Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-170
https://doi.org/10.33790/jrpr1100170Research Article
A Cross-Sectional Pilot Study on the Impact of Socioeconomic Status on Fall Risk in Older Adults Based on Multiple Outcome Measures: 10MWT, 5TSIS, CTSIB-M, and 6MWT
Mary Bayer DPT1, Halle Krisinski DPT1, Nikita Sak DPT1, and Rob Sillevis DPT, PhD1*
1Department of Rehabilitation Sciences, Florida Gulf Coast University, Fort Myers, FL, 33965,United States.
Corresponding Author Details: Rob Sillevis DPT, PhD, Associate Professor, Department of Rehabilitation Sciences, Florida Gulf Coast University, Fort Myers, FL, 33965, United States.
Received date: 05th May, 2025
Accepted date: 04th June, 2025
Published date: 06th June, 2025
Citation: Bayer, M., Krisinski, H., Sak, N., & Sillevis, R., (2025). A Cross-Sectional Pilot study on the Impact of Socioeconomic Status on Fall Risk in Older Adults Based on Multiple Outcome Measures: 10MWT, 5TSIS, CTSIB-M, and 6MWT. J Rehab Pract Res, 6(1):170.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The prevalence of falls increases with age, with one in four older adults reporting at least one fall per year. Falls can be fatal or non-fatal and lead to a variety of physical and psychological complications. The occurrence of falls can be affected by factors including but not limited to comorbidities, environment, medication, dizziness, and postural hypotension. As the population continues to age, it is important to gain a better understanding of factors contributing to falls so that appropriate preventative interventions can be provided. Socioeconomic status is a potential risk factor that has limited evidence.
Purpose: This study aims to determine if there is a relationship between four fall assessment scores in geriatric community dwelling populations of higher and lower socioeconomic status. The assessments for fall risk will be the 10-meter Walk Test (10MWT), Five Times Sit-to-Stand (5TSTS), Modified Clinical Test of Sensory Interaction on Balance (CTSIB-M), and a 6 Minute Walk Test (6MWT).
Methods: Subjects will be recruited from community-dwelling housing at Bonita Springs Senior Center after agreeing to and consenting to participate. They will complete the 10-meter Walk Test (10MWT), Five Times Sit-to-Stand (5TSTS), Modified Clinical Test of Sensory Interaction on Balance (CTSIB-M), and a 6 Minute Walk Test (6MWT) along with a socioeconomic status survey. Subjects will be anonymous, and their scores and surveys will be attached to a number to maintain anonymity.
Results: The sample consisted of 18 participants (n=18) with 13 females and 5 males aged 70-91 years with an average age of 82. One participant was excluded from the study after disclosing a history of Parkinson’s during data collection bringing the sample size to n=17 with 13 females and 4 males. Fall risk of 5TSTS and fall risk of CTSIB-M had a statistically significant (p = 0.035) and strong positive correlation (r = 0.514). Fall risk of 6MWT and fall risk of 10MWT had a statistically significant (p = 0.044) and moderate positive correlation (r = 0.494). All other results compared had no statistical significance.
Conclusion: Fall risk associated with scores of the 6MWT and 10MWT were found to be significantly correlated, indicating a positive relationship regarding walking speed and walking endurance in this patient population. Fall risk associated with scores of the 5TSTS and CTSIB-M were found to be significantly correlated, indicating a positive relationship regarding quadriceps strength and functional balance in this population. No significant correlations were found regarding education, age, current income and the outcome measures tested in the study.
Key Words: Fall Risk, Geriatric Population, Socioeconomic Status 10MWT, 6MWT, 5TSTS, CTSIB-M
Introduction
In general, falls play a large role in hospitalization and early decline of health status in older populations, with falls leading to over 250,000 injuries and 11,000 deaths each year [1]. While socioeconomic status (SES) and fall risk have been studied to some extent, the assessment of fall risk using various outcome measures and surveys to screen for general health factors with fall risk has not been studied thouroughly [2]. The only research found in this area included a few systematic reviews with many limitations due to lack of research in the area [2]. Falls are known to have a high associated economic burden, therefore it is important to continue to investigate the potential factors leading to falls [3-4]. As the cost of healthcare services continues to increase, the importance of health promotion and fall prevention for the older adults needs to be stressed. In order to prevent falls, providers must be knowledgeable in the many factors that can lead to falls. These may include but are not limited to disease or illness, decreased aerobic capacity, decreased functional lower extremity strength, poor balance, decreased gait speed, poor nutrition, poor overall health status, vision or hearing deficits, and potentially economic and environmental factors [5].
