Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-166
https://doi.org/10.33790/jrpr1100166Case Report
Addressing Body Awareness in Rehabilitation: A case Report
Brigitte Belanger, DSc, OTR/L1*, Carlene Rimes, OTR/L2, Paul Arthur, PhD, OTR/L1, and Ahmed Elokda, PT, PhD, FAACVPR1
1 Department of Rehabilitation Sciences - Occupational Therapy Program, Florida Gulf Coast University, Fort Myers, FL,United States.
2 Mobile Rehab LLC, Concierge Outpatient Therapy, Naples, FL, United States.
Corresponding Author Details: Brigitte Belanger, DSc, OTR/L, Associate Professor, Department of Rehabilitation Sciences - Occupational Therapy Program, Florida Gulf Coast University, Fort Myers, FL, United States.
Received date: 03rd April, 2025
Accepted date: 02nd May, 2025
Published date: 05th May, 2025
Citation: Belanger, B., Rimes, C., Arthur, P., & Elokda, A., (2025). Addressing Body Awareness in Rehabilitation: A case Report. J Rehab Pract Res, 6(1):166.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
This case report describes an increasingly observed clinical phenomenon and presents a novel rehabilitative approach via a comprehensive body awareness protocol designed to improve balance, postural stability, and motor performance to enhance functional performance and reduce falls. A client diagnosed with a neurodegenerative disease was referred for occupational therapy secondary to increased falls and a decreased ability to perform Activities of Daily Living (ADLs) safely. The client had been participating in a rigorous exercise regimen to remain functionally active but despite his best efforts he was losing the ability to perform functional tasks. Within six (6) weeks of participating in OT focused on principles of body awareness, the client had regained his independence in ADLs, and was no longer experiencing falls.
Keywords: Occupational Therapy, Neuro-Degenerative Disorders, Fall Prevention
Introduction
Occupational therapy interventions at their core revolve around Activities of Daily Living (ADLs) such as feeding, bathing, grooming, toileting, dressing, and transfers [1]. The performance of any of these ADLs relies on a host of underlying abilities such as proprioception, balance, strength and endurance. The transition from outpatient clinic rehabilitation to home therapy during the COVID-19 pandemic resulted in the opportunity to observe clients in their natural environments where many ambulate barefoot. While providing therapy in the home, one OTP began noticing that some of her clients were displaying a “toe flaring” behavior during ADLs that required sitting or standing balance (C. Rimes, personal communication May 10, 2023) (Fig. 1).
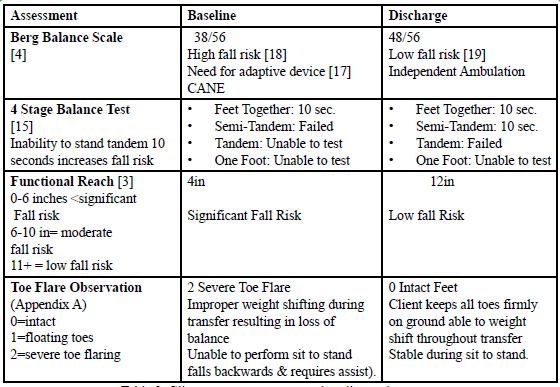
A review of the literature could find no mention of toe flaring, hallux dorsiflexion, and/or its influence on transfers and balance. Balance assessments such as Timed up and Go (TUG) [2], the Functional Reach [3], and the Berg Balance Scale (BBS) [4] do not address either toe function or position during the assessment process. Additionally, the literature on dynamic instability seems to focus on the use of compensatory versus remediation strategies to improve stability during mobility [5].
Clients diagnosed with neurodegenerative diseases often experience challenges attempting to maintain balance during functional transfers when rising from a seated position [6]. Practice guidelines in rehabilitation focus on strengthening and endurance training, adaptive strategy training, and the use of adaptive equipment [6,7]. There is limited attention on the role of body awareness or the role of balance and lower body position [8]. This offers us an opportunity to present a new approach.
There is a need to examine the role of the foot in our evaluation of body awareness. The foot is the only part of the body that stays in contact with the ground during all phases of gait. The toes provide posture and balance, support body weight, and aid in propulsion during the gait cycle [9]. Toes provide stability and momentum for movement and hug the ground so that one may maintain balance when they are doing anything on their feet. The toes are the most flexible part of the foot and are important for stability while standing and moving and the toe flexion angles and force of pushing against the floor affect dynamic balance [10]. While standing, the toes are in contact with the ground, the center of gravity shifts anteriorly, and the balance-controllable range increases. Consequently, the physical stability of the body is achieved. While ambulating, the toes stabilize the body during the entire stance phase and transmit the force during the terminal stance phase, thereby enabling propulsion [11]. Toe dysfunction is believed to cause instability in the physical balance of the body. Little mention of toe flaring has been observed in the literature beyond evidence that persons who fall have lower muscle strength than non-fallers [12]. Toe flaring forces one’s weight back onto their heels and prompts backward leaning [11].
