Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-172
https://doi.org/10.33790/jrpr1100172Research Article
Family-Based Support as a Social Determinant of Health-Protective Factor for Parents of Children with Autism Spectrum Disorder
Bisola E. Duyile1*, and Naomi Wheeler
1Assistant Professor, Department of Counseling, College of Community Health, Montclair State University, 1 Normal Ave. Montclair, NJ 07043, United States.
2Department of Counseling and Special Education, School of Education Virginia Commonwealth University, 1015 W. Main St., Richmond, VA 23284,United States.
Corresponding Author Details: Bisola E. Duyile, Assistant Professor, Department of Counseling, College of Community Health, Montclair State University, 1 Normal Ave. Montclair, NJ 07043, United States.
Received date: 09th May, 2025
Accepted date: 07th June, 2025
Published date: 09th June, 2025
Citation: Duyile, B. E., & Wheeler, N., (2025). Family-Based Support as a Social Determinant of Health-Protective Factor for Parents of Children with Autism Spectrum Disorder. J Rehab Pract Res, 6(1):172.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Parents of children with autism spectrum disorder (ASD) demonstrate resilience and resourcefulness in managing the demands of caregiving. This study highlights the critical role of familybased support as a social determinant of health-protective factor (SDHPF) that enhances the well-being of parents, helping to mitigate depressive symptoms. Using a secondary dataset of 199 parents/ caregivers of children with ASD, this study examines how familybased support, child symptom severity, and financial resources (income) influence parental mental health. The findings show that strong family support is positively associated with lower levels of depression, underscoring the strength of social networks in enhancing mental health. Results suggest that fostering family-based support systems can be a powerful tool in promoting resilience and reducing depression in parents of children with ASD. The study’s implications for professional development and training, clinical practice, and policy development focus on leveraging these strengths to further support the mental health of caregivers.
Key Words: Social Determinants of Health, Family-Based Support, Autism, Parents, Depression
Introduction
Parenting a child with autism spectrum disorder (ASD) presents significant challenges, including financial strain, time-related burdens, and social barriers [1]. Parents of children with disabilities report higher levels of stress and depression compared to parents of typically developing children [2]. These challenges are compounded by the social isolation that many parents experience due to limited resources and support systems [3]. Parents raising children with ASD face unique difficulties, such as navigating complex educational and medical systems and advocating for their children in multiple domains, including healthcare and school settings [4]. These stressors can significantly impact mental health and lead to symptoms of depression [5].
Despite the considerable distress these parents face, a dearth of resources exists aimed at supporting their mental health. While social support, particularly family-based support, has been shown to alleviate stress and depression in other caregiving populations, its role in mitigating depression in parents of children with ASD remains underexplored [6]. We aimed to address this gap by investigating how family-based support, as a social determinant of health (SDOH), influences depression in parents of children with ASD and whether financial resources and child symptom severity would moderate this relationship. The SDOH framework informs this study by emphasizing the various factors in individuals’ environments that impact their overall health and well-being. According to the Centers for Disease Control and Prevention [7], SDOH include conditions in the environments where people live, work, and play, which influence a wide range of health outcomes. Although there is an interconnectedness of all five SDOH domains: economic stability, education, social and community context, healthcare access and quality, and neighborhood environment [8], this study focuses on three domains of SDOH: (a) economic stability (financial resources), (b) social and community context (family-based support), and (c) health (severity of the child’s ASD symptoms). While ASD severity is not directly categorized as an SDOH, research indicates that child symptom severity can affect healthcare access and the quality of care a child receives, influencing both the child’s developmental outcomes and the emotional well-being of the parent [8]. These domains are particularly relevant for parents of children with ASD, as the interplay of economic and social factors significantly shapes their mental health outcomes, including the experience of depression.
We aimed to answer the following research questions: (a) How do SDOH protective factors, as measured by the Multidimensional Scale of Perceived Social Support [10] and Family Adjustment Measure [11], predict depression in parents of children with ASD? (b) How does child symptom severity (CSS) moderate the relationship between SDOH protective factors and depression? (c) How do financial resources moderate the relationship between SDOH protective factors and depression in parents of children with ASD?. The SDOH framework grounds our study hypotheses, which suggest that economic stability, social support, and access to healthcare influence mental health outcomes. Furthermore, the current study expands the application of the SDOH framework through a family systems level perspective on adjustment when a child has ASD, focusing specifically on the role of family-based support as a protective factor against depression.
Enhanced understanding of the influence of family-based support on the mental health of parents can inform professional training programs aimed at equipping future counselors and rehabilitation professionals to better support families that include a child with ASD. For practicing counselors, the results can guide treatment planning, particularly in recognizing the importance of family support in alleviating depression and as a resource associated with parental resilience. Additionally, the study has the potential to inform policies aimed at improving resources and services for families and parents of children with ASD, especially in areas related to social support and financial stability.
