Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-177
https://doi.org/10.33790/jrpr1100177Research Article
Practice Patterns in Pediatric and Adult Dysphagia: Implications for Clinical Training
Jane Grothaus1, Kaitlyn Hill2, Marlee Nebesniak1, Anastasia Raymer2*
1Department of Communication Disorders, University of Nebraska-Kearney, United States.
2School of Speech-Language Pathology, Old Dominion University, United States.
Corresponding Author Details: Anastasia Raymer, Ph.D., Professor, School of Speech-Language Pathology, Old Dominion University, 4501 Hampton Blvd, Norfolk, VA 23529, United States.
Received date: 20th May, 2025
Accepted date: 23th June, 2025
Published date: 25th June, 2025
Citation: Grothaus, J., Hill, K., Nebesniak, M., & Raymer, A., (2025). Practice Patterns in Pediatric and Adult Dysphagia: Implications for Clinical Training. J Rehab Pract Res, 6(1):177.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Most speech language pathologists (SLPs) receive training to work with patients with swallowing disorders in graduate school, focusing primarily on adult dysphagia. Although SLPs share common foundational knowledge and skills for adult and pediatric dysphagia populations, there are considerable differences in these two specialized areas of practice. We aimed to query SLPs’ practice patterns for dysphagia assessment and management for adults and pediatric populations to consider differences and guide training efforts.
Methods: We distributed two comprehensive anonymous surveys to explore practice patterns of SLPs who provide assessment and management of dysphagia for adult or pediatric populations. The 118 respondents, 62 for the adult survey and 56 for the pediatric survey, completed five-point Likert scale questions about how often they address swallowing across aspects of clinical practice and use several assessment tools and management techniques for dysphagia.
Results: Assessment patterns were similar for the adult and pediatric surveys as clinical swallowing evaluation and video fluoroscopic swallowing studies were most commonly used. Several other assessment tools were rarely used in clinical practice. Management techniques for adult and pediatric populations varied considerably as pediatric techniques focused on oral-motor development, posturing, and food acceptance, while adult intervention primarily used effortful swallows and oral motor exercises.
Conclusions: Our results provide a greater understanding of practice patterns of SLPs working with adults and pediatric patients with dysphagia and inform future areas of focus in clinical training for preservice and in-service SLPs.
Key words (3-5): Dysphagia, Pediatric Patients, Adult Patients, Training in Graduate School
Introduction
One common side effect of many medical conditions, including neurologic, structural, and genetic, is swallowing difficulty or dysphagia [1]. Based on U.S. population estimates in 2022, dysphagia affects more than 15 million individuals [2]. Likewise, pediatric dysphagia has been reported to occur in 500,000 infants and young children each year in the U.S [3]. Pediatric dysphagia often results from congenital factors, developmental issues, or neurological conditions present from birth or acquired during early childhood [4]. Adult dysphagia is more commonly associated with age-related conditions such as neurological diseases and structural problems of the larynx and esophagus.
Dysphagia presents unique challenges in both pediatric and adult populations. These individuals have difficulty swallowing food, liquids, or saliva. This can lead to various complications, including choking, aspiration (food or liquids entering the airway), weight loss, dehydration, malnutrition, respiratory issues (such as pneumonia due to aspiration), and reduced quality of life. Assessing and treating dysphagia in adults and children involves distinct considerations due to differences in anatomy, physiology, cognitive development, communication abilities, and overall health.
Some of the routine assessment procedures used in children and adults with suspected dysphagia are a thorough non-instrumental clinical evaluation [5, 6] as well as instrumental techniques such as video fluoroscopic swallow study (VFSS) or fiber-optic endoscopic evaluation of swallowing (FEES) [7, 8]. Several other assessment tools, such as rating scales (e.g., Penetration-Aspiration Scale [9]; Dysphagia Outcome and Severity Scale [10]) and standardized instruments (e.g., Mann Assessment of Swallowing Ability [11], have been described to document feeding and swallowing impairments and monitor changes over time.
Likewise, several treatment techniques have been described to address swallowing difficulties that occur across the lifespan. Many techniques are intended to foster development or restoration of feeding and swallowing skills, while others promote use of strategies to support swallowing safety and nutrition. Dysphagia management often requires a family-centered approach, involving parents and caregivers in therapy and making dietary modifications [12, 13]. Interventions for children may focus on improving direct oral sensorimotor interventions to foster developmental skills, feeding techniques, and strategies to modify postures and food textures to facilitate food acceptance and safe swallowing [14]. Adult dysphagia management can include dietary texture modifications, postural adjustments, sensorimotor swallowing exercises, electrical stimulation, and medical or surgical interventions, depending on the underlying cause [5,15,16]. Pediatric dysphagia management requires consideration of growth and development, while in adults, the focus may be on maintaining or improving the quality of life and preventing complications of dysphagia and aspiration.
