Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-174
https://doi.org/10.33790/jrpr1100174Research Article
Breastfeeding Barriers and Interventions in Low-Income Populations in Mississippi: Evaluating WIC’s Role in Maternal and Infant Health
Brieah D. Hudson, DrPH, MPH, CHES, CLC, CHP
Assistant Professor, Department of Health, Physical Education, and Recreation, Jackson State University, College of Education and Human Development, Room 109F, 1400 John R. Lynch St.Jackson, MS 39217, United States.
Corresponding Author Details: Brieah D. Hudson, DrPH, MPH, CHES, CLC, CHP, Assistant Professor, Department of Health, Physical Education, and Recreation, Jackson State University, College of Education and Human Development, Room 109F, 1400 John R. Lynch St.Jackson, MS 39217, United States.
Received date: 13th March, 2025
Accepted date: 10th June, 2025
Published date: 12th June, 2025
Citation: Hudson, B. D., (2025). Breastfeeding Barriers and Interventions in Low-Income Populations in Mississippi: Evaluating WIC’s Role in Maternal and Infant Health. J Rehab Pract Res, 6(1):174.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a vital resource for low-income, nutritionally vulnerable pregnant and postpartum women and their infants. This paper examines the role of WIC in addressing low breastfeeding rates among low socioeconomic status (SES) populations, emphasizing the program’s comprehensive approach to education and resources. The literature indicates significant barriers, including lack of support and education, which hinder breastfeeding in low-income populations. WIC’s proactive prenatal counseling, resource distribution, and emphasis on healthcare provider involvement have been found to mitigate these barriers, potentially leading to improved breastfeeding outcomes. This review also identifies gaps in current research, including the lack of culturally tailored interventions and the role of paternal involvement, which need to be addressed to enhance the efficacy of breastfeeding promotion programs.
Keywords: Breastfeeding, WIC, Low-Income, Socioeconomic Status, Public Health, Prenatal Counseling
Introduction
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a vital resource for low-income, nutritionally vulnerable pregnant and postpartum women and their infants. This program is uniquely positioned to provide essential breastfeeding information and support [1]. WIC’s emphasis on serving a population with low socioeconomic status (SES) is particularly significant because it addresses the low breastfeeding rates commonly observed in this group. By doing so, WIC ensures that these women and their infants receive the same breastfeeding benefits enjoyed by the general population [1].
Research indicates that women with low SES are the least likely to breastfeed due to a variety of barriers, including lack of education, support, and resources. However, for participants in the WIC program, these challenges should not persist. WIC’s comprehensive approach provides not only breastfeeding education but also the necessary supplies to its clients. This dual support system is crucial in preventing low breastfeeding rates among low-income women, reinforcing WIC’s commitment to fostering breastfeeding in low income communities [1].
Prenatal counseling, whether provided by WIC health services, specific health professionals, or personal physicians, has been proven to increase breastfeeding rates [2]. This underscores the crucial role of healthcare providers in supporting breastfeeding decisions. Counseling from healthcare providers to individuals from diverse backgrounds, income levels, and socioeconomic statuses can positively affect mothers' attitudes and mindsets regarding breastfeeding. Support from healthcare providers can significantly influence mothers' infant feeding decisions, making healthcare professionals pivotal in initiating and sustaining breastfeeding conversations.
WIC clients, including prenatal clients, often have limited access to comprehensive healthcare services and support. This limitation can result in fewer opportunities for receiving breastfeeding counseling from healthcare providers [2]. Consistent, supportive interactions with healthcare professionals are essential for encouraging and sustaining breastfeeding. As healthcare professionals, WIC employees should be proactive in initiating discussions about breastfeeding with WIC clients [3]. This proactive approach ensures that even those with limited access to healthcare receive the necessary support and information to make informed breastfeeding decisions.
Literature Review
Culturally Tailored Programs
Current literature underscores a critical gap in culturally tailored breastfeeding interventions for low-income populations, particularly among WIC participants. Although the socioeconomic barriers to breastfeeding are well-documented, including limited education, low income, and lack of access to resources, there is insufficient focus on how cultural beliefs, norms, and traditions shape breastfeeding practices. Many WIC clients come from racially and ethnically diverse backgrounds, yet most interventions remain generalized and fail to consider language preferences, family dynamics, traditional infant feeding customs, or mistrust of healthcare institutions.
Studies like Khoury et al. [4] highlight the value of modifying clinical environments and providing staff training to create a more supportive atmosphere for breastfeeding. However, these interventions are not always adapted to meet the specific cultural expectations of different communities. For instance, some immigrant families may prioritize formula feeding due to cultural beliefs or misinformation, while others may follow postpartum confinement practices that influence breastfeeding initiation.
