Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-164
https://doi.org/10.33790/jrpr1100164Research Article
Fall Risk Prediction in Adults Using Durable Medical Equipment: A Comparative Analysis of STEADI and 3-Key Question STEADI
Karen Probst, and Constance Lewis*
Gannon University, 109 University Square, Erie, PA 16541, United States.
Corresponding Author Details: Constance Lewis, Assistant Professor, Department of Physical Therapy Program, Gannon University, 109 University Square, Erie, PA 16541, United States.
Received date: 08th March, 2025
Accepted date: 26th April, 2025
Published date: 28th April, 2025
Citation: Probst, K., & Lewis, C., (2025). Fall Risk Prediction in Adults Using Durable Medical Equipment: A Comparative Analysis of STEADI and 3-Key Question STEADI. J Rehab Pract Res, 6(1):164.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Falls among older adults are a leading cause of morbidity, mortality, and increased healthcare costs. The Centers for Disease Control and Prevention’s (CDC) Stopping Elderly Accidents, Deaths & Injuries (STEADI) initiative provides fall risk screening tools, including the full 12-item STEADI and its three-item key-question counterpart (3KQ-STEADI). However, limited research has evaluated these tools in populations using durable medical equipment (DME), a subgroup at elevated fall risk. This study examines the predictive validity of the STEADI and 3KQ-STEADI self-assessment questionnaires in a cohort receiving durable medical equipment. A total of 118 participants were followed for six months after DME issuance, and fall occurrences were recorded. Results indicate that both assessments demonstrate high sensitivity (97.4%) but low specificity (STEADI: 8.5%; 3KQ-STEADI: 2.8%), suggesting that while effective in identifying at-risk individuals, they over-classify fall risk. These findings highlight the need for refined risk stratification methods in clinical practice.
Keywords: Falls, Fall Risk, Fall Prevention, Fall Risk Screening, STEADI, Durable Medical Equipment, Community, Elderly, Geriatrics
Introduction
Falls among older adults remain a major public health concern, representing the leading cause of injury-related mortality worldwide [1]. In the United States, approximately one in three adults aged 65 and older experiences a fall each year, accounting for an estimated 36 million falls and eight million fall-related injuries [2]. These events contribute significantly to healthcare utilization and economic burden, with fall-related medical costs exceeding $50 billion annually [3] and projected to surpass $100 billion by 2030 [4]. Given the rising proportion of older adults [5], comprehensive fall prevention strategies are imperative.
In response, the Centers for Disease Control and Prevention
(CDC) developed the Stopping Elderly Accidents, Deaths & Injuries
(STEADI) initiative to integrate fall risk screening, assessment, and
intervention into routine healthcare practice [6]. The STEADI toolk
it includes evidence-based screening tools such as the 12-item Stay
Independent questionnaire and a three-key-question (3KQ) version,
followed by structured clinical assessments of gait, strength, balance,
medication use, vision, and environmental hazards [7,8]. The Stay
Independent questionnaire covers fall risk factors such as balance,
medication use, and previous fall history, classifying individuals as at
risk for falls if they score ≥four out of 12. However, a score of
A critical aspect of fall prevention research is determining STEADI’s predictive validity—its ability to accurately identify older adults at risk for future falls. Several studies have evaluated the algorithm’s accuracy in prospective cohorts. Nithman and Vincenzo [11] found that in a sample of 77 older adults (39 community-dwelling, 38 residing in a retirement facility), STEADI had a sensitivity of 68.4% and a specificity of 44.9% in predicting 6-month falls, with better performance in community-dwelling participants (sensitivity ~73– 80%). Similarly, Loonlawong et al. [12] studied a 12-month cohort of 480 community-dwelling Thai older adults and reported that the 3KQ had a sensitivity of 93.9% and a specificity of 75%, whereas the 12-item tool achieved 77.7% sensitivity and 88.0% specificity. Meanwhile, Burns et al. [13] analyzed a U.S. sample of 1,563 older adults over 11 months, finding that the 3KQ demonstrated 68.7% sensitivity, while the 12-item questionnaire achieved 55.7% sensitivity and 75.9% specificity. Despite variations in population characteristics and methodology, these findings suggest that STEADI effectively stratifies fall risk, albeit with moderate specificity.