When clients experience multiple falls backwards, they begin to adopt a compensatory posture, leaning forward (to avoid falling backwards) resulting in a kyphotic forward hunched position. Toe flaring may also then reduce the efficiency in shifting body weight and increase the risk of falls. Relying on occupational therapy clinical guidelines for working with clients diagnosed with neurodegenerative diseases, a protocol was developed to incorporate the use of exercise and physical activity focused on principles of body awareness (weight shifting; sensory awareness; postural stability, motor performance, and proper body mechanics) to maximize performance and safety in the performance of ADLs [13].
Design and Setting
This single subject case report (IRB 2023-30) is based on a 59-year old retired Caucasian male Army Master Sergeant who enjoyed socializing with local friends in a variety of environments. He was referred to OT services to regain the ability to perform ADL’s and IADL’s safely and efficiently. The client had recently been diagnosed with amyotrophic lateral sclerosis (ALS). He was experiencing falls and reported feeling unsteady when walking. An occupational therapy practitioner (OTP) completed a comprehensive evaluation of the client in his home.
Methods
The client’s initial evaluation consisted of an interview and observation of functional task performance in the home. The OTP immediately noticed the client’s poor posture as he entered the room. The client had difficulty performing sit-to-stand transfers and was observed to have an exaggerated hallux dorsiflexion (toe flaring) when attempting to rise from a seated position. When his foot position was brought to his attention, he remarked that it was the first time he had noticed it. He experienced significant difficulty properly weight shifting during sitting and standing positions and was unable to bend down to retrieve items from the ground. Reaching out or down resulted in immediate stiffening, muscle tightening, and locking of joints. The client reported he had enjoyed good health throughout his life and the recent ALS diagnosis was the first time he had experienced a significant medical issue. The client was highly motivated to walk his daughter down the aisle for her wedding without a cane [14]. He was using a cane for support during ambulation, and his primary long-term goal centered on maintaining control of his body to live as productively a life for as long as possible. He was in the process of having a single-story home built to better match his current functional abilities, as he realized he was no longer capable of keeping up with the maintenance of his home. The client expressed frustration during the initial OT evaluation because he said that despite spending the last six months engaging in a rigorous exercise regimen to improve his strength and endurance, he was actually losing ground, as his balance was deteriorating and even basic self-care was becoming challenging. He no longer trusted his body and felt he no longer had the ability to complete simple tasks such as collecting the mail or the trash bins and felt himself increasingly “pulling back”, avoiding community activities and crowded venues. He felt defeated.
Administered assessments included:
• Berg Balance Scale [4] designed to measure a client’s risk for falls,
• 4 Stage Balance Test [15] designed to assess body mechanics during dynamic balance activities.
• Functional Reach Test [3] intended to assess forward reach without loss of balance.