In this study, the specific standardized outcome measures were used to assess fall risk. These measures assessed different variables such as balance, gait speed, functional lower extremity (LE) strength, and muscle/aerobic endurance to determine fall risk. The tests chosen were the 10-meter Walk Test (10MWT) to assess gait speed [6], Five Times Sit-to-Stand (5TSTS) to assess functional lower extremity strength [7], Modified Clinical Test of Sensory Interaction on Balance (CTSIB-M) to assess balance systems [8], and the Six Minute Walk Test (6MWT) to assess aerobic capacity [9-11]. A survey was created for this study to help determine socioeconomic status (SES) in which questions were asked about annual household income, highest education level achieved, childhood household income, and retirement status. The aim was to obtain a brief yet comprehensive look into the SES of the participants. Through this research, the researchers hope to shed some light onto possible correlations between SES and fall risk in order to better allow for comprehensive fall risk assessment and fall prevention of all aging individuals.
Background
As the population continues to age, geriatric care is taking on a larger role in physical therapy, especially in the areas of fall prevention and post-fall complication rehabilitation [12]. The World Health Organization (WHO) defines falls as “inadvertently coming to rest on the ground, floor, or other lower level, excluding intentional change in position to rest in furniture, wall, or other objects [13].” While the prevalence of falls increases with age, it is estimated that one in four older adults will fall per year [14]. The occurrence of falls can be affected by factors including but not limited to comorbidities, environment, medication, dizziness, and postural hypotension [15]. Falls can be fatal or non-fatal and lead to a variety of physical and psychological complications [14]. As the population continues to age, it is important to gain a better understanding of factors contributing to falls so that appropriate preventative interventions can be provided. One factor with mixed research pertaining to falls is socioeconomic status (SES), with only 3 prospective studies conducted that considered SES indicators other than educational level as of 2021 [16]. Of these studies, SES is not assessed on a multifactorial association using age, gender, income, childhood income, and education [16]. Lower SES can limit access to medical care, such as physical therapy, screening of fall risk, obtaining a diagnosis of conditions that increases fall risk, and preventative care. Understanding the impact of SES on fall risk can help clinicians understand which populations/types of patients are most in need of fall-related interventions such as: providing patient education, referring to other providers, distribution of information and resources, and modification of plans of care to appropriately address any differences [2].
SES & Fall Risk
Socioeconomic status is generally determined by education level, occupation, income, and wealth [17]. Several studies have found that higher SES leads to overall better well-being, as there is increased access to adequate nutrition, healthcare, and wellness services [18-20]. It has been suggested that lower SES leads to increased fall risk among older adults, as there are greater health inequalities in low-income individuals [18-20]. Individuals with higher SES likely have greater access to specialty care for vision and hearing among other services, which may contribute to a decreased fall risk. Sight and hearing both have effects on balance, and if these systems are not properly functioning, may lead to increased fall risk [5]. Other factors that may negatively impact the overall health of individuals of lower SES are unexpected fluctuations in life stressors. These may include illness, chronic stress, abuse or violence, and uncertainty of income. Individuals of higher SES are less likely to experience these events, leading to decreased stress [5]. Increased stress may lead to the development of unhealthy habits, such as smoking or drinking, as a coping mechanism.
Lastly, nutrition is another important health factor associated with SES and general health [17]. Food insecurity is the concept of altered eating patterns or nutrient intake as a result of limited financial resources [17]. It is a well-studied fact that healthier diets tend to be more costly than unhealthy diets. While this tends to be true in most cases, a systematic review by Darmon and Drewnowski [21] demonstrated what this means for overall health and socioeconomic status. They found that energy-dense foods are cheaper per calorie, and these are typically found more in the diets of those in the lower SES group [21]. Energy-dense foods are composed of refined grains, added sugars, or fats, in contrast to the more costly food items that are nutrient-dense foods, such as fruits and vegetables [21]. Since those in lower SES households are eating more refined grains, added sugars, and fats in their diet, it is possible that they may not be receiving adequate amounts of valuable nutrients found in vegetables and fruits that are important to their body and overall health [21] an important role in decreased overall health status and increased fall risk in those who are in lower SES households.
Assessing Fall Risk
Fall risk is assessed utilizing outcome measures such as the 10MWT, 5TSTS, 6MWT, and CTSIB-M. The literature shows that these tests can assess fall risk by measuring different aspects of a person's physical health. 6MWT is a validated measure of submaximal aerobic capacity and functional endurance with strong test-retest reliability (ICC > 0.90). During the test, participants are instructed to walk as far as possible within six minutes along a flat, straight 30-meter walkway [9-11]. A 2020 study by Paccini-Lutosa and colleagues has shown a moderate correlation between fall risk and aerobic capacity in community-dwelling elderly [9]. Research indicates that ambulating distances of less than 331.65 meters are related to a greater risk of falling [10]. Normal values for males in their 60s, 70s, and 80s are 572 meters, 527 meters, and 417 meters, respectively [11]. For women in their 60s, 70s, and 80s, it is 538 meters, 471 meters, and 392 meters, respectively [11]. Harada and colleagues found this test to have adequate concurrent validity with chair stands, standing balance, and gait speed for predicting falls in older adults [22]. The test-retest validity has a 95% confidence interval [22].