Often, speech-language pathologists (SLPs) are the primary practitioners called upon when a patient is suspected of having dysphagia [14, 17]. Worldwide, however, it has been reported that insufficient numbers of SLP training programs provide pediatricspecific and adult-specific assessment and treatment training for graduate SLP students [18]. The need for high quality training in dysphagia assessment in particular has been voiced [19]. More commonly, students complete one dysphagia class that covers information across the lifespan, with little time spent on pediatric swallowing issues. Consequently, it has been reported that SLPs do not feel well-educated regarding assessment and treatment of these varied populations [20].
Materials and Methods
For example, a survey of 134 practicing SLPs reported a lack of pediatric dysphagia education during graduate school [21]. More recently, Knollhoff [22] analyzed SLP academic courses and found that less than 1% were categorized as pediatric swallowing and feeding. In addition, the author reported 90% of participants receive 20 hours or less of clinical experiences in pediatric dysphagia, assessment, or treatment, and 60% of participants queried did not feel well prepared to provide pediatric swallowing and feeding services. The emphasis on adult dysphagia has been shown to leave many graduates without the necessary skills and knowledge they need to address the specific needs of pediatric patients with dysphagia.
Thus, we know about a lack of education and training dedicated to pediatric dysphagia in most graduate SLP programs. What we do not know, however, is what is the impact, if any, that lack of programming focused on pediatric dysphagia has on the practice patterns of SLPs working with patients with pediatric dysphagia. Ultimately, we wanted to better understand practice patterns of SLPs working with adults and pediatric patients with dysphagia to inform future areas of focus in clinical training settings to ensure that best evidence-based practices are implemented in clinical practice. To do so, we deployed two comprehensive surveys to explore practice patterns of SLPs who provide assessment, diagnosis, and management of dysphagia in these two distinct age groups.
Materials and Methods
In this report, we combine the results of two anonymous surveys conducted to explore clinical practice patterns for speech-language pathologists (SLPs) providing services to adults or children with swallowing disorders. We compare and contrast findings of the two surveys.
Pediatric Survey
This study was approved by the Institutional Review Board at the University of Nebraska-Kearney and assigned IRB # 021223-1. The researchers designed a 15-question, anonymous Qualtrics/webbased survey pertaining to dysphagia assessment and management for pediatric populations. To support validation of the survey, it was field-tested with two experienced clinicians who commented about the content and structure of the survey, leading to some edits prior to distribution. Along with demographic information, the survey delved into questions about swallowing practices with children. On a five-point Likert scale, ranging from “never” to “always,” clinicians reported how often they address dysphagia across phrases of clinical interactions and how commonly they use several dysphagia assessment methods and management techniques to identify and treat swallowing difficulties in children. The survey questions can be seen in Appendix A.
Participants invited to complete the survey were SLPs providing clinical services to patients with pediatric dysphagia in the past three years. The survey link was included in an invitation distributed through professional contacts, social media posts, and the American Speech-Language-Hearing Association's Special Interest Group 13: Swallowing and Swallowing Disorders listserv.
Adult Survey
To identify the practice patterns of SLPs working with adult patients with dysphagia and to determine the types of assessments and treatments most frequently used, a similar 15-item anonymous survey was developed by the researchers. To support survey content validation, it was field tested with two experienced clinicians who provided comments about content and structure of the survey questions. Edits were made prior to distribution of the survey. The anonymous survey was approved as an exempt project by the Old Dominion University Human Subjects committee, IRB # 1847850- 1. Along with demographic information, the survey delved into questions about swallowing practices with adults. On a fivepoint Likert scale, ranging from “never” to “always,” clinicians reported how often they address dysphagia across phases of clinical interactions and their use of a variety of dysphagia assessment and management techniques. Areas investigated included the diagnostic techniques reported by SLPs, such as VFSS, FEES, and clinical swallowing evaluations. Information regarding the management of adult dysphagia was obtained by asking participants to identify commonly used therapeutic methods and strategies. This survey can be found in Appendix A.
Participants invited to complete the survey included SLPs providing clinical services to adult patients with dysphagia in the past three years. The survey link was included in an invitation distributed through professional contacts, listservs, social media posts, and ASHA's Special Interest Group 13: Swallowing and Swallowing Disorders.
Analysis
Data were imported from Qualtrics into SAS version 9.4 [23] (SAS Institute Inc., Cary, NC) for data management and analysis. Descriptive statistics (frequencies and percentages) were obtained for all study variables by survey type (i.e., adult vs. pediatric survey). Chi-square tests were used to compare the responses to parallel questions between the adult and pediatric surveys. A p-value < 0.05 was used to determine statistical significance.
Results
Participant Characteristics
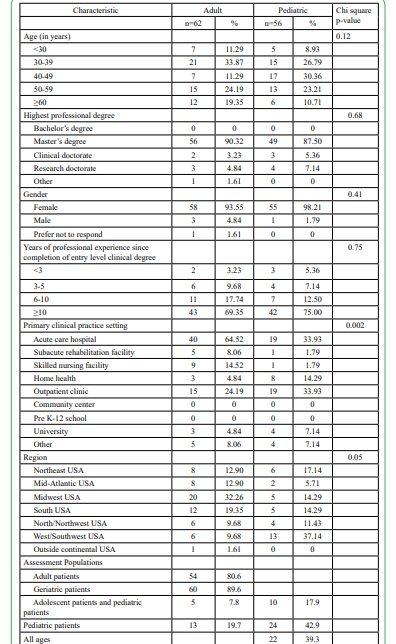
A total of 135 SLPs responded to the two surveys. Among them, 12 (8.9%) were excluded as they reported not providing clinical services to patients with dysphagia in their professional practice. Also, the adult survey had five respondents who only provided services to children and were excluded from the adult results. Therefore, the final analytic sample consisted of 118 participants. Among these, 62 (52.5%) answered the adult survey and 56 (47.5%) answered the pediatric survey. Responses to demographic survey questions are reported in Table 1.