Intervention
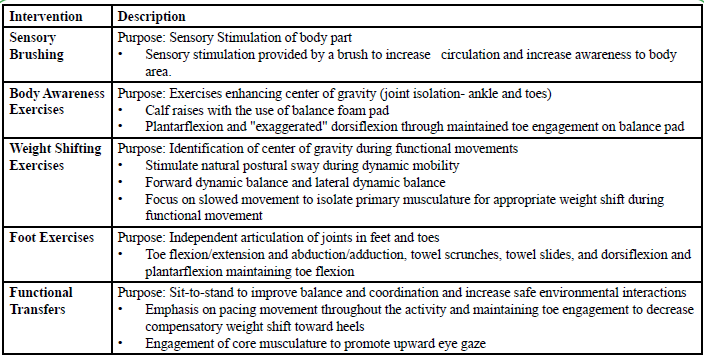
The client was seen in his home for nine (9) one-hour skilled OT sessions over the course of six (6) weeks (Table 1). Each OT skilled therapy session began with the OTP performing a sensory brushing protocol (Appendix B) to provide proprioceptive input to peripheral nerves, promote circulation and increase awareness of the body area. The sensory stimulus via the brush was intended to heighten body awareness [16] to aid the client in maintaining postural awareness designed to maximize safety for the remainder of the OT session. The OTP reviewed the brushing technique and reinforced the need and benefit of completing the brushing protocol 3x a day, as part of the client’s Home Exercise Program (HEP). The brushing protocol consisted of brushing each limb for two (2) minutes for a total of eight (8) minutes. An abnormal toe positioning was noted at the initial evaluation and the OTP included an additional intervention to address the abnormal toe position, described as “toe flaring” during interventions. The client performed a series of body awareness exercises, weight shifting exercises, foot exercises and functional transfers described in (Table 2). As the client’s skills improved (mastering the ability to maintain proper body positioning), greater emphasis was placed on proper body mechanics and exercises to activate the toes and to improve ankle, foot and toe mobility improving isolated joint and muscle mobility improving isolated joint and muscle movement. Natural weight shifting activities were introduced through the feet to facilitate awareness of correct positioning during transfers and proper weight bearing during both transfers and functional movement. As the client’s safety in dynamic standing and weight shifting improved, the focus of the sessions shifted to address the client’s performance of functional ADLs. The OTP developed a screen to measure the client’s ability to maintain toes in contact with the ground during sit-to-stand transfers and was reported as observations of toe positioning/flaring. (Appendix A).
Data Analysis
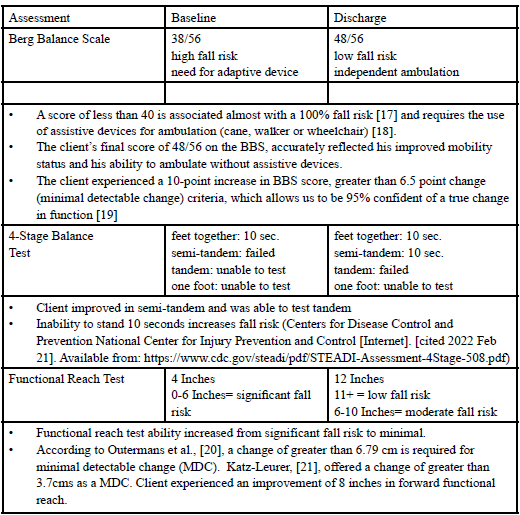
The client was discharged from therapy at six (6) weeks for a cross-country trip. At the time of discharge, the client stated he was satisfied with his abilities for performing tasks and happy he was once again independent in all self-care tasks. The client was ambulating independently and no longer depending on a cane for safety during mobility. He reported a renewed sense of optimism, stating: “for the first time I have hope and a greater sense of control over my body. I’ve been able to return to enjoying activities with my family and friends (male client, 59 years of age).” The OTP documented that the client appeared to have a better sense of his body and demonstrated the ability to shift his body position to maintain balance during tasks. He displayed a more fluid and natural posture, and natural rhythm during functional tasks. He no longer appeared to be hesitating during movement and showed no signs of muscle guarding. In as much as observation of body awareness skills can be reported the client seemed to have a greater sense of his position in space.
The client was referred to the OTP a second time, eight months after the original discharge. The new referral was for a recent onset of loss of function in the left hand. The client now presented with left hand muscle wasting and atrophy and decreased strength and function. The client explained he continued his home exercise plan and was very pleased with his ability to maintain his balance and weight shifting with no observed signs of toe flaring (Scored a 0 on Toe Flare observation during both sit to stand transfers and standing shoulder flexion).
Discussion
This case report demonstrates the importance of completing holistic evaluations that include areas such as foot positioning. It highlights the need to implement interventions that address specific client deficits by designing interventions that challenge and address body awareness, in addition to the performance of ADL tasks. Relying on rote repetition of ADL tasks without addressing body awareness is insufficient to regain balance. The toe flaring phenomenon seen in this case remains a mystery. Researchers have explored the converse motion of “toe curling” [22,23]. Toe curling has been attributed to a basal ganglia dysfunction, the area of the brain responsible for initiating muscle contractions that leads to dystonia (twisting and curling of muscles) and calf spasms. These result in clenched toe curling or reflexive toe-clenching which can worsen when attempting to ambulate, following ambulation (from fatigued muscles) or even re-occurring at certain times of the day as a result of the “wearing off” effect of medications [23]. Similarly, for toe curling and flaring, trajectories and spatiotemporal gait adaptations for approaching uneven terrain and stepping over objects have been offered as explanations for increased falls [24].