5TSTS assesses functional lower limb muscle strength and power through a timed test of repeated sit to stand transfers without the use of the upper extremities; scores of 16 seconds or greater indicate the risk of falls [7]. Lower limb strength deficits have been shown to have a strong correlation with an increase in fall risks [23]. This test has been found by Bohannon and others to have an intraclass correlation coefficient of 0.957, suggesting its reliability [24]. The 5TSTS has also been suggested in the literature to be a valid measure of the physical functioning in older adults [7,22,24].
The CTSIB-M examines balance in four conditions testing to determine which balance systems are impaired [8]. The four stages are: eyes open firm surface, eyes closed firm surface, eyes open foam surface, eyes closed foam surface [8]. The foam surface eliminates the somatosensory system by eliminating proprioceptive feedback from the feet and ankles [8]. When the eyes are closed, the visual system is eliminated [8]. The first stage tests the baseline condition, which includes all three systems. In the second stage, tests are performed to determine if the patient has any deficits in the somatosensory system or vestibular system. In the third and fourth stages, a foam pad is used to diminish somatosensory input. During the third stage, the eyes are open to test if their visual system can compensate for varied somatosensory input. In the fourth stage, the patient must rely on their vestibular system to maintain balance. A loss of function of any of these systems has been found to have a relationship to an increased risk of falls [8]. This test has been shown to have moderate validity and reliability when compared with the Greek Mini-Best Test [8]. This test has also been shown to be a predictor of multiple future falls when the individual cannot maintain standing on the foam surface with the eyes closed [25].
The 10MWT is used to assess gait speed. A decreased gait speed can indicate an increased risk of falls, hospitalization, and need for a caregiver [26]. Normal values for men in their 60s, 70s, 80s and above are 1.339 meters per second (m/s), 1.262 m/s, and 0.968 m/s respectively [27]. For women, normal values are 1.241 m/s, 1.132 m/s, and 0.943 m/s for the same age groups [27]. A score lower than 0.7m /s indicated a risk of adverse events, such as falls [27]. The 10MWT has been found to have excellent test-retest reliability for healthy older adult populations [28].
Economic Impact of Falls
As falls often lead to secondary complications, such as fractures, dislocations, and hospitalization, it is important to consider the financial impact of falls [29] It is estimated that falls cause 10-15% of emergency department visits annually [13]. With the median cost of hospitalization after a fall estimated to be between $11,000 to $26,143 per year, one fall can be economically devastating for individuals living with a lower SES [30,31]. This cost does not include extended care facilities or outpatient rehabilitation that may be needed as follow up care. Despite the majority of the cost of post fall hospitalization and care being covered by Medicare and Medicaid, there is still a high out-of-pocket cost for individuals [14]. The CDC estimates annually, twelve billion dollars are paid by private payers or out of pocket for non-fatal falls [32]. For individuals of lower SES, this out-of-pocket cost can be detrimental and lead them further into poverty or cause them to rely on other family members for financial support [33]. In recent polling from Peterson-KFF, 41% of American adults have healthcare debt that has led them to decrease spending on food and household items, borrow from their savings, or lend from friends or family [34]. This can place strain on relationships, lead to food insecurity, and potentially contribute to an overall decrease in quality of life and independence. Better understanding the potential factors leading to costly falls can likely help to reduce the over $220 billion of medical debt in the United States [34].
Methods
Research Design
This cross-sectional study design utilized a mixed methods approach that used the 10MWT, 6MWT, 5TSTS, and CTSIB-M as outcome measures to assess fall risk in older adults. Participants were given a written survey that was designed for this study to assess SES by collecting self-reported participant information on childhood household income, current income, education level, retirement status, and occupation. The research question was: Is there a relationship between fall risk and the geriatric community-dwelling population of varying socioeconomic status based on these outcome measures collected? Determining this relationship helps providers better understand fall risk in those with varying SES and educate or provide individually curated preventative measures to improve quality of life and reduce future falls in those with varying SES.
Sampling
Since this was a pilot study, no power analysis was used to determine the number of participants for this study. Eighteen participants were recruited from Bonita Springs Senior Center in Bonita Springs, Florida in the time frame of data collection. Participants were recruited from Bonita Springs Senior Center in Bonita Springs, Florida. This location was selected to capture individuals of varying economic status according to income maps of the areas of Lee and Collier counties [35]. Participants were chosen using a convenience sampling method comprised of volunteers within the community center. Criteria for inclusion was participants who were community-dwelling greater than 65 years of age in self reported good health. Community dwelling for the purpose of this study included those living in the general community, independent living communities, or senior living communities. Exclusion criteria will be adults with moderate cognitive impairment such as Alzheimer’s or dementia, age less than 65, dwell in assisted living, or are unable to independently ambulate the community. Participants were excluded if they self-reported a medical history of mild cognitive impairment, dementia, and Alzheimer’s disease, as well as other diagnoses such as Parkinson’s Disease or history of stroke which may impact the individual’s performance on these tests. Individuals younger than 65 were not included. Individuals who are unable to ambulate the community independently or reside in assisted living facilities were also excluded. One participant was excluded from this study due to history of Parkinson’s Disease reported during testing.