Of the 118 who responded to the two surveys, most participants were female (adult: 93.6%; pediatric: 98.2%) and had a master’s degree (adult: 90.2%; pediatric: 87.5%). In terms of years of professional experience, the majority of participants in both surveys (adult: 69.4%; pediatric: 75%) reported having 10 years or greater since completion of their entry level clinical degree. Regarding practice locations, significantly more adult-based SLPs saw patients with dysphagia primarily at acute care hospitals (n= 40; 60.5%) while SLPs working with pediatric dysphagia patients worked in acute care hospitals (n =18; 19%) or outpatient clinics (n =18; 19%). The two survey groups significantly varied in the regions represented across the U.S. with approximately 1/3 of adult survey participants from the midwestern U.S. (32.2%), and 1/3 of pediatric survey participants from the west/southwestern U.S. (37.5%).
When Dysphagia Is Addressed
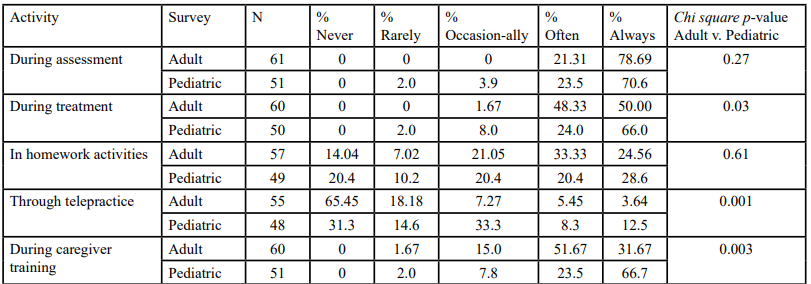
Table 2 shows SLP responses to how often they address dysphagia in the different phases of clinical practice. Some respondents did not answer these items. Significant differences were noted in some patterns reported between the adult and pediatric survey groups. The majority of clinicians in the adult and pediatric surveys reported that they “often” or “always” assess dysphagia in their patients, with no difference between groups. Again, a large majority “often” or “always” address dysphagia in treatment, although the pattern differed between groups. Significantly more pediatric survey respondents responded “always” than adult survey respondents (p<0.03). When queried about homework to address dysphagia symptoms, responses for adult and pediatric clinicians were evenly distributed from “never” to “always”, with no difference between groups. The use of telepractice for dysphagia varied significantly between the adult and pediatric survey clinicians (0.001). A majority of adult clinicians “never” address dysphagia through telepractice, while more pediatric clinicians reported at least “occasionally” working with dysphagia through telepractice. Finally, in caregiver training more adult survey SLPs “often” address dysphagia whereas more child survey SLPs “always” work with caregivers (p<0.003).
Assessment Populations
As indicated in Table 1, SLPs who responded to the adult dysphagia survey reported they most often assessed adult (n = 54, 80.6%) and geriatric (n = 60; 89.6%) patients. There were 13 (19.7%) participants in the adult dysphagia survey who reported also assessing and treating pediatric patients and five (7.8%) treated adolescent patients.
In the pediatric survey, 24 (42.9%) participants addressed only pediatric patients; 10 (17.9%) addressed pediatric and adolescent patients; and 22 (39.3%) reported working with pediatric, adolescent, adult, and geriatric patients with dysphagia.
Session Length
Table 3 displays typical length of dysphagia assessment sessions for the two surveys. Overall, session lengths for dysphagia assessment for pediatric survey SLPs were significantly different than adult survey SLPs (p<0.008). Respondents to the pediatric survey most commonly reported 46–60-minute dysphagia sessions (41.2%), while adult survey respondents most commonly reported 16-30 minute sessions (39.4%). In the adult survey, 13.6% of respondents reported spending only 10 to 15 minutes for dysphagia assessment compared to only 2% of the participants in the pediatric dysphagia survey.
