physical Therapy, 100(7), 1153-1162. doi:10.1093/ ptj/pzaa023View
Lurie, J. D., Zagaria, A. B., Pidgeon, D. M., Forman, J. L., & Spratt, K. F. (2013). Pilot comparative effectiveness study of surface perturbation treadmill training to prevent falls in older adults. BMC Geriatrics, 13(49). http://www.biomedcentral. com/1471-2318/13/49View
Mathis, R. A., Taylor, J. D., Odom, B. H., & Lairamore, C. (2019). Reliability and validity of the Patient-Specific Functional Scale in community-dwelling older adults. Journal of Geriatric Physical Therapy, 42(3), E67-E72. doi:10.1519/ JPT.0000000000000188View
Mettler-Toledo International Inc. all rights reserved. (2020, April 27). Balances and scales. Retrieved March 30, 2021, from https://www.mt.com/us/en/home/products/Industrial_ Weighing_Solutions/balances_scales_2.html?cmp=sea_560401 27&SE=BING&Campaign=MT_IND-LAB_EN_US &Adgroup=Balances%2FScales&bookedkeyword= %2Bscale+%2Bbalance&matchtype=b&adtext=777 21883739700&placement=Bing-not_available&netw ork=o&kclid=_k_c5d900e9229113e547f0608b4da09a2d_ k_&msclkid=c5d900e9229113e547f0608b4da09a2d
Mirelman, A., Herman, T., Brozgol, M., Dorfman, M., Sprecher, E., Schweiger, A., Giladi, N., & Hausdorff, J. M. (2012). Executive function and falls in older adults: New findings from a five-year prospective study link fall risk to cognition. PLoS ONE, 7(6), e40297. doi:10.1371/journal.pone.0040297View
Myers, A. (1998). Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) Scale. J Gerontol Med Sci, 1998. 53A(4), M287-M294.View
News Now Staff, (2019). Senate reports calls for more emphasis on falls prevention. American Physical Therapy Association (APTA). https://www.apta.org/news/2019/10/21/senate-report-calls-for-more-emphasis-on-falls-prevent
Roller, M., Kachingwe, A., Beling, J., Ickes, D. M., Cabot, A., & Shrier, G. (2017). Pilates Reformer exercises for fall risk reduction in older adults: A randomized controlled trial. Journal of Bodywork & Movement Therapies, 22(4), 983-998. http:// dx.doi.org/10.1016/j.jbmt.2017.09.004View
SDGWEP Follow. (2018, January 23). Tug test print. Retrieved March 30, 2021, from https://www.slideshare.net/SDGWEP/ tug-test-print-86594236
Shumway-Cook, A., Baldwin, M., Polissar, N. L., & Gruber, W. (1997). Predicting the probability for falls in community-dwelling older adults. Physical Therapy, 77(8), 812-819. doi:10.1093/ptj/77.8.812.View
Shumway-Cook, A., Brauer, S., & Woollacott, M. (2000). Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical Therapy, 80(9), 896-903. https://pubmed.ncbi.nlm.nih.gov/10960937View
Timed up and go. Shirley Ryan AbilityLab. (n.d.). https://www. sralab.org/rehabilitation-measures/timed-and-goView
Top 10 Elderly balance exercises to improve balance and COORDINATION: Updated for 2021. (2021, March 10). Retrieved March 26, 2021, from https://aginginplace.org/ top-10-elderly-balance-exercises-to-improve-balance-and-coordination/View
Tsonga, T., Michalopoulou, M., Kapetanakis, S., Giovannopoulou, E., Malliou, P., Godolias, G. & Soucacos, P. (2016). Reduction of falls and factors affecting falls a year after total knee arthroplasty in elderly patients with severe knee osteoarthritis. The Open Orthopaedics Journal, 10(1), 522-531. doi:10.2174/1874325001610010522View