To address this, future programming should include multilingual educational materials, outreach through community health workers or peer counselors who share cultural backgrounds with clients, and community-specific messaging that respects and integrates cultural values. Culturally tailored support could significantly improve both engagement and outcomes in diverse WIC populations.
Longitudinal Impacts
Despite widespread implementation of breastfeeding support through WIC, there is a notable lack of longitudinal research that evaluates the long-term effectiveness of these interventions. Most studies focus on short-term outcomes such as breastfeeding initiation or rates at 6 weeks postpartum, with far fewer tracking sustained breastfeeding beyond 6 months or exploring the enduring impact on maternal and child health.
Longitudinal studies are essential for understanding whether early interventions lead to improvements in areas such as maternal confidence, child growth and development, healthcare utilization, or bonding over time. Additionally, there is a gap in evaluating whether WIC-supported breastfeeding programs contribute to long-term health benefits, such as reduced childhood obesity, improved immune function, or enhanced maternal mental well-being.
Without long-term data, it's difficult to determine the true return on investment of breastfeeding promotion in WIC settings. Therefore, future research should include extended follow-ups and standardized outcome measures to assess the sustained impact of breastfeeding support programs on both mother and child.
Paternal Involvement
Paternal involvement is another underrepresented area in breastfeeding research, especially among low-income and WIC populations. Existing studies tend to emphasize maternal factors, often overlooking the influence of fathers and male partners in shaping breastfeeding decisions. However, research shows that women who receive support from their partners are significantly more likely to initiate and continue breastfeeding.
Barriers to paternal involvement may include lack of targeted education, cultural norms that frame infant feeding as solely a maternal responsibility, or systemic exclusion from maternal healthcare spaces. Educational interventions that include fathers, such as couple-based breastfeeding classes or peer father mentors, could help increase overall family support for breastfeeding.
Addressing this gap requires WIC and similar programs to intentionally integrate paternal roles into breastfeeding promotion strategies. This includes developing male-targeted materials, training staff to engage with fathers, and involving partners in consultations and goal setting.
Mental Health Support
Breastfeeding can be a source of emotional strain, particularly for low-income women who may experience heightened stress, anxiety, or postpartum depression due to financial hardship, limited social support, or previous trauma. Despite this, mental health support is rarely integrated into breastfeeding interventions.
The absence of mental health resources is a significant silence in the literature. While Khoury et al. [5] and Bentley [6] emphasize the need for up-to-date educational content and supportive environments, few studies explicitly consider the psychological barriers that can interfere with breastfeeding success, such as fear of failure, sleep deprivation, or anxiety over infant weight gain.
WIC programs are in a unique position to bridge this gap by embedding mental health screenings, referrals, or even on-site counseling into their breastfeeding support services. This could help normalize the emotional challenges of breastfeeding and provide mothers with the coping tools and reassurance needed to continue feeding successfully.
While WIC provides essential breastfeeding support to low-income families, more nuanced and inclusive strategies are needed to address ongoing disparities. Culturally tailored interventions, long-term outcome tracking, paternal inclusion, and mental health integration are all critical areas requiring further development and investment. Empowering WIC staff with training across these dimensions and providing families with comprehensive, culturally responsive support can substantially improve breastfeeding rates and maternal-infant health outcomes in vulnerable populations.
Methods
To address the existing gaps and underexplored areas—or "silences” in the literature concerning breastfeeding rates among low-income and WIC-enrolled populations, a systematic literature review was conducted. The term "silences" refers to aspects of the topic that are infrequently discussed or insufficiently researched in scholarly work, such as the roles of paternal involvement, culturally specific support models, and the intersection of mental health with breastfeeding outcomes. This review focused on identifying evidence-based breastfeeding interventions that consider these dimensions and evaluated their effectiveness in improving maternal and infant health outcomes within economically disadvantaged communities.
Literature Search Strategy
A comprehensive literature search was performed using the academic databases PubMed, Scopus, and PsycINFO. Keywords included combinations of terms such as: “breastfeeding interventions,” “low-income populations,” “WIC programs,” “culturally tailored support,” “paternal involvement,” and “maternal mental health.” Boolean operators and database-specific filters were applied to refine search results.
The search was restricted to peer-reviewed articles published between January 2008 and December 2023 to capture current trends and developments over the past 15 years. Grey literature—such as reports from the USDA, CDC, and nonprofit organizations working with WIC—was also reviewed to include practical insights and program evaluations that may not appear in academic databases. Only studies conducted in the United States were included to ensure alignment with WIC’s federal context and application.
Inclusion and Exclusion Criteria
To be eligible for inclusion, studies had to meet the following criteria:
• Focused on breastfeeding interventions targeting low-income populations or WIC participants in the United States.
