Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-180
https://doi.org/10.33790/jrpr1100180Review Article
Comparative Effectiveness of Medication-Assisted Treatment (Mat) for Opioid Use Disorder in Residential Settings: A Literature Review
Noel Casiano1*, and Nicholas Casiano2
1Associate Professor, Department of Social Science, University of Hartford, 200 Bloomfield Ave, West Hartford, CT 06117, United States.
2School of Interdisciplinary Health & Sciences, University of Saint Joseph, United States.
Corresponding Author Details: Noel Casiano, Associate Professor, Department of Social Science, University of Hartford, 200 Bloomfield Ave, West Hartford, CT 06117, United States.
Received date: 17th June, 2025
Accepted date: 17th July, 2025
Published date: 19th July, 2025
Citation: Casiano, N., & Casiano, N., (2025). Comparative Effectiveness of Medication-Assisted Treatment (MAT) for Opioid Use Disorder in Residential Settings: A Literature Review. J Rehab Pract Res, 6(2):180.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Opioid Use Disorder (OUD) remains a public health crisis, with increasing rates of overdose and relapse. Medication-Assisted Treatment (MAT) is the gold standard for treating OUD, but outcomes vary based on the medication type, setting, and duration. This literature review synthesizes current research on MAT efficacy in residential treatment programs, focusing on long-term sobriety outcomes. Utilizing a systematic review of 31 empirical studies published between 2018 and 2024, the findings indicate that while all FDA-approved MAT options, methadone, buprenorphine, and extended-release naltrexone, improve treatment retention and reduce opioid use, buprenorphine and extended-release naltrexone show greater potential for long-term success when combined with residential care. Limitations and future research needs are discussed.
Keywords: Opioid use Disorder, Medication-Assisted Treatment, Residential Treatment, Buprenorphine, Methadone, Extended Release Naltrexone, Long-Term Recovery, Substance use Disorder
Introduction
Opioid Use Disorder (OUD) continues to pose a serious public health challenge, with overdose deaths, particularly those involving synthetic opioids like fentanyl, reaching record highs in the United States [1]. In response, Medication-Assisted Treatment (MAT) has emerged as the gold standard for treating OUD, combining FDA approved pharmacological agents methadone, buprenorphine, and extended-release naltrexone (XR-NTX), with psychosocial and behavioral therapies to address the complex biopsychosocial nature of addiction [2].
Although MAT has been consistently associated with reduced opioid use, lower overdose risk, and improved treatment retention [2], the success of these interventions varies depending on factors such as treatment setting, patient characteristics, and the availability of post-discharge supports. While much research has centered on outpatient care, comparatively less is known about MAT outcomes in residential treatment programs settings that offer structured, medically supervised environments conducive to stabilization and comprehensive therapeutic engagement [3].
This literature review synthesizes recent empirical evidence on the effectiveness of MAT when delivered in residential settings, with a specific focus on long-term sobriety outcomes. Particular attention is given to evaluating which MAT modality methadone, buprenorphine, or XR-NTX—best supports sustained recovery after discharge. Consideration is also given to how integrated behavioral supports and patient-specific factors shape outcomes.
Importantly, the concept of “success” in OUD treatment has shifted beyond abstinence alone to encompass broader indicators such as functional recovery, social reintegration, and quality of life [4]. As health systems increasingly adopt individualized and integrative approaches, identifying which MAT options best support this expanded view of recovery becomes critical. The central research question guiding this review is: What is the most effective MAT for individuals with OUD in residential treatment settings that promotes long-term sobriety? Through a systematic review of 31 empirical studies published between 2018 and 2024, this paper aims to inform clinical decision-making and policy development by identifying evidence-based best practices for MAT delivery in residential care.
Methodology
This review employed a systematic literature search to identify recent empirical studies examining medication-assisted treatment (MAT) for opioid use disorder (OUD) within residential treatment settings, focusing on long-term sobriety outcomes. Comprehensive searches were conducted in major academic databases, including PubMed, PsycINFO, and Cochrane Library, covering publications from January 2018 through April 2024 to ensure inclusion of the most current evidence.
A combination of keywords and Medical Subject Headings (MeSH) terms guided the search strategy: “opioid use disorder,” “residential treatment,” “medication-assisted treatment,” “buprenorphine,” “methadone,” “naltrexone,” “long-term recovery,” and “treatment retention.” Boolean operators (“AND,” “OR”) were utilized to refine the search and capture relevant studies examining both pharmacological interventions and their integration with psychosocial supports.