Assessment Tools
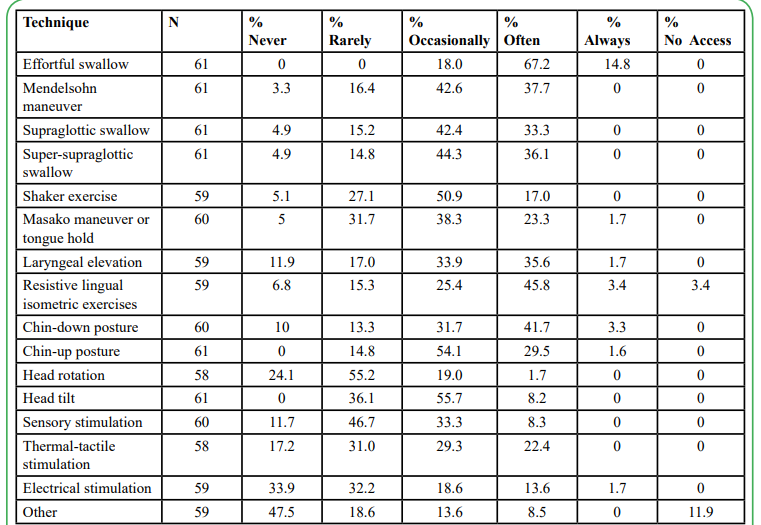
Table 4 illustrates several tools used when assessing pediatric and adult patients with suspected swallowing disorders. Survey respondents reported how frequently they used each tool, with p-values for comparisons of responses between adult and pediatric SLPs. The most used assessment tool in both groups was the clinical swallowing exam, as a large majority responded with “always” or “often”, and no significant difference was evident in response pattern between groups.
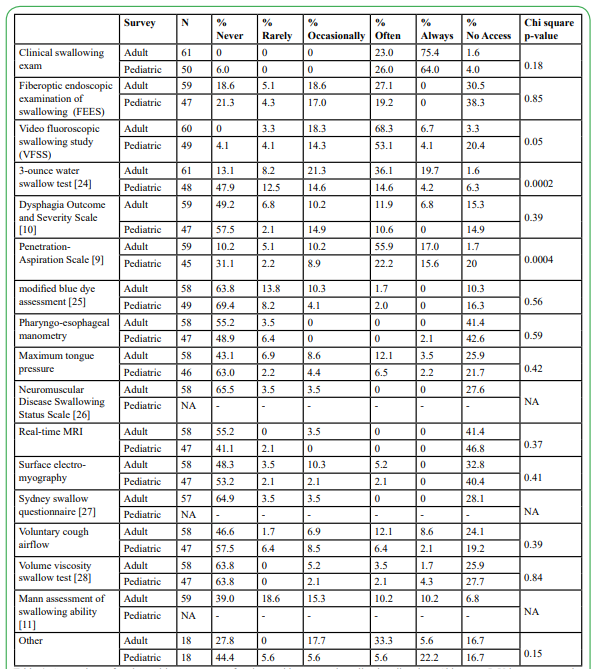
Table 4: Comparison of tools used in assessment of patients with suspected swallowing disorders; Chi square P-Values compare the adult and pediatric survey responses
The most used tool was the instrumental exam VFSS, reported “often” by the majority of adult and pediatric survey respondents. A significant group difference evident for the groups on the VFSS appears to be driven by many (20.4%) of the pediatric respondents indicating “no access” to VFSS. Much less commonly used as an instrumental technique is the FEES, as approximately 50% of each group reported “no access” or “never” using the technique. Significant differences between the two survey groups were evident for the use of the 3-ounce water swallow test [24] and the PenetrationAspiration Scale [9]. Both tools were significantly more likely to be used “often” or “always” in adult patients than pediatric patients.
Rarely used by either adults or pediatric SLPs working with patients with dysphagia included the modified blue dye assessment [25], pharyngo-esophageal manometry, maximum tongue pressure, Neuromuscular Disease Swallowing Status Scale [26], real-time MRI, surface electromyography, Sydney Swallow Questionnaire [27], voluntary cough airflow, Volume Viscosity Swallow Test [28], and Assessment of Swallowing Ability [11].
At least one-quarter of adult study participants did not have access to the following assessment tools: FEES, pharyngoesophageal manometry, maximum tongue pressure, Neuromuscular Disease Swallowing Status Scale [26], real-time MRI, surface electromyography, and Volume Viscosity Swallow Test [28].
Treatment Techniques
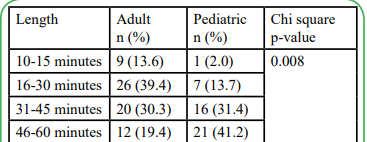
Treatment techniques typically used with adult and pediatric populations vary considerably. Results of questions pertaining to use of dysphagia intervention techniques are displayed in Table 5 for the adult survey and Table 6 for the pediatric survey. The most commonly used technique reportedly used for treating adult swallowing disorders was the effortful swallow as more than 80% “often” or “always” use the technique. The next most common techniques used in adults reported by >40% of respondents were resistive lingual isometric exercises and chin-down posture. More than 50% of respondents “rarely” or “occasionally” use Mendelsohn maneuver, supraglottic swallow, super-supraglottic swallow, Shaker exercise, Masako maneuver, laryngeal elevation, chin-up posture, head rotation, head tilt, sensory stimulation, thermal-tactile stimulation, and electrical stimulation. A considerable number of respondents reported “never” using head rotation (24.1%) and electrical stimulation (33.9%).