Literature Review
Autism Spectrum Disorder (ASD) and Its Impact on Families
ASD is a neurodevelopmental disorder characterized by persistent deficits in social communication and interaction, alongside restricted and repetitive patterns of behavior [12]. The prevalence of ASD has increased dramatically, with 1 in 36 children diagnosed in the United States [13]. The impact of ASD extends beyond the child to their families, with parents experiencing significant challenges in managing their child’s symptoms and navigating the various systems of care. These challenges include not only the child’s behaviors but also difficulties accessing appropriate educational and healthcare services [1]. Parents of children with ASD report higher levels of stress, anxiety, and depression compared to parents of children with other disabilities [2]. This stress is often exacerbated by the child’s symptoms, particularly behaviors such as aggression, hyperactivity, and sensory sensitivities, which are common in children with ASD [14]. Additionally, research has shown that depression significantly affects caregiving and parenting, often impairing a parent's ability to engage effectively with their child. Parents experiencing depression may endure increased stress, lower motivation, lack of energy, thinking about death, pessimism, a feeling of alienation, anxiety, and guilt symptoms, psychosomatic symptoms, reduced emotional availability, and lower self-regulation abilities, which can negatively impact caregiving quality [15-17]. The emotional burden can lead to increased isolation, decrease motivation to engage in social support groups or community programs and also impact their ability to receive external support as depression often reduces a parent’s ability to seek or utilize available resources [15, 18]. In addition, the financial and time-related burdens placed on parents as they seek therapies and educational interventions for their children contribute to increased levels of depression [19]. Furthermore, parental self-regulation plays a critical role in a child’s ability to regulate their own emotions and behaviors [20]. Given the impact of parental self-regulation on the child’s development, addressing protective factors for the depressive symptoms and emotional strain experienced by parents of children with ASD is essential in supporting not only their well-being but also their child’s emotional and behavioral regulation.
The Role of Social Support in Parental Mental Health
Social support has long been recognized as a protective factor against the negative effects of caregiving stress, particularly for parents of children with disabilities. Family-based support, defined as a network that includes immediate and extended family, friends, and other parents of children with disabilities [21], has been identified as a critical resource for parents of children with ASD. Research indicates that parents who report higher levels of social support experience lower levels of stress, anxiety, and depression [22, 23]. Support can come in many forms, including emotional, financial, and practical help with caregiving responsibilities [6]. Social support emerged as a critical factor in mitigating stress and improving the quality of life (QOL) for parents of adult children with ASD. Drogomyretska et al. [24] found that perceived social support from family and friends was the strongest protective factor against parental stress, and family-based support had a more significant impact than formal or professional support. Similarly, Marsack [25] demonstrated that family-based support reduced caregiver burden, enhancing QOL in older parents of children with ASD, emphasizing the importance of informal support in improving caregivers’ well-being. While prior research has consistently demonstrated the benefits of social support in alleviating stress and depressive symptoms [3, 6], the specific role of family-based support in mitigating depression in parents of children with ASD remains underexplored. Although studies have linked family support to lower levels of parental stress [18, 26, 27], fewer studies have examined its direct impact on mental health outcomes such as depression, particularly in the context of ASD caregiving.
However, despite the well-documented benefits of social support, many parents of children with ASD report feeling socially isolated due to the demands of caregiving and the lack of accessible support systems [3, 18, 28]. Moreover, family-based support is often informal and may be inconsistent, particularly for families in lower-income communities or those with limited access to healthcare [29]. Thus, understanding the mechanisms through which family-based support can alleviate depression is essential.
Social Determinants of Health and Parental Depression
The SDOH framework is particularly relevant for understanding the mental health of parents of children with ASD. Economic stability, including family income and access to financial resources, has been shown to be a key factor in the mental health of caregivers [30]. Parents with greater financial resources have more access to support services, which can reduce stress and mitigate depressive symptoms. Conversely, low income and financial instability can exacerbate stress and increase the likelihood of depression [6]. The social and community context, particularly family-based support, is another critical domain of SDOH that impacts the mental health of parents of children with ASD. Social support networks, including family, friends, and community resources, have been shown to buffer the effects of stress and reduce the incidence of depression in caregivers [31, 32]. However, access to these support networks is often uneven, with parents in lower-income or rural areas facing greater challenges in obtaining the support they need [33]. Lastly, the severity of the child’s ASD symptoms can also influence parental mental health outcomes. More severe symptoms are associated with higher levels of parental stress, which in turn increases the risk of depression [25]. Understanding how symptom severity interacts with social and economic factors to influence depression is a key focus of this study.