A crucial limitation of these studies is the lack of specific analysis on older adults utilizing durable medical equipment (DME) such as canes, walkers, and wheelchairs. Lohman et al. [14] emphasized the need for further validation of STEADI within a nationally representative sample, particularly in subgroups at higher risk of falls due to mobility impairments. Additionally, Sri-On et al. [15] found that adding a question about DME use improved fall prediction accuracy, reinforcing the need for research focused on this subgroup. Lin et al. [16] expanded upon previous findings by assessing STEADI’s predictive performance across different clinical settings and highlighted the importance of tailoring fall prevention interventions to mobility-limited populations.
To date, no study has specifically examined STEADI’s predictive validity in individuals receiving DME. Given that mobility aids are frequently prescribed following falls and may be associated with increased fall risk due to improper use or declining function [17,18], targeted validation is necessary to refine STEADI’s clinical application for high-risk older adults. Addressing this gap, the present study evaluates the predictive validity of STEADI’s 12-item assessment and its three-item abbreviated version among individuals using DME, with the goal of improving fall risk prediction and enhancing coordination between clinical and community-based fall prevention efforts.
Methods
This study employed a convergent parallel design to evaluate the concordance between the full STEADI 12-item assessment and the three-item abbreviated version (3KQ) in predicting fall risk among individuals receiving durable medical equipment. A convergent parallel design was chosen to allow for simultaneous collection and comparison of quantitative fall risk assessment data and self-reported fall occurrences, enhancing the study’s robustness and validity.
Participant Recruitment & Sampling Participants were recruited using a convenience sampling approach at a local nonprofit equipment exchange program during DME pick-up. Eligible participants were older adults (individuals aged 65 years or older per CDC), received DME from the program, and provided reliable contact information. Exclusion criteria included individuals who were younger than 65 years of age, unable to provide verbal informed consent or could not be reached for follow-up.
During the study period, a total of 255 individuals received gently used durable medical equipment through the program. Of these, 118 met the inclusion criteria and agreed to participate in the followup study. Prior to data collection, all participants provided verbal informed consent, which included an explanation of the study’s purpose, procedures, and voluntary nature. Among those excluded, 44 individuals were under the age of 65, while the remaining 93 were excluded due to providing unreliable contact information, being unable to recall fall history, or declining to give the required verbal consent.
Data Collection Procedures Upon receiving DME, both the 12- item STEADI and 3KQ-STEADI questionnaires were completed. These self-report surveys were administered by non-profit staff via a hand-held tablet with responses exported to an Excel document along with demographic information, including age, zip code, income level, type of insurance, and contact information, as well as the type of DME received. Demographic data was collected by the non-profit organization as part of their standard procedures.
Follow-up and Fall Tracking All eligible participants were contacted via telephone six months post-DME receipt to determine if they had experienced any falls during the intervening period, severity of falls was not inquired upon. Fall occurrence was defined as any unintentional event resulting in a person coming to rest on the ground or a lower level, with or without injury. Participants were asked structured questions to minimize recall bias, ensuring consistency in self-reported falls.
Data Management & Statistical Analysis Data from both fall risk assessments (categorized as fall risk or non-fall risk) and participant reports of falls were analyzed the data using Microsoft Excel for Microsoft 365 (Version 2503). To understand how well the STEADI and 3KQ-STEADI assessments aligned, several statistical methods were employed. Sensitivity and specificity were calculated to determine the accuracy of each assessment in predicting falls. The relationship between the fall risk classifications and whether participants actually experienced falls was examined using chi-square tests. Additionally, a focused analyses on subgroups of participants was conducted, based on their age and the type of durable medical equipment they used, to see if the assessments' ability to predict fall risk differed across these groups.