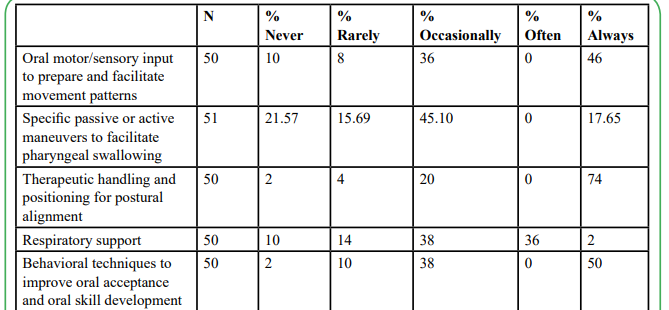
Turning to the pediatric swallowing survey results in Table 6, the most commonly used intervention techniques were therapeutic handling and positioning (“always” 74%), behavioral techniques to improve oral acceptance and skill development (“always” 50%) and oral motor/sensory input to facilitate movement patterns (“always” 46%). “Occasionally” used were specific passive or active maneuvers (45.1%) and respiratory support (38%). A considerable number of respondents “never” (21.6%) use maneuvers, however.
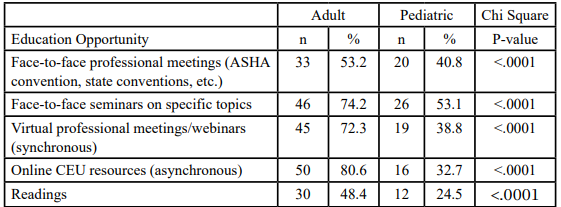
Continuing Education
Finally, both surveys ended with a question about the preferred methods for accessing continuing education pertaining to dysphagia (Table 7). Adult and pediatric SLP respondents endorsed all listed platforms for accessing continuing education opportunities. Respondents to the adult survey were significantly more likely to prefer each type of education opportunity listed than respondents to the pediatric survey. Online CEU resources were the most highly preferred platform for adults (80.6%), followed closely by face-toface seminars (74.2%) and virtual professional meetings/webinars (72.3%). Each of these far surpassed the numbers endorsed by the pediatric survey participants who preferred face-to-face seminars (53.1%), face-to-face professional meetings (40.8%) and virtual professional meetings/webinars (38.8%).
Discussion
Pediatric and adult dysphagia encompass a wide range of swallowing disorders that can arise from various etiologies, including neurological, structural, and developmental conditions. The complexity of these disorders requires SLPs to have a thorough understanding of the anatomy and physiology of swallowing, as well as the ability to perform detailed assessments and develop tailored intervention plans. The manifestations of dysphagia in children can vary widely, from difficulties with sucking and swallowing in infants to challenges with chewing and managing different food textures in older children. This variability necessitates a nuanced approach to diagnosis and treatment, which can be particularly challenging for inadequately trained SLPs [22]. Likewise, dysphagia assessment and management are complex and demanding of clinical decisionmaking for adult patients as well. Thus, a considerable body of knowledge is expected of new clinicians entering clinical practice to address the possible dysphagia manifestations across the lifespan. Yet, evidence suggests that training tends to be focused on adult dysphagia moreso than pediatric dysphagia. Research indicates that many SLPs feel underprepared to manage pediatric dysphagia effectively [21]. Most SLP graduate programs offer only a cursory overview of pediatric dysphagia, with limited hands-on clinical experience. While continuing education courses are available, they are often not mandatory, and many practicing SLPs may not have the time or resources to pursue these opportunities. While there are beneficial online courses, such as those focused on pediatric dysphagia and medically-based feeding disorders, many SLPs may only feel comfortable with live, hands-on training and workshops.
The results of our two surveys of clinicians providing services for dysphagia populations give insights on professional practice to inform the content of graduate dysphagia courses. Although many evidence-based practices have been developed and described in the clinical literature, clinicians in our surveys tend to use a more circumscribed set of tools and techniques for assessment and management of swallowing disorders. We propose that those options need considerable emphasis in preservice graduate coursework and clinical training for new SLPs to enter clinical practice with essential knowledge and skills for addressing dysphagia across the lifespan. Our surveys indicated that several other tools and techniques are much less commonly used clinically. While students need to be introduced to most of those options, clinicians in specialized settings will want to expand their expertise on the variety of tools and techniques available for swallowing management through in-service continuing education options.
With respect to dysphagia assessment, not surprisingly, noninstrumental clinical swallowing evaluations and instrumental VFSS are the most commonly used tools in clinical practice for both adults and children. This observation suggests that preservice graduate educational training activities should center on instruction, simulations, and hands-on experiences to advance skills particularly for those two methods, including information for adults and children. Other assessment tools are reportedly used less frequently in clinical practice (e.g., FEES, Penetration-Aspiration Scale [9], 3-ounce water swallow [24], Mann Assessment of Swallowing Ability [11]), whether for lack of availability or lack of familiarity. Exposure to some tools developed particularly with pediatric populations in mind, such as the Sydney Swallow Questionnaire [27], would expand clinical options that are relevant to children. Regardless, the survey findings suggest that, while students should be introduced to some of the other assessment options during preservice clinical preparation, less direct instruction would be warranted with the limited class time available. Given limited time and resources, those who need specialized dysphagia knowledge and skills for their clinical practice setting would require additional training outside of graduate school courses in the form of hands-on continuing education coursework.