Procedure
Approval for this study was given by the Florida Gulf Coast University Institutional Review Board on June 13, 2024 through an expedited review. Informed consent was collected prior to participation in this study. After obtaining written consent, the participants were given a random number for data collection to maintain anonymity. Participants were given a paper survey on socioeconomic status to complete. The survey (see appendix 1) consisted of questions about current annual household income, highest educational level completed, occupation, retirement status, and childhood household income. Income was measured in increments of $25,000, from less than $25,000 to greater than $150,000.
Once the survey was completed, participants were taken through each test. Results of each test were recorded on a scorecard sheet (see appendix 2). This scorecard included space for the participant’s score to be recorded, the normative scores for the age group for each test, and whether the score indicates a heightened risk of falling [6-11,23,27]. After completing all tests, scores were discussed with the participants.
During the screening process, each outcome measure had a designated station. The tests were completed in random order to minimize testing effect. The 10-Meter Walk Test (10MWT) is a reliable and valid assessment of gait speed and functional mobility [27]. The subjects were instructed to walk a total of 10 meters at their comfortable or fastest safe pace. The test was repeated 3 times and the average speed (in meters per second) was calculated. The 6MWT course was a 27.5-meter (90 feet) loop around the senior center multipurpose room, designated by cones and chairs marking the course. One six-minute trial was given, and the participant was notified of the time passed and left in the test at each minute. The participant was allowed take as many standing rests as they liked, however the timer was not stopped [36]. If the participant needed to take a seated rest break, the timer would be stopped and the test would be considered complete at that time [36]. Participants were permitted to use any assistive device or bracing they were currently using. The type of device and/or bracing was documented. During the test, the administrator walked closely behind the participant for safety and to decrease the influence on speed and distance walked [36]. After six minutes, the participant was instructed to stop, and the distance completed was measured and recorded [36]. For the purposes of this study, the 10WT was modified slightly to be done during the 6MWT. The floor was marked with tape and cones at a distance of five meters due to the space constraints of the testing room. The time was recorded to the nearest hundredth of a second when the participant passed the cones. This was recorded around minute one and minute two of the 6MWT. This gave an estimated average gait speed.
For the CTSIB-M, participants were instructed through four stages. The first stage was standing on a firm surface (the hard floor) with feet positioned at hip distance apart and with eyes open for 30 seconds. In the second stage, they maintained the same positioning with their eyes closed for 30 seconds. In the third and fourth stages, participants stood on a foam surface (two-inch thick AirEx pad) with their eyes open and then closed, respectively. In between each stage, they were permitted a 10-second rest. Participants were allowed two additional attempts if they were unable to maintain the position for 30 seconds. The scores of these three trials were then averaged [8]. The CTSIB-M has demonstrated moderate to excellent test-retest reliability (ICC ranging from 0.75 to 0.95) and is validated against force platform measures of balance [8]. The CTSIB-M is a practical, reliable, and efficient tool for assessing functional balance in older adults. This test has also been shown to be a predictor of multiple future falls when the individual cannot maintain standing on the foam surface with the eyes closed [25].
The 5TSTS assessed the lower limb strength as well as balance and postural control [23]. For this test, participants were seated in a chair forty-eight centimeters high with their arms across their chest to prevent assistance from their upper extremities [9]. Participants were instructed to rise to a full standing position and return to a seated position five times as quickly as possible without using their arms, unless required for safety. Timing begins on the command “Go” and ends when the participant fully stands for the fifth time. The total time taken, was recorded in seconds. They were given one attempt to complete the test. If the participant was unable to complete the test without the use of the upper extremities, they were allowed to complete the test however were considered to be at risk of falls [9]. In community-dwelling older adults, a cut-off time of > 16 seconds is often used to indicate increased risk of falls [7].
Data Analysis
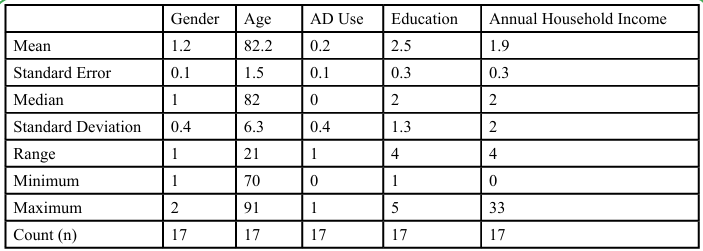
IBM® SPSS® version 28.0 was utilized to analyze the data. Descriptive statistics were used to describe the age, gender, assistive device (AD) use, education, and annual household income of the sample. The Shapiro–Wilk test of normality identified that the data were normally distributed for all variables with p > 0.05; for that reason, the Pearson’s correlation was used to evaluate the correlation between age, education, and fall risk as indicated by performance on the 6MWT, 10MWT, 5TSTS, and CTSIB-M.