Results
A total of 118 participants who received durable medical equipment (DME) and completed the six-month follow-up telephone interview were included in the analysis. Data was compiled using Microsoft Excel for Microsoft 365 (Version 2503) and statistical analyses were conducted using built-in Excel functions. The mean age of participants was 73.4 years (SD = 5.8), with 58.5% identifying as female. Income distribution varied, with 47.3% reporting low-income status, and the majority (68.6%) had Medicare as their primary insurance. Participants resided in a range of zip codes, predominantly from urban areas (72.9%) compared to rural (27.1%).
Fall Incidence and Predictive Validity Of the 118 participants, 41 (34.7%) experienced a fall during the follow-up period. Fall incidence was similar between the two questionnaires: 42.7% of participants identified as at risk by the full 12-item STEADI experienced a fall, while 43.62% of participants identified as at risk by the 3KQSTEADI experienced a fall.
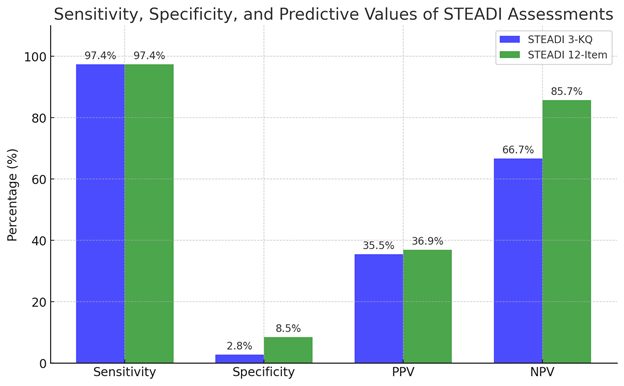
Diagnostic properties of both questionnaires were evaluated based on their ability to predict falls. The sensitivity was identical for both questionnaires at 97.4%, as shown in Figure 1. These results indicate that both self-report surveys were highly sensitive in identifying individuals who experienced a fall during the six-month period. However, both questionnaires exhibited low specificity: 8.5% for the full STEADI and 2.8% for the 3KQ-STEADI (Figure 1). This suggests that while the full STEADI had slightly better specificity, both tools tended to over-identify individuals as at risk, including those who did not experience a fall.
The positive predictive value (PPV) of the full STEADI 12-item assessment was slightly higher (36.9%) compared to the 3KQSTEADI (35.5%) (Figure 1). This suggests that the full STEADI tool had a marginally greater probability of correctly identifying individuals who actually experienced a fall during the followup period. Conversely, the negative predictive value (NPV) was notably higher for the 12-item STEADI (85.7%) compared to the 3KQ-STEADI (66.7%) (Figure 1), indicating that the full 12-item STEADI questionnaire was significantly more effective at correctly ruling out individuals who did not experience falls.
Agreement Between STEADI and 3KQ-STEADI Agreement between the full 12-item STEADI and 3KQ-STEADI questionnaires was evaluated using kappa statistics, which yielded a moderate agreement (κ = 0.57, p < 0.001). This suggests that while both tools identified similar fall risk classifications, there were instances where classification differed. A detailed breakdown of classification concordance is shown in Figure 1.
Subgroup Analysis Subgroup analysis revealed that fall risk prediction varied by age group. Participants aged 75 and older were more likely to experience falls (42.1%) compared to those aged 65-74 (29.8%), although this difference did not reach statistical significance (p = 0.08). Income level and insurance type did not significantly influence fall occurrence.
ChatGPT generated (OpenAI, March 2025 version) which visualized sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) based on data manually provided by the researchers from the study cohort. The underlying data were calculated using participant responses and follow-up outcomes; ChatGPT was used solely for figure generation.