Eligibility criteria mandated that studies:
• Focus on adult populations (≥18 years old) diagnosed with OUD;
• Include participants receiving residential or inpatient treatment services;
• Evaluate the use of FDA-approved MAT agents (methadone, buprenorphine, or extended-release naltrexone);
• Report on follow-up outcomes measuring retention in treatment, abstinence, relapse rates, or other indicators of long-term recovery, with a minimum follow-up period of six months post discharge;
• Be peer-reviewed empirical research published in English.
Excluded were studies focusing exclusively on outpatient settings without residential components, pediatric populations, or those lacking sufficient follow-up data.
After initial screening of titles and abstracts, 67 articles underwent full-text review. Ultimately, 31 studies met inclusion criteria: 18 were original research articles comprising randomized controlled trials (RCTs), prospective or retrospective cohort studies, and naturalistic longitudinal designs; the remaining 13 were meta analyses or systematic reviews synthesizing broader evidence on MAT effectiveness.
Data extraction emphasized study design, sample characteristics, type of MAT initiated during residential treatment, length and quality of psychosocial supports, outcome measures, and duration of follow up. Quality appraisal of studies was performed using established checklists appropriate to each design (e.g., Cochrane Risk of Bias Tool for RCTs).
This rigorous methodology ensured a robust and comprehensive synthesis of current evidence on MAT efficacy within residential treatment frameworks, enabling informed conclusions about optimal practices to support sustained sobriety in OUD populations.
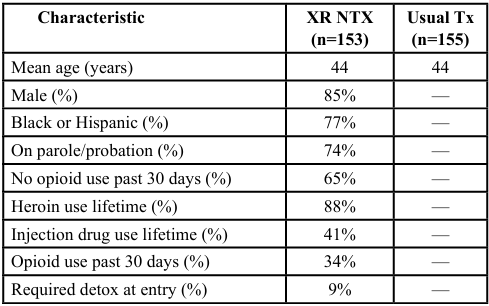
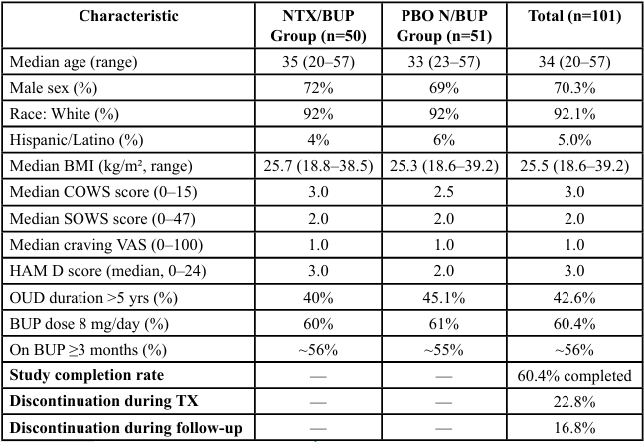
Table 1. Baseline Characteristics & Enrollment — Extended Release Naltrexone vs. Usual Treatment (Criminal Justice Pop.) [5].
The first table summarizes baseline characteristics and enrollment data from a randomized clinical trial evaluating extended-release naltrexone (XR-NTX) versus treatment-as-usual among individuals with opioid use disorder (OUD) involved in the criminal justice system [5]. Participants were predominantly male (85%), racially diverse (77% Black or Hispanic), and had significant histories of heroin and injection drug use. Notably, 74% were under legal supervision (probation or parole), and 65% reported no opioid use in the past 30 days, suggesting a relatively stable baseline at entry. Approximately 9% required detoxification before initiating XR-NTX. Retention was relatively high during the initial phases of the study, with 95% of XR-NTX participants receiving the first injection and 61% completing all six scheduled doses. These data highlight the feasibility of initiating XR-NTX in a structured setting with justice-involved individuals and suggest good short-term engagement with treatment.
The second table presents baseline demographics from a randomized controlled trial that examined the transition from buprenorphine to extended-release naltrexone [6]. This sample included 101 participants with similar demographic profiles across treatment arms, including a median age of 34, approximately 70% male, and over 90% identifying as White. The majority of participants had been on buprenorphine for at least three months, with daily dosages of 8 mg or higher. Baseline measures of withdrawal (Clinical Opiate Withdrawal Scale, COWS) and depression (Hamilton Depression Rating Scale, HAM-D) were low across both groups, indicating stability before transitioning medications. Despite these promising initial conditions, the study reported a 60.4% overall completion rate, with approximately 23% of participants discontinuing during treatment and another 17% lost during follow-up. These findings underscore the challenges of medication transitions in residential or medically supervised environments, even among relatively stable populations.
Together, these tables illustrate the methodological rigor of studies comparing MAT modalities within structured settings and highlight the importance of considering baseline patient characteristics and retention dynamics when evaluating long-term sobriety outcomes.