While much of the existing literature has focused on the relationship between CSS and parental stress, there is a gap in research exploring the role of family-based support as a protective SDOH factor for depression in parents of children with ASD. This study seeks to fill this gap by examining how family-based support, financial resources, and CSS interact to influence depression in this population. The findings will contribute to the growing body of literature on SDOH and provide practical implications for professionals and policymakers working with families of children with ASD.
Methodology
Research Design
We adopted a non-experimental, cross-sectional design using secondary data analysis. The researchers examined the relationship between social determinants of health-protective factors (SDHPF), specifically family-based support, and depression in parents of children diagnosed with ASD, as well as the moderation of this relationship by either family financial resources or CSS. The research approach is correlational, investigating how perceived social support and family-based support influence depression outcomes in these parents. We hypothesized a negative association between support and depressive symptoms that would be strengthened as CSS or family financial resources increased. The study uses convenience sampling from a dataset collected as part of a previously funded initiative aiming to assess the psychometric properties and family experiences of parents raising children with ASD. The study aims to examine these relationships in the context of SDOH and parental mental health, contributing to both the literature on ASD and the broader discourse on social determinants of health.
Sampling and Data Collection
The study utilized secondary data from an original study involving 253 participants, with data collected from the fall of 2018 to spring 2019. Participants were recruited through a collaboration with an autism-related organization in the United States. Inclusion criteria for the original study required participants to be at least 18 years old, currently parenting a child with ASD, and able to read and respond in English. Following data cleaning, 199 participants were retained for analysis. Data were collected using the REDCap electronic data capture tools hosted at [Virginia Commonwealth University][34], which ensured participant anonymity and included instruments for demographic information, the FAM [11], MSPSS [10], Patient Health Questionnaire-8 [35], and a researcher developed CSS Scale. The CSS measured the frequency of behaviors as reported in the DSM-5 [12]. There are several measures of symptom severity of ASD that studies have used to examine severity and to challenge behavior in other parent studies on ASD [36, 37]. However, few studies have specifically included the potential influence of differences in the frequency of ASD symptoms. The FAM is a 30- item scale that assesses family adjustment, including dimensions like parental distress, family-based support, and coping strategies. Items are rated on a five-point Likert scale from Never to Almost Always and include prompts such as “I feel supported by my spouse, partner, or significant other.” The MSPSS is a 12-item tool measuring the perception of social support from family, friends, and significant others with a seven-point Likert scale from Very Strongly Disagree to Very Strongly Agree on prompts like, “My friends really try to help me”. The PHQ-8 is an 8-item measure of depressive symptom frequency (e.g., “Feeling down, depressed, or hopeless”) ranging from Not at All to Nearly Every Day, with scores above 10 indicative of clinically significant depression. The CSS is a 3-item scale assessing the severity of ASD symptoms in the past 30 days on a sixpoint Likert from Strongly Disagree to Strongly Agree for symptoms such as aggression, communication, and repetitive behaviors. CSS scores ranged from three to 18, where lower scores infer less severe ASD-related symptoms in the past month. We totaled subscales for each measure and used total scores as manifest variables.
We used Structural Equation Modeling (SEM) to test the hypothesized relationships between SDHPF and depression. Additionally, we conducted moderation analyses to assess the roles of CSS and financial resources in these relationships. All predictor variables were mean-centered to reduce multicollinearity and improve interpretability.
Data Analysis
Before conducting the analyses, the researcher performed data cleaning to address missing data and outliers and check for assumptions of normality and linearity. Little’s Missing Completely at Random (MCAR) test indicated that data was missing at random (χ² = 1281.32, p = 0.773). About 9.4% of the data were missing, which was handled using pairwise deletion to minimize data loss and maintain statistical power. Income data, highly skewed with outliers, was transformed with a square root to improve normality, making the data suitable for use as a continuous variable in moderation analysis.
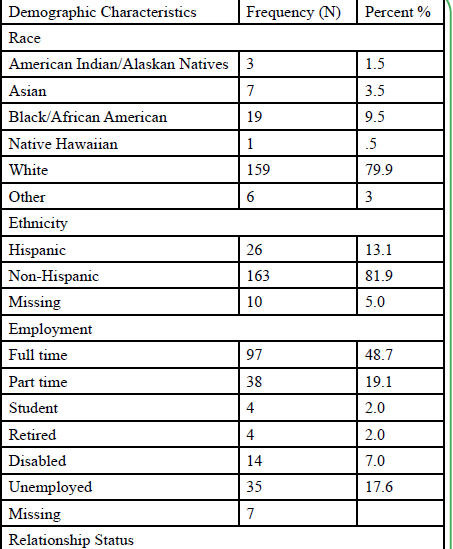
The sample was predominantly female (87.4%), White (79.9%), and married (74.4%). Ages ranged from 23 to 74 years, with a mean of 41.04 years (SD = 8.6). See Table 1. The average annual family income was $89,223, with significant skewness observed in the distribution. Post-transformation, income was used as a moderator in the analyses. On average, participants scored 9.24 on the PHQ- 8, with approximately 47.65% meeting the criteria for clinically significant depression (scores ≥ 10).