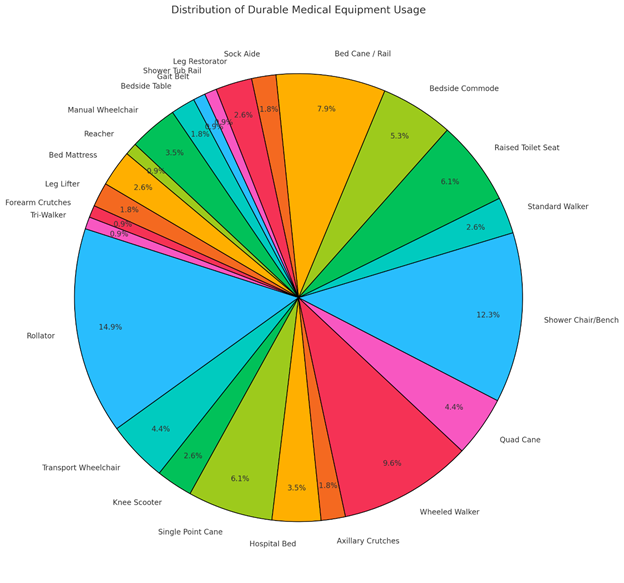
Regarding type of durable medical equipment acquired, the most commonly received items were rollator walkers (14.9%) and shower chairs/benches (12.3%) (Figure 2). No statistically significant correlation was found between the type of DME received and the incidence of falls (p = 0.73), indicating that the type of mobility aid did not appear to influence fall occurrence within the study population.
ChatGPT generated (OpenAI, March 2025 version), based on frequency data compiled by the researchers on the type of DME distributed to participants. The figure was produced using a script generated by ChatGPT to display the proportions visually; the data input was entirely researcher-derived.
Summary of Key Findings The study revealed that both fall risk assessments demonstrated a strong ability to identify individuals who would go on to experience a fall, showing a high sensitivity of 97.4%. However, their ability to correctly identify those who would not fall (specificity) was low, although the full STEADI assessment performed marginally better in this regard. When comparing the agreement between the full STEADI and the abbreviated 3KQSTEADI, a moderate level of consistency was observed (κ = 0.57, p < 0.001). While older participants, those aged 75 and above, did experience falls more frequently than younger individuals, this difference did not reach statistical significance within the sample. Furthermore, the type of durable medical equipment used by participants did not appear to be significantly related to whether they experienced a fall. The number of participants who did not complete the follow-up was small, suggesting that this loss did not substantially skew the overall results. Taken together, these findings suggest that the 3KQ-STEADI could be a useful tool for quickly identifying individuals at potential risk of falling but also underscore the ongoing need to enhance accuracy in identifying those who are truly at low risk.
Figure Generation and Data Visualization Figures 1 and 2 were generated using ChatGPT [19], a large language model capable of scripting data visualization code and formatting output based on tabulated inputs. For Figure 1, raw sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) metrics were manually entered into ChatGPT, which then generated a Python script to produce the graph. For Figure 2, frequency data for each type of durable medical equipment (DME) distributed in the study was similarly entered, and ChatGPT generated the corresponding pie chart. All underlying data were researcher-provided, and no data analysis or statistical inference was performed by the model. Figures were verified for accuracy and consistency with study results. No manual adjustments were made to the figures beyond exporting them as high-resolution images for publication.
Discussion
This study provides important insights into the predictive validity of the STEADI and 3KQ-STEADI questionnaires in identifying fall risk among older adults receiving durable medical equipment. The observed high sensitivity for both tools aligns with prior studies highlighting their effectiveness in detecting individuals at risk of falling [16]. In this cohort, the full STEADI and 3KQ-STEADI achieved sensitivity rates of 89.74% and 87.18%, respectively, suggesting both tools are useful for screening populations in which early identification is critical.
However, specificity remained low (19.48% for 12-item STEADI; 21.33% for 3KQ-STEADI), indicating a tendency to over-classify fall risk. This finding is particularly important in clinical practice, where false positives may lead to unnecessary interventions and strain on healthcare resources. The STEADI algorithm's broad criteria, while effective for capturing at-risk individuals, may not sufficiently differentiate between those with transient versus significant risk factors. Moreover, because all participants in this study received DME, perceived vulnerability may have influenced perceived fall risk, contributing to reduced specificity [20].
It is worth considering whether STEADI’s sensitivity and specificity may vary among perceived fall risk populations. The high sensitivity observed could reflect the tool’s utility in general risk detection, whereas specificity might improve in more narrowly defined clinical populations (e.g., those with certain comorbidities or mobility limitations). If STEADI is best interpreted as a sensitivitydriven screening tool, its value lies in minimizing missed cases, especially when used as an entry point for more precise, targeted assessments. These results suggest an opportunity for future research to investigate whether combining STEADI with tools emphasizing specificity could create a more robust, tiered fall risk assessment protocol.