Another plausible explanation for toe flaring could be a return to the plantar Babinski reflex, which would occur following a significant neurological insult such as a spinal cord injury or stroke resulting in dorsiflexion of the big toe and fanning of other toes. This would suggest impairment in the corticospinal tract (CST), and a pyramidal tract dysfunction of the CST [25]. A second explanation could be a rapid-onset dystonia-parkinsonism with babinski and pyramidal tract dysfunction, however, since we are able to correct the toe flare pattern when the client is made aware of the posture and instructed in exercises and positioning, a more likely explanation could simply be a maladaptive postural response [26]. Barring alternative explanations such as maladaptive postures resulting from increased pain or abnormal reflexes, a more likely hypothesis for toe flaring is that it is a learned adaptive behavior. For example, when clients with Parkinson’s begin to experience a reduction in functional ability they initially rock backwards and lift their toes in an attempt at recruiting force through their heels [27]. This action allows them to gain momentum and mechanical advantage to increase torque on their heels, which assists in contracting the calf muscles to aid in rising from a sitting position.
Over time, a gradual loss of body awareness resulting from progressive neurodegenerative changes may then lead to toe flaring without the associated momentum to regain balance. The toe flaring then occurs without conscious awareness of the compensatory movement. As clients become weaker they increasingly adopt a forward leaning body position (kyphosis) for fear of falling backwards which leads to the locking of muscles in an attempt to gain stability. This maladaptive response may be what our client identified as feeling “a loss of control of his body” as the maladaptive response no longer results in a successful transfer. An argument could be made that cognitive/attentional mechanisms might explain the return of a normal foot position restoring better balance.
Conclusion
Addressing body awareness and proprioception in the evaluation process is critical to providing effective evidence-based interventions. OTPs have the clinical skills and expertise to develop and implement holistic treatment plans that can provide optimal rehabilitation for clients experiencing body awareness difficulties that are affecting their ability to maintain their independence in ADLs and free of the fear of falls. By focusing on body position, musculature, and posture, we can improve clients’ body awareness and reduce fall risk. It is imperative that OTPs embrace a holistic approach in the evaluation process and implement relevant and meaningful interventions to meet the individual needs of clients.
Implications for Future Research
This case represents the experience of one adult with a chronic neurological condition at risk for falls. It cannot be generalized. No sensory assessments were performed at baseline or discharge limiting our ability to state with any certainty if sensation played a role in the restoration of balance. The improvement in foot positioning that improved balance was due to a cognitive/attentional mechanism rather than the sensory brushing and targeted interventions. Finally, the creation and implementation of researcher designed assessments and interventions will require third party validation before it can be replicated.
Key Messages
• Foot positioning is rarely addressed during assessments and there are no standardized assessments available.
• Preliminary findings of a comprehensive approach to assessing and addressing body awareness issues are positive and should be explored.
Acknowledgments
Our many thanks to the client in this case report for his willingness to participate and share results to help improve the lives of others.
Abbreviations
TUG: Timed Up and GO
ADL: Activities of Daily Living
CST: Corticospinal Tract
PD: Parkinson’s Disease
ALS: Amyotrophic Lateral Sclerosis
LB: Lower Body
UB: Upper Body
Bilateral hallux dorsiflexion
Toe flaring
OT: Occupational Therapy
Competing Interests:
The author declares that he has no competing interests.