Confirmatory Factor Analysis (CFA) was used to assess the psychometric properties of the FAM and MSPSS scales. The results indicated that both the family-based support subscale of the FAM and the MSPSS subscales (family, friend, significant others) demonstrated good reliability, with factor loadings ranging from 0.73 to 0.92. The goodness of fit indices (RMSEA = 0.06, CFI = 0.95) suggested that the model fit the data well.
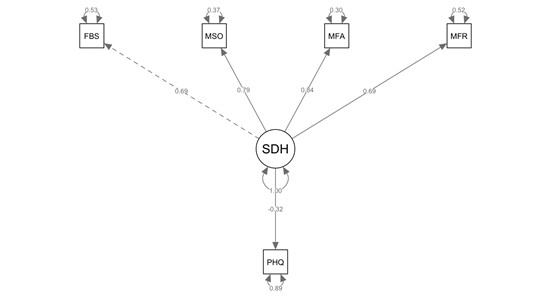
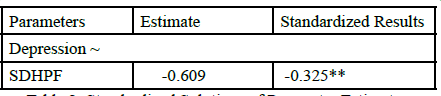
The final SEM model that included the relationship between SDHPF and depression indicated that family-based support was significantly associated with reduced depression (β = -0.609, p < 0.01). This supports the hypothesis that stronger family support is linked to lower depression levels in parents of children with ASD. See Figure 1 and Table 2 below.
Note. FBS refers to the Family Adjustment Measure Family-based support Subscale; MSO refers to the Multidimensional Scale of Perceived Social Support significant-other subscale; MFR refers to the Multidimensional Scale of Perceived Social Support friend subscale; MFA refers to the Multidimensional Scale of Perceived Social Support family subscale; SDH refers to latent social determinants of healthprotective factor; PHQ refers to the PHQ-8 symptoms of depression.
Note. SDHPF refers to the latent social determinants of healthprotective factor; ** denotes Pvalue < .01.
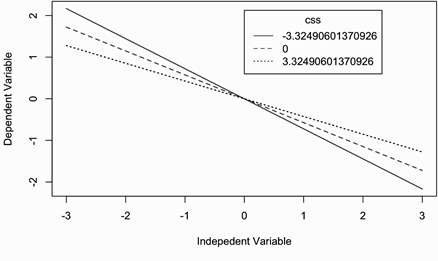
Moderation analysis examining CSS indicated that while CSS was positively associated with depression (β = 0.498, p < 0.001), it did not significantly moderate the relationship between SDHPF and depression (p > 0.05). The moderation analysis for financial resources showed that income did not significantly moderate the relationship between SDHPF and depression (p > 0.05).
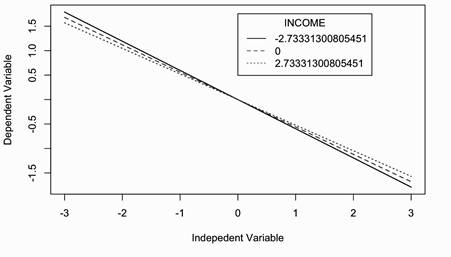
To further explore the moderation effects, we conducted a simple slope analysis to assess the interaction between CSS and income on depression. The purpose was to determine whether these variables had additive or interactive effects on depression, with a significant interaction indicating that the relationship between SDHPF and depression changes depending on the level of the moderator. Although the initial regressions showed no significant interaction, the post-hoc probe revealed exploratory insights. Specifically, at medium (mean) and high (+1 SD) levels of income, SDHPF significantly reduced depression (p < 0.01 and p < 0.05, respectively). This suggests that family-based support (SDHPF) is more effective at reducing depression when income is medium to high, although the effect at high income is only marginally significant. Similarly, low (-1 SD) and medium (0) levels of CSS were associated with a significant reduction in depression due to SDHPF (p < 0.01 for both). This indicates that family-based support significantly reduces depression for parents of children with ASD when the child's symptom severity is low to medium. See Figures 2 and 2.1 below
In summary, while income and CSS did not show a significant moderation effect in the initial analysis, further probing revealed that family-based support significantly reduced depression when income is medium/high or CSS is low/medium. These exploratory insights highlight the importance of strengthening social support systems for parents to alleviate depressive symptoms, which has significant implications for both clinical practice and policy aimed at supporting families of children with ASD. It is important to note the potential of a Type 1 error as a result of multiple comparisons during this simple slope analysis, which warrants caution in the interpretation of the moderation effects.