Considering swallowing intervention, several techniques have been described to directly address skills necessary for oral feeding and swallowing or to compensate for an impaired swallowing system. Surprisingly, based on our survey results, a limited number of these techniques were reported to be used often in clinical practice. Therefore, we suggest that graduate coursework focus education and training on the most frequently used techniques and strategies. The strategy of implementing an effortful swallow is most commonly attempted in adults as are lingual isometric exercises. Much less often used techniques for adults are ones to protect or circumvent the impaired swallow or sensory techniques to rehabilitate the swallow. In pediatric interventions, most commonly used are therapeutic handling and postural positioning as well as techniques to improve oral acceptance and skill development. Again, these observations suggest directions for the most essential pre-service learning for dysphagia content and skills. Those clinicians in settings where dysphagia intervention is common will want to explore continuing education training for the variety of techniques available to expand their practice repertoire. Interestingly, clinicians responding to the pediatric survey were less likely to endorse any number of potential professional development avenues, which are likely to be so necessary in the pediatric dysphagia realm.
Lastly, of significant note is that the SLPs in these surveys reported much cross-coverage for pediatric and adult services. Of the SLPs who responded to the pediatric survey, nearly 40% (n = 22, 39.3%) reported to assess and treat patients of all ages on their caseloads. Of the SLPs who responded to the adult survey, nearly 20% (n = 13, 19.7%) indicated they also had pediatric patients and five (7.8%) also saw adolescent patients for swallowing disorders. These findings have implications for the importance of expanding preservice training to address both adult and pediatric populations. This type of caseload requires a broad and dynamic skill set, ongoing professional development, effective resource management, and the ability to navigate complex emotional and ethical landscapes. However, the diverse clinical knowledge and skills involving assessment tools and techniques, treatment approaches, communication approaches, emotional and psychological considerations, logistical challenges, and continuing education and professional development remain far from the forefront of dysphagia swallowing assessment and treatment education in graduate school. Until these aspects are addressed during graduate training, many SLPs may struggle to balance crucial factors imperative in providing comprehensive and effective dysphagia care across the lifespan.
Other observations of our surveys also have implications for preservice training. When queried about use of homework for dysphagia management, some clinicians always assign homework. Likewise, many clinicians now report the frequent use of telepractice, moreso for children than for adults, for dysphagia management. These findings suggest the importance of incorporating these types of activities in preservice education and clinical training activities for dysphagia so students are prepared for the necessities of clinical practice.
Limitations
Although we attempted to conduct a comprehensive survey to gain a sense of common dysphagia practice patterns for adult and pediatric populations, we recognize that our methods and findings are not without limitations. One significant limitation to this study relates to the participant groups. Given the large numbers of SLPs providing clinical services for dysphagia, the respondent samples were rather small. The survey process leads to self-selection of the population and limits the expanse of the study and ultimately its generalizability and is subject to response bias. The findings of these two surveys occurred at singular points in time, which limits significance over time. A longitudinal study would prove beneficial to support or reject the findings reported here. Further, a qualitative examination of SLPs providing dysphagia services may provide insights into why some of these response patterns were evident.
Many respondents selected “other” as a response to the questions about dysphagia assessment and intervention, and we do not know what those other options might have been. The assessment tools and treatment techniques described for dysphagia are continually expanding and evolving and respondents may have been familiar with items that were not listed in our survey. For example, we neglected to include two rating scales that clinicians may be using in clinical practice (i.e., EAT-10 [29] and PEDI-EAT-10 [30]). Likewise, some of our other work suggests that clinicians often use informal or non-standardized methods for assessment and treatment that are not evidence-based [31], a likely scenario in this survey as well. Finally, we noted that our respondents represented a rather experienced group, having graduated from training programs many years earlier. Therefore, their response patterns may not represent patterns of professional practice that might be seen in clinicians who more recently exited academic training where advances may have taken place in expanding dysphagia knowledge and skills in both adult and pediatric populations.
Future Directions
Specialized training programs and fellowships can significantly enhance the competencies of SLPs in managing pediatric dysphagia. Programs such as the Pediatric Dysphagia Speech Pathology Fellowship at Nationwide Children's Hospital provide extensive clinical and research training, equipping SLPs with the skills necessary to deliver high-quality care [31]. Such training experiences emphasize practical, hands-on activities and the application of evidence-based practices, which are essential for effective intervention. Incorporating case studies and practical applications into training programs can bridge the gap between theory and practice. Courses that offer video examples, guided self-study modules, and detailed analysis of reallife cases have been shown to improve the practical skills of SLPs [32-34]. These elements help clinicians understand the nuances of pediatric dysphagia, from initial assessment to the development of comprehensive treatment plans.
Professional organizations such as the American Speech-LanguageHearing Association (ASHA) play a crucial role in advocating for better training standards. ASHA's endorsement of specialized training programs and its provision of continuing education credits can encourage more SLPs to pursue advanced training in dysphagia with additional focus on pediatric dysphagia. Additionally, professional bodies can facilitate the development of standardized curricula that ensure all graduate programs adequately cover feeding and swallowing disorders across the lifespan for infants to elderly.