Results
The sample consisted of 18 participants (n=18) with 13 females and five males aged 70-91 years with an average age of 82. One participant was excluded from the study after disclosing a history of Parkinson’s during data collection. The final sample size was n=17 with 13 females and four males. The education received ranged between high school, some college experience and an associate's degree. This includes three participants with some college experience, five participants with a high school Diploma or GED equivalent, five participants with an associate’s degree, three participants with a bachelor's degree, and one participant with a master's degree. Although the survey included a question on annual household income, the data were limited in quality and completeness. Several participants reported uncertainty about their household income and provided only estimated guesses. Among the 15 participants who were able to answer the current annual household income question, responses varied: seven reported incomes between $25,000–49,999, four between $50,000–74,999, three reported less than $24,000, and one reported $75,000–99,999. Due to the limited sample and reliability concerns, income data were not used in the final analyses. As a result, education level was used as the primary SES indicator in this study. Future research should seek to capture more comprehensive and validated SES data, including income, occupational status, and neighborhood indicators, to more accurately assess the relationship between socioeconomic factors and fall risk.
The Pearson’s correlation was used to evaluate the correlation between variables. The following variables were evaluated; age, education and fall risk level concurrent with performance of the different outcome measures performed. For the interpretation of the Pearson’s r value, the following were used: values between 0.1-0.3 are weakly correlated, between 0.3-0.5 are moderately correlated, and above 0.5 strongly correlated [36]. For this study the set significance level was set at <0.05 [38].
Age and Fall Risk
Correlations between age and fall risk were determined based on Pearson’s correlation and p-value to understand the significance of each outcome measure tested during the study. Age and fall risk associated with the 10MWT had a non-significant (p = 0.197) but moderate negative correlation (r = -0.329). Age and fall risk associated with the 5TSTS had a nonsignificant (p = 0.844) and below weak positive correlation (r = 0.052). Age and fall risk associated with the 6MWT had a non-significant (p = 0.744) and below weak positive correlation (r = 0.075). Age and fall risk associated with the CTSIB-M had a non-significant (p = 0.690) and weak positive correlation (r = 0.105). Lastly age and education had a non-significant (p = 0.577) and weak positive correlation (r = 0.146).
Fall risk of 5TSTS and fall risk of 10MWT had a non-significant (p = 0.146) but moderate positive correlation (r = 0.368). Fall risk of 6MWT and fall risk of 10MWT had a statistically significant (p = 0.044) and moderate positive correlation (r = 0.494). Fall risk of CTSIB-M and fall risk of 10MWT had a non-significant (p = 0.366) and weak positive correlation (r = 0.234). Fall risk of 5TSTS and fall risk of 6MWT had a non-significant (p = 0.233) but moderate positive correlation (r = 0.308). Fall risk of 5TSTS and fall risk of CTSIB-M had a statistically significant (p = 0.035) and strong positive correlation (r = 0.514). Fall risk of 6MWT and fall risk of CTSIB-M had a non-significant (p = 0.398) and weak positive correlation (r = 0.219).
Education and Fall Risk
Correlations between education and fall risk were determined based on Pearson’s correlation and p-value to understand the significance of each outcome measure tested during the study. Education and fall risk associated with the 10MWT had a non-significant (p = 0.656) and weak negative correlation (r = -0.117). Education and fall risk associated with the 5TSTS had a non-significant (p = 0.529) and weak positive correlation (r = 0.164). Education and fall risk associated with the 6MWT had a non-significant (p = 0.551) and weak negative correlation (r = -0.156). Lastly, education and fall risk associated with the CTSIB-M had a non-significant (p = 0.718) and below weak positive correlation (r = 0.095). All these correlations discussed can be found in Table 2.
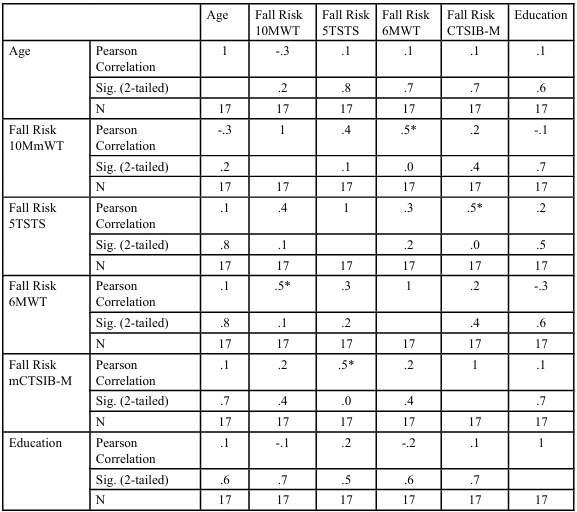
Table 2. Pearson correlation of age, prior level of education received, and outcome measures performed
Discussion
Falls are a major concern for the aging population with multiple factors having an effect on an individual’s risk of falling. There is a current gap in the literature in regard to the role SES plays in fall risk. In the current study, 17 participants were surveyed to determine SES and fall risk. Of the 17 participants included, 11 were found to be at risk of falls on the 10MWT, seven on the 5TSTS, 15 on the 6MWT, and six on the CTSIB-M.