Discussion
We examined the role of informal and family-based support as an SDHPF for depression in parents of children with ASD. By analyzing the relationship between family-based support, CSS, and income, the study addresses a gap in existing literature on the mental health impacts of family-based support for parents of children with ASD and situates this research in the SDOH literature. The study used a secondary dataset of 199 parents (primarily biological parents, 91.33%) who completed a series of well-established instruments, including the Multidimensional Scale of Perceived Social Support (MSPSS), the Family Assessment Measure (FAM), and the Patient Health Questionnaire-8 (PHQ-8).
Family-Based Support as a Protective Factor
The results confirmed that family-based support significantly predicted lower levels of depression in parents of children with ASD. Our findings align with previous research showing that social support, particularly from family, protects against stress and depression [29]. Parents who reported higher levels of social support from family and friends experienced fewer depressive symptoms. These findings support the growing evidence that family-based support is a critical factor for enhancing mental health in caregivers of children with disabilities [24, 25].
Moderating Effects of Child Symptom Severity and Income
Contrary to the hypothesis, CSS did not significantly moderate the relationship between family-based support and depression in this study. While CSS was a significant predictor of depression, its interaction with family support did not show a strengthening effect of that association. The non-significant influence of CSS contrasts with prior studies indicating that more severe child behaviors (e.g., aggression, communication difficulties) exacerbated parental distress and depression [2, 38]. The failure to find a significant moderation effect may be due to the researcher-developed CSS scale, which primarily focused on behavior frequency rather than the intensity or functional impact of symptoms, limiting its sensitivity in capturing the full spectrum of child behaviors.
The study also found that income did not moderate the relationship between family-based support and depression. This is surprising, as financial resources are frequently cited as a key determinant of caregiver mental health in the ASD literature [39, 40]. The skewed distribution of income in this sample (predominantly uppermiddle- income) may have limited the variability needed to detect a significant moderating effect. Additionally, the high costs of raising a child with ASD may reduce the impact of income as a protective factor, suggesting that financial stability alone may not be sufficient to mitigate the psychological burdens faced by parents of children with ASD.
Implications
Professional Preparation
The results of this study emphasize the importance of incorporating SDOH into mental health and rehabilitation practitioner training programs. Educators must prioritize equipping future counselors and rehabilitation professionals with knowledge on the impact of family-based support on the mental health of parents, particularly those raising children with disabilities. Understanding how social support networks, whether family, friends, or community, can buffer against depression and stress is crucial for holistic approaches to work with families that include a child with ASD. Integrating SDOH frameworks into education and professional development programs can help students develop a holistic understanding of mental health [41, 42], particularly in diverse contexts where socioeconomic, cultural, and family dynamics play a pivotal role in shaping individuals’ well-being. By incorporating these frameworks into the curriculum, educators ensure that future practitioners are wellequipped to assess and understand the broader social context of their clients’ lives, health, and well-being.
In addition to SDOH training, integrating disability-specific training is essential. Educators should provide students with knowledge about the unique challenges faced by families of children with ASD, including navigating the healthcare and educational systems, managing caregiver stress, and dealing with the societal stigma that often surrounds disabilities. By recognizing the interconnected systems that act as social determinants, future counselors and rehabilitation practitioners can approach their work with cultural competence and empathy, tailored to meet the needs of families from varying socioeconomic backgrounds, cultural contexts, and lived experiences [43]. Furthermore, training should include practical skills for assessing family-based support as a potential resource for wellbeing. Future counselors should be equipped with the tools to use screening instruments such as the Multidimensional Scale of Perceived Social Support (MSPSS) and the Family Adjustment Measure (FAM) to assess family dynamics and the strength of social support systems. This knowledge and awareness of the importance of family dynamics equips counselors and rehabilitation professionals to design tailored interventions that address gaps in family support, enhance existing family support, and recommend appropriate related resources.
Practicing Counselors
For practicing counselors, the findings of this study suggest that family-based support could be integrated into the therapeutic process for families and parents of children with ASD. Based on evidence from SDOH research, including the findings of this study for the influence of family support for depressive symptoms, counselors can broaden case conceptualization beyond a singular focus on the individual and consider the family system as a whole when assessing and addressing mental health needs. Similarly, in other client populations who also tend to experience social isolation, social support demonstrated a significant effect for enhancing counseling outcomes [44]. Understanding how family relationships, social networks, and support systems impact mental health can enhance treatment outcomes for caregivers. Social support groups for parents of children with ASD can also serve as valuable resources. Counselors should consider recommending or facilitating participation in peer support groups, where parents can share experiences and receive emotional support from others facing similar challenges. Collaborations with ASDspecific organizations can also help families access information about therapies, legal rights, and community resources, reducing isolation and stress.