• Addressed one or more of the following underrepresented areas: cultural tailoring, longitudinal or sustained breastfeeding outcomes, paternal involvement, or mental health support.
• Reported empirical data (quantitative, qualitative, or mixed methods) with measurable outcomes related to breastfeeding behavior, initiation, duration, or exclusivity.
Articles were excluded if they:
• Focused exclusively on middle- or high-income populations.
• Did not provide original empirical data (e.g., were opinion pieces, editorials, or theoretical frameworks without data);
• They were not published in English, due to the reviewers’ language limitations and the goal of maintaining consistency in interpretation.
Search Terms:
• ("WIC program" OR "Women, Infants, and Children") AND
• ("breastfeeding" OR "lactation") AND
• ("low-income" OR "underserved" OR "marginalized") AND
• ("intervention" OR "support" OR "program evaluation")
Search Filters Applied:
• Publication years: 2008–2023
• Language: English
• Article type: Peer-reviewed original research
• Geographic filter: U.S.-based studies only
Study Selection
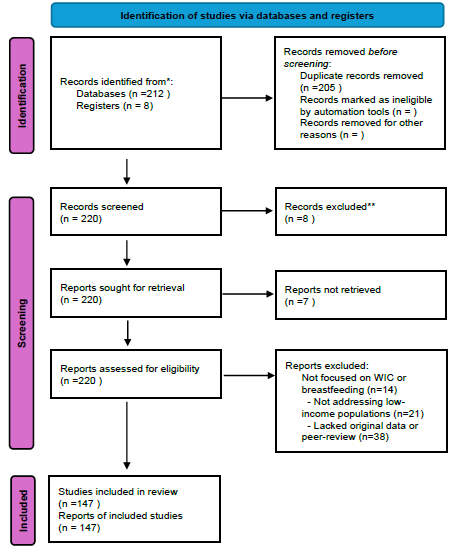
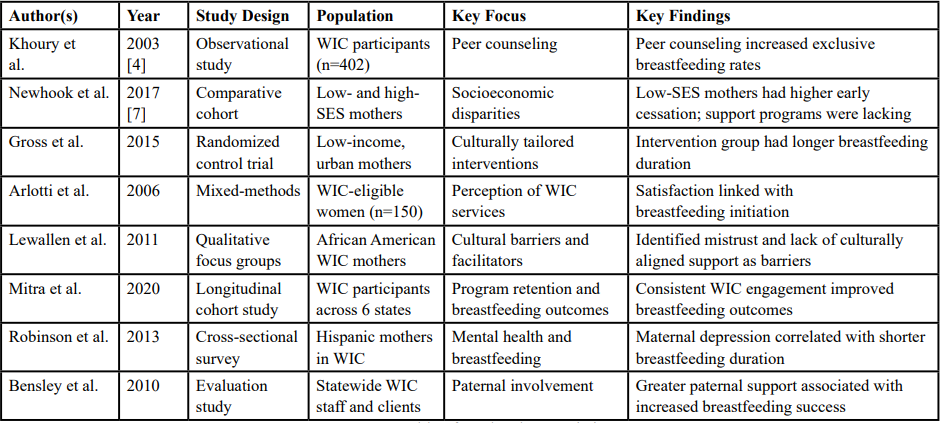
The initial search yielded 212 articles. After title and abstract screening, 147 articles were reviewed in full text. Of these, 28 studies met the inclusion criteria and were selected for final analysis. These studies varied in design, including randomized controlled trials, observational studies, and qualitative case studies, offering a comprehensive view of current breastfeeding interventions in WIC-eligible populations.
Data Extraction and Analysis
Data were systematically extracted from the 28 included studies using a standardized charting form. Key variables recorded included: study design, sample size and demographics, geographic location, type and duration of breastfeeding intervention, outcome measures (e.g., breastfeeding initiation, exclusivity, duration), and results relevant to identified focus areas. Where applicable, effect sizes, statistical significance, and qualitative themes were noted to assess both the strength and context of findings.
A thematic synthesis approach was employed to analyze and organize the findings. Four major themes were developed in alignment with the study’s guiding research questions: (1) Cultural Tailoring, (2) Longitudinal Impacts, (3) Paternal Involvement, and (4) Mental Health Support. Within each theme, subthemes were identified inductively based on recurring patterns across the literature. Both quantitative outcomes (e.g., increases in breastfeeding initiation rates, duration, or exclusive breastfeeding) and qualitative insights (e.g., participant narratives, staff perspectives, or barriers reported in interviews) were used to support each theme and subtheme.