Prior research has suggested that higher SES individuals have a lower instance of falls.5 While this study cannot confirm nor deny the impact of SES on fall risk due to limited variability in SES among participants, correlations found between fall risk as determined by the relationship of 5TSTS and CTSIB-M as well as the relationship of 6MWT and 10MmWT were found to be statistically significant.
The current study found a statistically significant positive correlation between the 10MWT and 6MWT. According to previous literature in this area in 2012, strong correlations were also found between walking speed and walking endurance in the population of stroke and MS patients [39]. In another study assessing the relationship between gait speed and walking endurance in Parkinson's patients, a relationship was found between the two, specifically with comfortable 10MWT speed and 6MWT [40]. While research regarding the relationship between the 10MWT and the 6MWT has begun to be assessed in different populations, this study found a positive correlation in regards to the general community dwelling geriatric population, which to our knowledge has not been studied at this time.
It is interesting to note that as the results indicated a significant correlation between 10MWT and 6MWT, there was no significant correlation between these two outcome measures and 5TSTS which assessed quadriceps strength. When looking into other literature discussing the relationship between quadriceps strength (5TSTS) and gait speed (10MWT), they did find a correlation between those outcome measures in the stroke population. A study in 2021 found a moderately strong negative relationship between 5TSTS and 10MWT [41]. This negative correlation found in the 2021 study suggests that as the participants scored lower times with the 5TSTS, indicating stronger quadriceps, the participants gait speed was higher, indicating faster ambulation [41]. Another study discussing the relationship between walking endurance (6MWT) and quadriceps strength in systolic heart failure patients found a significant correlation. This 2025 study found a moderate inverse relationship between the 5TSTS and 6MWT [42]. This inverse correlation found in the 2025 study suggests that as participants walked longer distances, scoring higher in the 6MWT, the participants completed the 5TSTS at a quicker rate, indicating stronger quadriceps [42].
The current study also found a statistically significant positive correlation between the CTSIB-M and 5TSTS. The relationship between these tests has not been explored in the current literature and would need further investigation to confirm the presence of a statistically significant relationship in a larger sample size. However, several studies have explored the relationship between lower extremity strength and balance in older adults. A 2019 study found a moderate correlation between leg strength and balance performance using a dynamometer to measure leg extension strength and the stork balance stand test to assess balance [43]. Furthermore, a 2024 Taiwanese study found that lower extremity strength had a positive relationship with static and dynamic balance performance [44]. These studies suggest that lower extremity strength can play a role in balance of older adults, which aligns with the findings of the current study.
It has been found that no single test is an adequate predictor of fall risk in geriatric populations [45]. Each of the tests selected for this study assess common factors related to falls including gait speed, endurance, balance and its components, and lower extremity strength and power. When used in combination, the 6MWT, 5TSTS, 10MWT, and CTSIB-M can assist clinicians in identifying a patient’s potential deficits and aid in tailoring interventions to reduce risk of falls [45]. It is important to continue to investigate other factors that may contribute to fall risk, including SES, nutritional status, medications and polypharmacy, and cognitive impairments.
Limitations
There were several limitations to this study. The small sample size was small, leading to a decreased ability to make assumptions and generalizations about the results of the study. The small sample size had several potential reasons. The response of the community was less than expected and led to limited participation in the study. As this study was conducted at only one location, there was a potential limited variance in SES in participants as most individuals lived in relatively the same geographic location. Of the 15 participants who were able to answer the current annual household income question of the survey, there was less variability in reported annual household income than was expected for the given geographic area chosen, as Bonita Springs was expected to have a greater variety based on the data from Best Neighborhood on household income in the area [35]. Finally, many of those who were at the facility were unwilling to participate in the study. Of those who were willing and able to participate, many were unable or unwilling to answer all the questions in the survey. This further limit the generalizability of the results.
Although efforts were made to control for certain demographic characteristics, this study may still be affected by unmeasured confounding variables. Factors such as comorbidities, polypharmacy, variations in physical activity levels, environmental hazards, and psychological status (such as the fear of falling) could have influenced both the outcome measures and fall risk. The absence of control for these potential confounders may have introduced bias into the observed associations. Future studies with multivariate models or longitudinal designs should aim to control for these variables to better isolate the effects of individual functional assessments on fall risk.
In addition to the limitations already noted, this study may be subject to recall bias, particularly in self-reported aspects such as prior falls or medical history, which could influence the associations observed. Selection bias is also a consideration, as participants who volunteered may differ systematically from those who declined participation, potentially affecting generalizability. Furthermore, the cross-sectional design limits our ability to draw causal inferences between the outcome measures and fall risk. Longitudinal studies are needed to establish temporal relationships and predictive validity among these variables.