Counselors should therefore assess family dynamics early in the therapeutic relationship, identifying areas of strength and areas where additional prevention or intervention may be needed. Assessment of family dynamics can guide the development of treatment plans that leverage existing family strengths while addressing gaps in support. Indeed, family functioning predicted more positive developmental outcomes for children with ASD over time [45]. Family-based interventions could include strategies for improving communication, increasing positive family interactions, and strengthening supportive relationships between parents and extended family members or friends (similar to items assessed with the family-based support scale). Initial studies suggest that systemic interventions like relationship education, a multi-family group psychoeducation that teaches relationship skills like communication and conflict management, are effective to improve family adjustment among parents of a child with a disability [46].
Counselors could also use SDOH screeners (e.g., Accountable Health Communities (AHC) Health-Related Social Needs (HRSN) Screening tools) during intake assessments to identify the quality of family-based support and other factors, such as income, housing stability, and access to healthcare. These tools can provide valuable insights into how external factors are affecting a parent’s mental health, helping counselors to tailor their interventions more effectively. By incorporating these tools into their practice, counselors can ensure that they are considering all aspects of a parent’s life that may influence their mental health and well-being.
Policy and Social Justice Advocacy
Social justice advocates have an important role to play in promoting policies that expand access to family-based support services for parents of children with ASD. The findings of this study highlight the crucial role that family support plays in reducing parental depression, underscoring the need for comprehensive policy solutions that prioritize the well-being of caregivers. Policy interventions that address financial support and provide resources to reduce economic stressors could significantly enhance parents’ ability to engage with available support systems, ultimately improving caregiving and reducing depressive symptoms. Advocates should use the study’s findings to champion policies that provide financial support and increase access to mental health services for parents. One example of a policy that aligns with these findings is the Autism Family Caregivers Act (H.R. 6783/S. 4198). This legislation, which supports caregiver training and access to vital resources, would help to ease the mental health burden on families by providing structured support and resources to enhance the caregiving experience. Advocates should work at the state and regional levels to ensure that this policy is enacted and that caregiver programs are adequately funded to meet the needs of all families affected by ASD.
Limitations and Future Research
While this study provides valuable insights into the family-based support as an SDHPF for depression of parents of children with ASD, it has several limitations. The sample was homogeneous, with most participants being White, educated, middle-class, and female. This lack of diversity limits the generalizability of the findings. Additionally, the cross-sectional design of the study precludes causal inferences about the relationships between family-based support and depression. The CSS scale’s focus on frequency, rather than intensity or functional impact, also limits the study’s ability to fully assess the impact of CSS. Future studies can use more comprehensive scales prominent in ASD research, such as the Child Behavior Checklist [47] and Autism Diagnostic Observation Schedule (ADOS) severity scores [48]. To further probe the relationships, future researchers should employ longitudinal designs to observe how family-based support interacts with income and CSS. They can also track the effects of family-based support and other SDOH over time. Racial and ethnic minorities, as well as lower-income families, often face additional barriers to accessing resources, which can impact their ability to benefit from family-based supports. Therefore, larger and more diverse samples are needed to explore how family-based support and other SDOH factors, including educational attainment and access, operate across different socioeconomic, ethnic, and cultural groups. Additionally, more robust and validated instruments should be employed to assess CSS and family-based support in more detail, ensuring that all relevant aspects are captured.
Conclusions
This study provides strong evidence for the protective role of family-based support as a SDOH in reducing depression in parents of children with ASD. By highlighting the importance of social support networks, the study informs counseling and rehabilitation practice, education, and policy aimed at improving the mental health and quality of life for these parents. It also opens the door for future research to build on these findings and investigate broader social determinants that impact this population.
Competing interests:
The Authors have no competing interests to disclose.