Implications for Clinical Practice Given its high sensitivity, the STEADI framework remains a valuable first-line tool for identifying older adults at risk of falls—particularly those who may not otherwise seek preventive care. In populations with mobility impairments or DME use, STEADI screening can trigger early referral and intervention. Clinicians, however, should be mindful of the tool’s moderate specificity and consider supplementing results with additional individualized assessments, as recommended by the CDC algorithm.
Integrating contextual factors—such as fall history, medication use, or physiological conditions—can enhance predictive accuracy. Functional tests (e.g., gait assessment), medication reviews, cognitive screenings, and comprehensive evaluations by physical or occupational therapists may be critical for refining care plans. Interventions should be tailored to the individual and may include targeted therapies, home modifications, education, and long-term management strategies [21]. Importantly, this study reaffirms that issuing DME alone is not a standalone fall prevention strategy.
Subgroup Analysis No significant relationship was found between the type of DME issued and fall incidence. This suggests that while DME can play a role in fall prevention, its effectiveness may depend on factors such as appropriate fit, usage training, comorbidity profiles, and follow-up care. Future studies should further investigate whether specific device types interact with patient characteristics to influence fall outcomes.
Limitations This study has several limitations. First, the sample was limited to individuals obtaining DME from a local nonprofit program, which may limit generalizability. Second, fall outcomes were based on self-reported data, introducing the potential for recall bias. Third, comorbidities and psychosocial factors influencing fall risk were not measured. Future work would benefit from objective fall tracking (e.g., wearable devices or electronic health record data) and broader data collection on clinical and environmental influences.
Future Directions To refine fall risk prediction, future research should explore integrating STEADI with other tools that emphasize specificity, forming a layered approach to risk stratification. Examination of sensitivity and specificity among subgroups, inclusive of how cognition, mental health, environmental hazards, and vestibular function impact STEADI’s performance, may guide more personalized interventions. Investigating the effectiveness of multimodal and individualized treatment strategies [22], including therapy, caregiver education, and home safety optimization, remains essential, particularly among older adults using DME.
Conclusion
This study supports the use of the STEADI and 3KQ-STEADI tools as sensitive fall risk screening instruments for older adults, including those using durable medical equipment. While the tools demonstrate high sensitivity, their limited specificity highlights the need for supplementary assessments to guide clinical decisions. Future efforts should focus on refining risk models and exploring integrated, patient-centered strategies that enhance fall prevention outcomes across diverse older adult populations.
Competing Interests:
The authors declare that they have no competing interests.
List of Abbreviations
Stopping Elderly Accidents, Deaths, & Injuries (STEADI)
Durable Medical Equipment (DME)
3-key question Stopping Elderly Accidents, Deaths, & Injuries (3KQ-STEADI)Ethical Considerations The study received Institutional Review Board (IRB) approval to ensure ethical compliance. All data were anonymized before analysis to protect participant confidentiality, and access was restricted to authorized research personnel only.
Acknowledgement
The authors would like to acknowledge Chosen Inc. for their support and collaboration throughout the duration of this project. Their assistance with community outreach, participant engagement, and program implementation was instrumental to the success of this study.