Since this research was only done in one geographic location in Bonita Springs, this could have caused the range in socioeconomic status to be too narrow to find any statistically significant results. In the future, it may be beneficial to replicate this study with data obtained in a larger geographic location to expand the range of socioeconomic status to obtain more accurate data that can generalize to more of the population. Another suggestion would be to increase the number of participants to improve the generalizability of the data collected and come to more reliable conclusions. Lastly, follow-up research could be done with a more standardized survey questionnaire to assess socioeconomic status. In this research study, we found that many participants were unable to fully answer the survey, especially in regard to childhood income. A different survey with more standardized results regarding socioeconomic status could be useful in future research to identify the full scope and relationship between socioeconomic status and fall risk in the geriatric population.
Conclusion
Fall risk was found to be significantly correlated with walking speed and endurance (6MWT and 10MWT), as well as quadriceps strength and functional balance (5TSTS and CTSIB-M), suggesting that these measures may serve as useful indicators of fall susceptibility in this patient population. While no significant correlations were found between demographic factors such as education and age, or among certain combinations of outcome measures, the study supports the multifactorial nature of fall risk and highlights the value of using a combination of standardized functional assessments in clinical practice. These findings have important clinical implications: integrating tools such as the 6MWT, 10MWT, 5TSTS, and CTSIB-M into routine assessment protocols may enhance clinicians' ability to identify patients at higher risk of falls and guide the development of personalized intervention strategies.
From a policy perspective, the results support continued advocacy for standardized fall risk screening protocols in outpatient and community health settings, especially for aging or neurologically impaired populations. Future research should explore the predictive validity of these tools in longitudinal fall incidence studies, and investigate how interventions targeted at improving specific functional domains—such as balance or lower extremity strength—might mitigate fall risk. Additionally, research examining environmental, psychosocial, and behavioral contributors to fall risk could complement these findings and further inform fall prevention frameworks.
Competing Interest:
The authors of this research declare no competing interest regarding this study.
References
Li, S., Surineni, K. (2024). Falls in hospitalized patients and preventive strategies: A narrative review. The American Journal of Geriatric Psychiatry: Open Science, Education, and Practice. 5:1-9.View
Smit, F., van Zwieten, A., Sherrington, C., et al. (2025). Socioeconomic position across the life course and falls among middle- and older-aged adults: protocol for a systematic review. BMJ Open. 15(1):e087971.View
U.S. Centers for Disease Control and Prevention. (2024). Facts about Falls. Older Adult Fall Prevention. Published May 9, View
Newgard, C. D., Lin, A., Caughey, A. B., et al. (2020). The Cost of a fall among older adults requiring emergency services. J Am Geriatr Soc. 69(2):389-398. View
Liu, H., Hu, T. (2022). Impact of socioeconomic status and health risk on fall inequality among older adults. Health & Social Care in the Community. 30(6):e4961-e4974. View
Kitcharanant, N., Vanitcharoenkul, E. & Unnanuntana, A. (2020). Validity and reliability of the self-rated fall risk questionnaire in older adults with osteoporosis. BMC Musculoskelet Disorders. 21(1). View
Buatois, S., Perret-Guillaume, C., Gueguen, R., et al. (2010). A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys Ther. 90(4):550-560. View
Cohen, H., Blatchly, C. A., Gombash, L. L. (1993). A study of the clinical test of sensory interaction and balance. Physical therapy. 1;73(6):346-51. View
Paccini Lutosa, L., Soares da Silva, J., Gomes Pereira, D. A., et al. (2020). Physiological risk of falls, physical and aerobic capacity in community-dwelling elderly. Fisioter Mov. 33:e003342. View
Regan, E., Middleton, A., Stewart, J. C., et al. (2020). The six minute walk test as a fall risk screening tool in community programs for persons with stroke: a cross-sectional analysis. Top Stroke Rehabil. 27(2):118-126. View
Steffen, T. M., Hacker, T. A., Mollinger, L. (2002). Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 82(2):128-137. View
Vaishya, R., Vaish, A. (2020). Falls in Older Adults are Serious. Indian J Orthop. 54(1):69-74. View
WHO global report on falls prevention in older age. The Library of Congress. Published 2015. Accessed April 2, 2025. View
Centers for Disease Control and Prevention (2021). Facts about falls. www.cdc.gov. View
Salari, N., Darvishi, N., Ahmadipanah, M., Shohaimi, S., Mohammadi, M. (2022). Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J Orthop Res. 17(1). View