Conclusion
SLPs who specialize in pediatric swallowing disorders and those who focus on adult swallowing disorders play critical roles addressing the unique needs and challenges presented by their respective patient populations. While they share common foundational knowledge and skills, there are significant differences between these two specialized areas of practice.
Throughout these surveys, a comparative analysis identified similarities and differences in the assessment and management of dysphagia in pediatric and adult patients. By shedding light on these distinctions, we aim to foster a greater understanding of the challenges and opportunities in the field of dysphagia management across different age groups. The findings presented in this survey contribute valuable insights for healthcare professionals, researchers, and practitioners working to enhance the quality of life for individuals living with dysphagia, whether they be children or adults. But above all, it sheds light on the critical need to provide specific and hands-on preservice and in-service training for SLPs working with dysphagia patients, including those with pediatric dysphagia.
Even though principles of dysphagia assessment and treatment apply across the lifespan, the unique characteristics and needs of adults and children necessitate different skills, approaches, and considerations in the management of swallowing disorders. Specialized training and expertise are essential for SLPs working with each population to provide effective and age-appropriate care.
The need for better training of SLPs in pediatric dysphagia is evidenced by the training that SLPs seek after graduation to augment their education. In addition, as the participants in this survey who work with pediatric patients with swallowing disorders indicated a preference for face-to-face trainings, the importance of hands-on experiences must be considered for future clinicians. Addressing this gap requires a multifaceted approach that includes enhancing graduate program curricula, increasing access to specialized training programs and continuing education, and advocating for higher training standards through professional organizations. By investing in comprehensive, hands-on training during graduate school programming, we can ensure that SLPs are well-equipped to provide the highest standard of care in professional practice.
Competing Interests
The authors declare that they have no competing interests.
List of Abbreviations
SLPs: Speech-Language Pathologists VFSS: videofluoroscopic swallowing study FEES: fiberoptic endoscopic evaluation of swallowing
Acknowledgments
Data collection and preliminary analysis were sponsored by undergraduate research grants from Old Dominion University for Kaitlyn Hill (adult dysphagia survey), and through Nebraska’s EPSCoR undergraduate research grant for Marlee Nebesniak (pediatric dysphagia survey). Portions of these findings were presented at annual meetings of the Speech and Hearing Association of Virginia, the Nebraska Speech-Language Hearing Association, Student Research Days at Old Dominion University and the University of Nebraska-Kearney, and the American Speech-Language Hearing Association annual convention. We have no conflicts of interest to disclose.
References
Panebianco, M., Marchese-Ragona, R., Masiero, S., & Restivo, D.A. (2020). Dysphagia in neurological diseases: A literature review. Neurological Sciences, 41(11), 3067–3073. View
Hong, I., Bae, S., Lee, H.K., & Bonilha, H.S. (2024). Prevalence of dysphonia and dysphagia among adults in the United States in 2012 and 2022. American Journal of Speech-Language Pathology, 33(40), 1868-1879. View
Bhattacharyya, N. (2020). The prevalence of pediatric voice and swallowing problems in the United States. Laryngoscope, 125(3), 746–750. View
Lawlor, C.M., & Choi, S. (2020). Diagnosis and management of pediatric dysphagia: A review. JAMA Otolaryngology-Head & Neck Surgery, 146(2), 183–191.View
Ciucci, M.R., Johnes, C.A., Malandraki, G.A., & Hutcheson, K.A. (2016). Dysphagia practice in 2035: Beyond fluorography, thickener, and electrical stimulation. Seminars in Speech & Language, 37(3), 201–208. View
Heckathorn, D.-E., Speyer, R., Taylor, J., & Cordier, R. (2016). Systematic review: Non-instrumental swallowing and feeding assessments in pediatrics. Dysphagia, 31(1), 1–23. View
Miller, C.K., Schroeder, J.W., & Langmore, S. (2020). Fiberoptic endoscopic evaluation of swallowing across the age spectrum. American Journal of Speech-Language Pathology, 29(2S), 967–978. View
Pizzorni, N., Rocca, S., Eplite, A., Monticelli, M., Rama, S., Mozzanica, F., et al. (2024). Fiberoptic endoscopic evaluation of swallowing (FEES) in pediatrics: A systematic review. International Journal of Pediatric Otorhinolaryngology, 181:11983. View
Rosenbek, J.C., Robbins, J.A., Roecker, E.B., Coyle, J.L., & Wood, J.L. (1996). A penetration-aspiration scale. Dysphagia, 11(2), 93–98. View
O’Neil, K.H., Purdy, M., Falk, J., & Gallo, L. (1999). The dysphagia outcome and severity scale. Dysphagia, 14(3), 139– 145. View
Mann, G. (2002). MASA: The Mann Assessment of Swallowing Ability. Clifton Park, NY: Thomson Learning.