References
Vohra, R., Goodall, E., & Tyler, G. (2014). The effects of parental stress on the mental health of caregivers of children with autism. Journal of Autism and Developmental Disorders, 44(4), 941-947. https://doi.org/10.1007/s10803-013-1953-6
Barańczuk, U., & Pisula, E. (2020). Parental stress and quality of life in parents of children with autism spectrum disorder: The role of child-related factors and family functioning. Journal of Autism and Developmental Disorders, 50(3), 937-947. https:// doi.org/10.1007/s10803-019-04149-z
Meadan, H., Sarris, A., & Munda, K. (2010). Parent stress and coping with children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 40(3), 357-373. https:// doi.org/10.1007/s10803-009-0886-5
Tomeny, T. S. (2016). Examining the link between autism spectrum disorder and parental mental health: A review of the literature. Journal of Autism and Developmental Disorders, 46(4), 1229-1240. https://doi.org/10.1007/s10803-015-2672-5
Cohrs, D. C., & Leslie, L. A. (2017). Parental depression and its relationship to children with autism spectrum disorder: A review of the literature. Journal of Child and Family Studies, 26(10), 2815-2825. https://doi.org/10.1007/s10826-017-0800-9
Ekas, N. V., Whitman, T. L., & Shivers, C. M. (2016). The role of social support in the mental health of parents of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(3), 888-897. https://doi.org/10.1007/s10803-015- 2611-5
Centers for Disease Control and Prevention (CDC). (2020). Social determinants of health: Know what affects health.View
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. (n.d.). Healthy People 2030.View
Dababnah, S., & Parish, S. L. (2016). Feasibility of an empirically based program for parents of preschoolers with autism spectrum disorder. Autism: The International Journal of Research and Practice, 20(1), 85–95.View
Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30-41.View
Daire, A. P., Jennings, R. M., & Lee, J. Y. (2014). Family adjustment to autism spectrum disorders: The impact on parents’ mental health. Journal of Family Social Work, 17(4), 309-324. https://doi.org/10.1080/10522158.2014.946377
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).View
Maenner, M. J., Warren, Z., Williams, A., Amoakohene, E., Bakian, A. V., Bilder, D. A., Durkin, … & Shaw, K. A (2023). Prevalence and characteristics of autism spectrum disorder among children aged 8 years — autism and developmental disabilities monitoring network, 11 sites, United States, 2020. MMWR. Surveillance Summaries, 72(2), 1–14. https://doi. org/10.15585/mmwr.ss7202a
O’Connor, R., Langer, A., & Tompson, M. (2017). The impact of child behavior on parental mental health. Journal of Autism and Developmental Disorders, 47(6), 1778-1793.View
Foody, C., James, J. E., & Leader, G. (2015). Parenting stress, salivary biomarkers, and ambulatory blood pressure: A comparison between mothers and fathers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45(4), 1084–1095.View
Lovell, B., & Wetherell, M. A. (2020). Exploring the moderating role of benefit finding on the relationship between child problematic behaviours and psychological distress in caregivers of children with ASD. Journal of Autism and Developmental Disorders, 50(2), 617–624.View
Pisula, E., & Porębowicz-Dörsmann, A. (2017). Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PLOS ONE, 12(10), e0186536.View
Guan, Z., Abner, E. L., & Zwi, A. B. (2023). Social isolation and loneliness in family caregivers of people with severe mental illness: A scoping review. American Journal of Community Psychology, 72(3–4), 380–398.View
Delobel-Ayoub, M., Ehlinger, V., Klapouszczak, D., Maffre, T., Raynaud, J. P., Delpierre, C., & Arnaud, C. (2015). Socioeconomic disparities and prevalence of autism spectrum disorders and intellectual disability. PLoS ONE, 10(11), e0141964.View
Duyile, B. E., LoCasale-Crouch, J., NeSmith, T. B., Turnbull, K. L. P., Colson, E., Corwin, M. J., Mateus, M. C., Forbes, E., Geller, N., Heeren, T., Hauck, F. R., Jaworski, B., Kellams, A., Kerr, S., & Moon, R. Y. (2024). Maternal education and child self-regulation: Do maternal self-regulation and responsiveness mediate the association? Department of Counseling Scholarship and Creative Works.View
\ Mesibov, G. B., & Schopler, E. (1983). The development of community-based programs for autistic adolescents. Children’s Health Care, 12(1), 20–24.View
Merz, E. C., & Huxhold, O. (2010). Social support, stress, and depression among parents of children with disabilities. American Journal of Orthopsychiatry, 80(1), 91-98.View
Lindsey, R. A., & Barry, T. D. (2018). Protective factors against distress for caregivers of a child with autism spectrum disorder. Journal of Autism and Developmental Disorders, 48(4), 1092– 1107.View
Drogomyretska, K., Fox, R., & Colbert, D. (2020). Brief report: Stress and perceived social support in parents of children with ASD. Journal of Autism and Developmental Disorders, 50, 4176–4182.View