Khalatbari-Soltani, S., Stanaway, F., Sherrington, C., et al. (2021). The Prospective Association Between Socioeconomic Status and Falls Among Community-Dwelling Older Men. J Gerontol A Biol Sci Med Sci. 76(10):1821-1828. View
U.S Centers for Disease Control and Prevention (2023). Socioeconomic factors. Centers for Disease Control and Prevention. Published September 1. View
Vafaei, A., Pickett, W., Zunzunegui, M. V., Alvarado, B. E. (2016). Neighbourhood social and built environment factors and falls in community-dwelling canadian older adults: A validation study and exploration of structural confounding. SSM - Population Health. 2:468-475. View
Zhou, Y., Zhou, L., Fu, C., et al. (2015). Socio-economic factors related with the subjective well-being of the rural elderly people living independently in China. Int J Equity Health. 14(1):5. View
Kim, T., Choi, S. D., Xiong, S. (2020). Epidemiology of fall and its socioeconomic risk factors in community-dwelling Korean elderly. Na KS, ed. PLoS ONE. 15(6):e0234787. View
Darmon, N., Drewnowski, A. (2015). Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 73(10):643-660. View
Harada, N. D., Chiu, V., Stewart, A. L. (1999). Mobility-related function in older adults: assessment with a 6-minute walk test. Arch Phys Med Rehabil. 80(7):837-841. doi:10.1016/s0003 9993(99)90236-8 View
Albalwi, A. A., Alharbi, A. A. (2023). Optimal procedure and characteristics in using five times sit to stand test among older adults: A systematic review. Medicine (Baltimore). 102(26):e34160. View
Bohannon, R. W., Shove, M. E., Barreca, S. R., Masters, L. M., Sigouin, C. S. (2007). Five-repetition sit-to-stand test performance by community-dwelling adults: A preliminary investigation of times, determinants, and relationship with self-reported physical performance. Isokinetics and Exercise Science.15(2):77-81. View
Nitz, J. C., Stock, L., Khan, A. (2013). Health-related predictors of falls and fractures in women over 40. Osteoporos Int. 24(2):613-621. View
Fritz, S., Lusardi, M. (2009). White paper:“walking speed: the sixth vital sign”. Journal of geriatric physical therapy. Jan 1;32(2):2-5. View
Bohannon, R. W., Andrews, A. W. (2011). Normal walking speed: a descriptive meta-analysis. Physiotherapy. 97: 182-189 View
Peters, D. M., Fritz, S. L., Krotish, D. E. (2013). Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 36(1):24-30. View
U.S. Centers for Disease Control and Prevention. (2024). Facts about Falls. Older Adult Fall Prevention. View
Newgard, C. D., Lin, A., Caughey, A. B., et al. (2020). The Cost of a fall among older adults requiring emergency services. J Am Geriatr Soc. 69(2):389-398. View
Siracuse, J. J., Odell, D. D., Gondek, S. P., et al. (2012). Health care and socioeconomic impact of falls in the elderly. Am J Surg. 203(3):335-338. View
Older adult falls data. Centers for Disease Control and Prevention. September 6, 2023. View
Pin, S., Spini, D. (2016). Impact of falling on social participation and social support trajectories in a middle-aged and elderly European sample. SSM - Population Health. 2:382-389. 18(1): 1.View
Rae, M., Claxton, G., Amin, K., Cox, C., Rakshit, S. (2024). The Burden of Medical Debt in the United States. Peterson-KFF Health System Tracker. Published February 12. View
Best Neighborhood. The Highest and Lowest Income Areas in Fort Myers, FL |BestNeighborhood.org. Best Neighborhood.
Kervio, G., Carre, F., Ville, N. S. (2003). Reliability and intensity of the six-minute walk test in healthy elderly subjects. Medicine & Science in Sports & Exercise. Jan 1;35(1):169-74. View
Kent State University. SPSS Tutorials: Pearson Correlation. Kent.edu. Published 2018. View
Andrade, C. (2019). The P Value and Statistical Significance: Misunderstandings, Explanations, Challenges, and Alternatives. Indian J Psychol Med. 41(3):210-215. doi:10.4103/IJPSYM. IJPSYM_193_19 View
Algas, U., Severinsen, K., Overgaard, K. (2012). Relations Between 6 Minute Walking Distance and 10 Meter Walking Speed in Patients With Multiple Sclerosis and Stroke. Archives of Physical Medicine and Rehabilitation. 93(7):1167-1172. View
Duncan, R. P., Combs-Miller, S. A., McNeely, M. E., et al. (2017). Are the average gait speeds during the 10meter and 6minute walk tests redundant in Parkinson disease?. Gait Posture. 52:178-182. View
Azharuddin, M., Zia, N.U. (2021). Correlation between sit-to stand ability, dynamic balance, gait speed, and quality of life in stroke population: a non-randomized pilot study. Bull Fac Phys Ther 26, 26. View
Triangto, I., Aulia Syavitri Dhamayanti, Putra, M. S., et al. (2025). Correlation of Sit-to-Stand Test and 6-Minute Walk Test to Illustrate Cardiorespiratory Fitness in Systolic Heart Failure Patients. Annals of Rehabilitation Medicine. 49(1):23 29. View
Castillo-Rodríguez, A., Onetti-Onetti, W., Sousa Mendes, R., Luis Chinchilla-Minguet, J. (2020). Relationship between Leg Strength and Balance and Lean Body Mass. Benefits for Active Aging. Sustainability. 12(6):2380. View
Yeh, P. C., De-Kai Syu, Ho C.C., Lee, T. S. (2024). Associations of lower-limb muscle strength performance with static and dynamic balance control among older adults in Taiwan. Frontiers in Public Health. 12. View
Beck Jepsen, D., Robinson, K., Ogliari, G., et al. (2022). Predicting falls in older adults: an umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatrics. 22(1). View