Shune, S.E., Linville, D., & Namasivayam-MacDonald, A. (2022). Integrating family-centered care into chronic dysphagia management: A tutorial. Perspectives of the ASHA Special Interest Groups, 7(3), 795–806. View
Simione, M., Dartley, A.M., Cooper-Vince, C., Martin, V., Hartnick, C., Taveras, E.M., et al. Family-centered outcomes that matter most to parents: A pediatric feeding disorders qualitative study. Journal of Pediatric Gastroenterology and Nutrition, 71(2), 270–275. View
Lefton-Grief, M.A., & Arvedson, J.C. (2016). Pediatric feeding/swallowing: Yesterday, today, and tomorrow. Seminars in Speech & Language, 37(4), 298–309. View
. Chandran, S.K., & Doucet, M. (2024). Neurogenic dysphagia. Otolaryngology Clinics of North America, 57(4), 589–597. View
. Cosentino, G., Todisco, M., Giudice, C., Tassorelli, C., & Alfonsi, E. (2022). Assessment and treatment of neurogenic dysphagia in stroke and Parkinson’s disease. Current Opinion in Neurology, 35(6), 741–752. View
. Rogus-Pulia, N.M., & Plowman, E.K. (2020). Shifting tides toward a proactive patient-centered approach in dysphagia management of neurodegenerative disease. American Journal of Speech-Language Pathology, 29(2S), 1094–1109. View
. Kamal, R.M., Ward, E., & Cornwell, P. (2012). Dysphagia training for speech-language pathologists: Implications for clinical practice. International Journal of Speech-Language Pathology, 14(6), 569–76. View
Speyer, R., Cordier, R., Farneti, D., Nascimentao, W., Pilz, W., Verin, E., et al. (2021). White paper by the European Society for Swallowing Disorders: Screening and non-instrumental assessment for dysphagia in adults. Dysphagia, 37(4), 333–349. View
Caesar, L.G., & Kitila, M. (2020). Speech-language pathologists' perceptions of their preparation and confidence for providing dysphagia services. Perspectives of the ASHA Special Interest Groups, 5(6), 1666–1682. View
Wilson, J.J., Simmons, A.K., & McCarthy, J.H. (2020). Pediatric dysphagia: Survey results describing speech-language pathologists' education and experience. Perspectives of the ASHA Special Interest Groups, 5(1), 236–245. View
Knollhoff, S.M. (2023). Pediatric dysphagia: A look into the training received during graduate speech-language pathology programs to support this population. Language, Speech, and Hearing Services in Schools, 54(2), 425–435. View
SAS. (2013). Statistical Analysis Software. Users' Guide Statistics Version 9.4. Cary: SAS Institute Inc.
DePippo, K.L., Holas, M.A., & Reding, M.J. (1992). Validation of the 3-oz water swallow test for aspiration following stroke. Archives of Neurology, 49(12):1259–61. View
Thompson-Henry, S., & Braddock, B. (1995). The modified Evan’s blue dye procedure fails to detect aspiration in the tracheotomized patient: Five case reports. Dysphagia, 10(3), 172–175. View
Wada, A., Kawakami, M., Liu, M., Otaka, E., Nichimura, A., Liu, F., et al. (2015). Development of a new scale for dysphagia in patients with progressive neuromuscular diseases: The Neuromuscular Disease Swallowing Status Scale (NdSSS). Journal of Neurology, 262(10), 2225–2231. View
Wallace, K.L., Middleton, S., & Cook, I.J. (2000). Development and validation of a self-report symptom inventory to assess the severity of oral-pharyngeal dysphagia. Gastroenterology, 118(4), 678–687. View
Clavé, P., Arreola, V., Romea, M., Medina, L., Palomera, E., & Serra-Prat, M. (2008). Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clinical Nutrition, 27(6), 806–815. View
Belafsky, P.D., Mouadeb, D.B., Rees, C.J., Pryer, J.C., Postma, G.N., Allen, J., & Leonard, R.J. (2008). Validity and reliability of the Eating Assessment Tool (EAT-10). Annals of Otology, Rhinology, and Laryngology, 117(2), 919-924. View
Arslan, S.S., Demir, N., Karaduman, A., & Belafsky, P.C. (2018). The pediatric version of the Eating Assessment Tool: A caregiver administered dysphagia-specific outcome instrument for children. Disability and Rehabilitation, 40(17), 2088-2092. View
Roitsch, J., Prebor, J., & Raymer, A.M. (2021). Cognitive assessments for patients with neurological conditions: A preliminary survey of speech-language pathology practice patterns. American Journal of Speech-Language Pathology, 30(5), 2263–2274. View
Nationwide Children's Hospital. Pediatric Dysphagia Speech Pathology Fellowship [Internet]. 2023 [cited 2025 Apr 3]. Available from: View
Northern Speech Services. Pediatric Dysphagia and Medically Based Feeding Disorders [Internet]. 2021 [cited 2025 Apr 3]. Available from: View
Northern Speech Services. Pediatric Dysphagia Assessment and Treatment [Internet]. 2023 [cited 2025 Apr 3]. View
Tubes2 Tables. Preterm infant feeding and swallowing laboratory [Internet]. 2024 [cited 2025 Apr 3]. Available from: View