Marsack, S. L. (2017). The relationship between parental stress and mental health in families of children with autism spectrum disorder. Research in Autism Spectrum Disorders, 41, 14-25. https://doi.org/10.1016/j.rasd.2017.06.004
Parkes, A., Sweeting, H., & Wight, D. (2015). Parenting stress and parent support among mothers with high and low education. Journal of Family Psychology, 29(6), 907–918.View
Respler-Herman, M., Mowder, B. A., Yasik, A. E., & Shamah, R. (2012). Parenting beliefs, parental stress, and social support relationships. Journal of Child and Family Studies, 21(2), 190– 198.View
Samsell, B., Lothman, K., Samsell, E. E., & Ideishi, R. I. (2022). Parents’ experiences of caring for a child with autism spectrum disorder in the United States: A systematic review and metasynthesis of qualitative evidence. Families, Systems, & Health, 40(1), 93–104.View
Yu, S., Kowitt, S. D., Fisher, E. B., & Li, G. (2017). Mental health in China: Stigma, family obligations, and the potential of peer support. Community Mental Health Journal, 54(6), 757– 764.View
Janssen, M. (2019). Financial stress and its impact on the mental health of parents raising children with autism. Autism Research, 12(2), 245-253.View
Mo, S., Bu, F., Bao, S., & Yu, Z. (2024). Comparison of effects of interventions to promote the mental health of parents of children with autism: A systematic review and network metaanalysis. Clinical Psychology Review, 114, 102508.View
Zaidman-Zait, A., Mirenda, P., Duku, E., Vaillancourt, T., Smith, I. M., Szatmari, P., Bryson, S., Fombonne, E., Volden, J., Waddell, C., Zwaigenbaum, L., Georgiades, S., Bennett, T., Elsabbagh, M., & Thompson, A. (2017). Impact of personal and social resources on parenting stress in mothers of children with autism spectrum disorder. Autism, 21(2), 155–166.View
Singh, A., Seligman, M., & Kim, Y. (2017). The role of social support in the mental health of parents of children with autism spectrum disorder. Autism Research, 10(5), 923-934.View
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377-81.View
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606-613.View
Giovagnoli, G., Postorino, V., Fatta, L. M., Sanges, V., De Peppo, L., Vassena, L., Rose, P. D., Vicari, S., & Mazzone, L. (2015). Behavioral and emotional profile and parental stress in preschool children with autism spectrum disorder. Research in Developmental Disabilities, 45–46, 411–421.View
Wayment, H. A., Al-Kire, R., & Brookshire, K. (2018). Challenged and changed: Quiet ego and posttraumatic growth in mothers raising children with autism spectrum disorder. Autism, 23(3), 607–618.View
McStay, R. L., Dissanayake, C., Scheeren, A., Koot, H. M., & Begeer, S. (2014). Parenting stress and autism: The role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism: The International Journal of Research and Practice, 18(5), 502–510.View
Adak, B., & Halder, S. (2017). Systematic review on prevalence for autism spectrum disorder with respect to gender and socioeconomic status. Journal of Mental Disorders and Treatment, 3(1), Article 133.View
Buescher, A. V., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics, 168(8), 764-770.View
Johnson, K. F., Rumbidzai, M., Norris, M., DeWitt, J., & Marulli, T. (2024). Evaluating social determinants of health competency of rehabilitation clinical staff and students. Rehabilitation Research, Policy, and Education, 38(1).View
Robins, L., Johnson, K., Duyile, B., Gantt-Howrey, A., Dockery, N., Robins, S., & Wheeler, N. (2022). Family counselors addressing social determinants of mental health in underserved communities. Family Journal.View
Lozada, F., Wheeler, N. J., Castro, A., Gomez, R., & Green, M. (2024). An ecologically-informed transdisciplinary prevention model for Black and Latine family wellbeing. Journal of Counseling and Development, 102(2), 210-225. View
Robbins, K. A., Bartholomew, T. T., Joy, E. E., TaeHyuk Keum, B., Perez-Rojas, A. E., & Lockard, A. J. (2024). Social support and psychotherapy outcomes for international students in university/college counseling centers. Journal of American College Health.View
Szatmari, P. Tombeau Cost, K., Duku, E., Bennett, T., Elsabbagh, M., Georgiades, S., Kerns, C. , … & Zwaigenbaum, L. (2021). Association of child and family attributes with outcomes in children with Autism. JAMA Network Open, 4(3).View
Wheeler, N. J., Kozachuk, L., Man, J., & Pointer, A. (2024). Exploring family adjustment among parents of a child with a disability in relationship education. Family Journal, 32(3), 471- 480.View
Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA preschool forms & profiles. University of Vermont, Research Center for Children, Youth, & Families.
Shumway, S., Farmer, C., Thurm, A., Joseph, L., Black, D., & Golden, C. (2012). The ADOS calibrated severity score: Relationship to phenotypic variables and stability over time. Autism Research, 5(4), 267–276.View