References
Occupational therapy practice framework: Domain and process—Fourth edition. (2020). The American Journal of Occupational Therapy, 74(Supplement_2). View
Podsiadlo, D., & Richardson, S. (1991). The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. Journal of the American Geriatrics Society, 39(2), 142–148. View
Duncan, P. W., Weiner, D. K., Chandler, J., & Studenski, S. (1990). Functional reach: a new clinical measure of balance. Journal of Gerontology, 45(6), M192–M197. View
Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I., & Maki, B. (1992). Measuring balance in the elderly: validation of an instrument. PubMed, 83 Suppl 2, S7-11. View
Otake, Y., Yozu, A., Fukui, T., Sumitani, M., & Haga, N. (2018). Relationship between Toe Flexion Movement and Center of Pressure Position. International Journal of Foot and Ankle, 2(2). View
Schoneburg, B., Mancini, M., Horak, F., & Nutt, J. G. (2013). Framework for understanding balance dysfunction in Parkinson’s disease. Movement Disorders, 28(11), 1474–1482. View
Monticone, M., Ambrosini, E., Laurini, A., Rocca, B., & Foti, C. (2015). In-patient multidisciplinary rehabilitation for Parkinson’s disease: A randomized controlled trial. Movement Disorders, 30(8), 1050–1058.View
Hewitt, J., Goodall, S., Clemson, L., Henwood, T., & Refshauge, K. (2018). Progressive Resistance and Balance Training for Falls Prevention in Long-Term Residential Aged Care: a cluster randomized trial of the Sunbeam program. Journal of the American Medical Directors Association, 19(4), 361–369. View
Wood, J., Henderson, W., & Foster, E. R. (2022). Occupational therapy practice guidelines for people with Parkinson’s Disease. American Journal of Occupational Therapy, 76(3). View
Rodgers, M. M. (1995). Dynamic Foot Biomechanics. Journal of Orthopaedic and Sports Physical Therapy, 21(6), 306–316. View
Hughes, J., Clark, P., & Klenerman, L. (1990). The importance of the toes in walking. Journal of Bone and Joint Surgery - British Volume, 72-B(2), 245–251. View
Mickle, K. J., Munro, B. J., Lord, S. R., Menz, H. B., & Steele, J. R. (2009). ISB Clinical Biomechanics Award 2009. Clinical Biomechanics, 24(10), 787–791. View
Acharya, A. B., Jamil, R. T., & Dewey, J. J. (2023, January 1). Babinski reflex. StatPearls - NCBI Bookshelf. View
Chapman, M. (2022, November 14). Als success story delivers man’s “most special day.” ALS News Today. View
Centers for Disease Control and Prevention & National Center for Injury Prevention and Control. (2017). The 4-stage balance test. View
Keppler, S., Döllinger, N., Wienrich, C., Latoschik, M. E., & Israel, J. H. (2022). Self-touch: an immersive interaction technique to enhance body awareness. I-com, 21(3), 329–337. View
Shumway-Cook, A., Baldwin, M., Polissar, N. L., & Gruber, W. (1997). Predicting the probability for falls in Community Dwelling older adults. Physical Therapy, 77(8), 812–819. View
Qutubuddin, A. A., Pegg, P. O., Cifu, D. X., Brown, R., McNamee, S., & Carne, W. (2005). Validating the Berg Balance Scale for patients with Parkinson’s disease: A key to rehabilitation evaluation. Archives of Physical Medicine and Rehabilitation, 86(4), 789–792. View
Romero S, Bishop MD, Velozo CA, & Light K. (2011). Minimum detectable change of the Berg Balance Scale and Dynamic Gait Index in older persons at risk for falling. Journal of Geriatric Physical Therapy, 34(3):131-7. View
Outermans, J. C., van Peppen, R. P., Wittink, H., Takken, T., & Kwakkel, G. (2010). Effects of a high-intensity task-oriented training on gait performance early after stroke: a pilot study. Clinical Rehabilitation, 24(11), 979–987. View
Katz-Leurer, M., Fisher, I., Neeb, M., Schwartz, I., & Carmeli, E. (2009). Reliability and validity of the modified functional reach test at the sub-acute stage post-stroke. Disability and Rehabilitation, 31(3), 243–248. View
Chahine, L. M., Edison, B., Daeschler, M., Mantri, S., Kahl, S., Rapoport, R., Goyle, A., Precht, C., Kopil, C., & Marras, C. (2020). The most bothersome aspects of off periods reported by individuals with Parkinson’s disease. Movement Disorders Clinical Practice, 7(3), 284–292. View
Galna, B., Murphy, A. T., & Morris, M. E. (2009). Obstacle crossing in people with Parkinson’s disease: Foot clearance and spatiotemporal deficits. Human Movement Science, 29(5), 843– 852. View
Hirayama, K., Fukutake, T., & Kawamura, M. (1999). ‘Thumb localizing test’ for detecting a lesion in the posterior column– medial lemniscal system. Journal of the Neurological Sciences, 167(1), 45–49. View
Liu, Y., Lu, Y., Zhang, X., Xie, S., Wang, T., Wu, T., & Wang, C. (2016). A case of rapid-onset dystonia-parkinsonism accompanied by pyramidal tract impairment. BMC Neurology, 16(1). View
Endo, M., Ashton-Miller, J. A., & Alexander, N. B. (2002). Effects of age and gender on toe flexor muscle strength. The Journals of Gerontology Series A, 57(6), M392–M397. View
Robb, K. A., & Perry, S. D. (2019). Textured foot orthotics on dynamic stability and turning performance in Parkinson’s disease. Journal of Motor Behavior, 52(4), 396–403. View