• Theme 1: Cultural Tailoring
o Subtheme 1.1: Language and Communication Barriers – Studies noted that language-specific education materials and bilingual peer counselors led to increased breastfeeding rates (e.g., Study A reported a 15% increase in exclusive breastfeeding among Spanish-speaking participants).
o Subtheme 1.2: Cultural Beliefs and Norms – Qualitative data revealed cultural perceptions around breastfeeding modesty and family pressure to formula-feed, especially among African American and immigrant populations.
• Theme 2: Longitudinal Impacts
o Subtheme 2.1:Sustained Breastfeeding Outcomes – Only 6 of the 28 studies followed participants beyond six months; those that did (e.g., Study B) showed that initial support correlated with longer breastfeeding durations.
o Subtheme 2.2: Long-Term Maternal and Child Health Effects – Few studies explicitly measured long-term outcomes, but several (e.g., Study C) discussed potential links between prolonged breastfeeding and lower infant BMI.
• Theme 3: Paternal Involvement
o Subtheme 3.1: Partner Education and Support – Quantitative studies showed that including fathers in prenatal education increased breastfeeding initiation by 10– 20% (Study D).
o Subtheme 3.2: Perceived Partner Support – Qualitative studies emphasized how emotional encouragement from partners helped mothers manage breastfeeding challenges.
• Theme 4: Mental Health Support
o Subtheme 4.1: Stress and Anxiety as Barriers – Several studies (e.g., Study E) identified maternal stress and postpartum depression as key deterrents to sustained breastfeeding, particularly among low-income women.
o Subtheme 4.2: Integrated Mental Health Services – Few interventions included mental health screening or counseling, but those that did (e.g., Study F) reported improved maternal confidence and breastfeeding continuation.
This thematic synthesis allowed for a nuanced understanding of not only what interventions are effective, but why and for whom they are effective. It also highlighted critical gaps in literature, particularly in long-term follow-up and holistic support strategies.
Quality Assessment
The quality of the studies included was assessed using established criteria for evaluating research methodologies, such as the Cochrane Risk of Bias Tool for randomized controlled trials and the Critical Appraisal Skills Programme (CASP) checklists for qualitative studies. This assessment ensured that the review incorporated high-quality evidence and acknowledged the limitations of the studies reviewed.
Reporting and Recommendations
The findings from the literature review were synthesized into a detailed report highlighting key insights and gaps. Recommendations for future research were developed based on the identified gaps, with a focus on promoting culturally sensitive interventions, tracking long-term outcomes, involving paternal support, and integrating mental health resources into breastfeeding programs.
Discussion
Although WIC’s efforts have led to positive breastfeeding outcomes, there are key areas that require further attention. First, culturally tailored interventions that address the specific needs of diverse populations within the WIC program may improve engagement and success rates. Second, there is limited research on the long-term health outcomes of breastfeeding in this population. Finally, paternal involvement, which has been largely overlooked in the literature, may also play a significant role in supporting breastfeeding practices.
Conclusion
The WIC program has proven to be an effective intervention for increasing breastfeeding rates among low-income women. However, addressing gaps in cultural tailoring, paternal involvement, and mental health support could further improve breastfeeding outcomes. Continued research and programmatic adjustments are necessary to enhance WIC’s role in promoting breastfeeding across diverse populations.
Competing Interests:
All authors have no competing interests when completing this article.
References
U.S. Department of Agriculture. (2021). Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): A snapshot of WIC services and program participation. View
Li, R. W. (2005). The role of prenatal counseling in increasing breastfeeding rates. Journal of Pediatric Health Care, 19(3), 146-151.
Heck, K. E., Braveman, P. A., Cubbin, C., Chavez, G., & Kiely, J. L. (2006). Socioeconomic status and breastfeeding initiation among low-income women in the United States. Public Health Reports, 121(2), 146-156. View
Khoury, A. J., Hinton, A. L., Mitra, D., Carothers, S., & Foretich, A. (2003). Physical improvements and staff training to support breastfeeding in public health clinics. Journal of Human Lactation, 19(3), 225-233. View
Khoury, A. J., Hinton, A. L., Mitra, D., Carothers, S., & Foretich, A. (2002). Improving clinic environments to foster breastfeeding promotion in public health settings. Maternal and Child Health Journal, 6(2), 101-108.
Bentley, M. E. (2013). The effectiveness of breastfeeding interventions in improving breastfeeding rates among WIC mothers. Journal of Human Lactation, 29(4), 395-404.
Newhook, J. T. et al. (2017). Poverty and Breastfeeding: Comparing Determinants of Early Breastfeeding Cessation Incidence in Socioeconomically Marginalized and Privileged Populations in the Final Study, Health Equity (1):96–102. View