References
James, S. L., Lucchesi, L. R., Bisignano, C., Castle, C. D., Dingels, Z. V., Fox, J. T., … Murray, C. J. L. (2020). The global burden of falls: global, regional, and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention, 26(Suppl 1), i3–i11. View
Moreland, B., Kakara, R., & Henry, A. (2020). Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years — United States, 2012–2018. MMWR Morbidity and Mortality Weekly Report, 69(27), 875-881. View
Florence, C. S., Bergen, G., Atherly, A., Burns, E., Stevens, J., & Drake, C. (2018). Medical Costs of Fatal and Nonfatal Falls in Older Adults. Journal of the American Geriatrics Society, 66(4), 693–698. View
Houry, D., Florence, C., Baldwin, G., Stevens, J., & McClure, R. (2016). The CDC Injury Center's response to the growing public health problem of falls among older adults. American Journal of Lifestyle Medicine, 10(1), 74-77. View
Healthy People 2030. (n.d.). U.S. Department of Health and Human Services. View
Stevens, J. A., & Phelan, E. A. (2013). Development of STEADI: a fall prevention resource for health care providers. Health Promotion Practice, 14(5), 706–714. View
Moncada, L. V. V., & Mire, L. G. (2017). Preventing falls in older persons. American Family Physician, 96(2), 240-247. View
Rubenstein, L. Z., & Josephson, K. R. (2002). The epidemiology of falls and syncope. Clinics in Geriatric Medicine, 18(2), 141– 158. View
Ambrose, A. F., Paul, G., & Hausdorff, J. M. (2013). Risk factors for falls among older adults: a review of the literature. Maturitas, 75(1), 51–61. View
Karani, M. V., Haddad, Y., & Lee, R. (2016). The role of pharmacists in preventing falls among America’s older adults. Frontiers in Public Health, 4, 250. View
Nithman, R. W., & Vincenzo, J. L. (2019). How steady is the STEADI? Inferential analysis of the CDC fall risk toolkit. Archives of Gerontology and Geriatrics, 83, 185-194. View
Loonlawong, S., Limroongreungrat, W., Rattananupong, T., Kittipimpanon, K., Saisanan Na Ayudhaya, W., & Jiamjarasrangsi, W. (2022). Predictive validity of the Stopping Elderly Accidents, Deaths & Injuries (STEADI) program fall risk screening algorithms among community-dwelling Thai elderly. BMC Medicine, 20(1), 78. View
Burns, E. R., Lee, R., Hodge, S. E., Pineau, V. J., Welch, B., & Zhu, M. (2022). Validation and comparison of fall screening tools for predicting future falls among older adults. Archives of Gerontology and Geriatrics, 101, 104713. View
Lohman, M. C., Crow, R. S., DiMilia, P. R., Nicklett, E. J., Bruce, M. L., & Batsis, J. A. (2017). Operationalization and validation of the STEADI fall risk algorithm in a nationally representative sample. Journal of Epidemiology and Community Health, 71(12), 1191-1197. View
Sri-On, J., Tirrell, G. P., Kamsom, A., Marill, K. A., Shankar, K. N., & Liu, S. W. (2018). A High-yield Fall Risk and Adverse Events Screening Questions From the Stopping Elderly Accidents, Death, and Injuries (STEADI) Guideline for Older Emergency Department Fall Patients. Academic Emergency Medicine. 25(8), 927–938. View
Lin, C. C., Meardon, S., & O'Brien, K. (2022). The predictive validity and clinical application of STEADI for fall risk screening. Advances in Geriatric Medicine and Research, 4(3), e220008. View
Liu H. H. (2009). Assessment of rolling walkers used by older adults in senior-living communities. Geriatrics & Gerontology International, 9(2), 124–130. View
Bateni, H., & Maki, B. E. (2005). Assistive devices for balance and mobility: Benefits, demands, and adverse consequences. Archives of Physical Medicine and Rehabilitation, 86(1), 134- 145. View
OpenAI. (2025). ChatGPT (March 2025 version) [Large language model]. OpenAI. View
Gell, N. M., Wallace, R. B., LaCroix, A. Z., Mroz, T. M., & Patel, K. V. (2015). Mobility device use in older adults and incidence of falls and worry about falling: findings from the 2011-2012 national health and aging trends study. Journal of the American Geriatrics Society, 63(5), 853–859. View
Hopewell, S., Adedire, O., Copsey, B. J., Boniface, G. J., Sherrington, C., Clemson, L., … Lamb, S. E. (2018). Multifactorial and multiple component interventions for preventing falls in older people living in the community. The Cochrane database of systematic reviews, 7(7), CD012221. View
Sherrington, C., Fairhall, N. J., Wallbank, G. K., Tiedemann, A., Michaleff, Z. A., Howard, K., … Lamb, S. E. (2019). Exercise for preventing falls in older people living in the community. The Cochrane database of systematic reviews, 1(1), CD012424. View