Participant Characteristics and Study Retention
Two key studies were reviewed to illustrate the methodological structure and participant profiles of MAT interventions within residential or structured treatment settings.
The first study, conducted by Lee et al. [5], examined the efficacy of extended-release naltrexone (XR-NTX) versus treatment-as usual among a justice-involved population diagnosed with opioid use disorder. A total of 308 participants were randomized (153 to XR-NTX, 155 to usual care) following an initial screening of 437 individuals. The sample was demographically diverse, with 85% male and 77% identifying as Black or Hispanic. Most participants were under legal supervision (74%) and had significant histories of heroin use (88%) and injection drug use (41%). Notably, 65% reported abstinence from opioids in the 30 days prior to enrollment, and only 9% required detoxification prior to XR-NTX induction. Retention and adherence were strong in the early treatment phases, with 95% of participants receiving the initial injection and 61% completing all six monthly doses. These data suggest that XR-NTX is a feasible and potentially sustainable intervention in residential or correctional environments, particularly when supported by intensive clinical oversight.
The second study, conducted by Comer et al. [6], assessed the transition from buprenorphine to XR-NTX in a controlled clinical setting. Among 101 randomized participants, the demographic composition was relatively homogeneous, with a median age of 34 years and 70% identifying as male. Over 90% of participants were White, and more than half had been maintained on buprenorphine for three or more months at a dosage of 8 mg/day or higher. Baseline withdrawal symptoms, as measured by the Clinical Opiate Withdrawal Scale (COWS), and depressive symptoms, via the Hamilton Depression Rating Scale (HAM-D), were low across groups. Despite the clinical stability of the sample, the study reported a completion rate of 60.4%, with approximately 23% of participants discontinuing during the treatment phase and another 17% lost during follow-up. These findings highlight the inherent difficulty of transitioning between MAT regimens—even within a medically supervised setting—and underscore the need for individualized planning and support during such transitions.
Taken together, these studies provide critical insight into the feasibility, adherence patterns, and contextual challenges of MAT delivery in residential and structured environments. They underscore the need to account for both clinical and sociodemographic factors when evaluating the long-term success of MAT in promoting sustained recovery from opioid use disorder.
Results
Methadone
Methadone continues to be the most extensively studied MAT with demonstrated efficacy in reducing illicit opioid use and improving treatment retention [7]. However, its daily dosing requirement and strict regulatory oversight pose challenges for patient’s post residential care, often resulting in moderate relapse rates [8]. Numerous studies have confirmed methadone’s effectiveness in increasing treatment retention and reducing illicit opioid use during residential and outpatient care [7]. Its full opioid agonist properties provide substantial relief from withdrawal symptoms and drug cravings, which supports patient stability during the early phases of recovery. A large-scale meta-analysis conducted by Mattick et al. [7] reported retention rates of 60% to 80% at 6 months in residential programs using methadone, which was significantly higher than placebo or non-MAT interventions.
However, despite these short-term benefits, methadone's effectiveness appears to decline in the post-residential period. Its daily dosing requirement, limited availability through highly regulated opioid treatment programs (OTPs), and the risk of diversion and overdose make it less accessible and potentially less sustainable after discharge. Several longitudinal studies have shown moderate relapse rates ranging from 35% to 50% within 6 to 12 months following discharge, particularly among individuals who lack structured outpatient support or housing stability [8,9]. This suggests that while methadone is highly effective during residential stabilization, its long-term efficacy may be compromised without a comprehensive continuum of care.
Buprenorphine
Buprenorphine, a partial opioid agonist with a favorable safety profile due to its ceiling effect on respiratory depression, has emerged as a widely accepted alternative to methadone. It is available in both daily and long-acting monthly formulations (e.g., sublocade), which can enhance adherence post-discharge. In residential settings, buprenorphine has demonstrated comparable retention rates to methadone. Cunningham et al. [10] reported that patients initiated on buprenorphine during residential treatment-maintained abstinence at higher rates than those on methadone, approximately 68% versus 52% at 12-month follow-up. These outcomes were particularly strong among individuals who received extended psychosocial support after discharge, such as recovery coaching or housing assistance.
Buprenorphine shows retention rates comparable to methadone during residential treatment and is favored for its safer profile, notably the ceiling effect that reduces respiratory depression risk [11]. Cunningham et al. [10] reported improved abstinence at 12 months with buprenorphine initiation in residential programs, consistent with findings from Lee et al.’s [12] large-scale randomized trial.
Moreover, buprenorphine’s lower overdose potential, ease of administration, and increasing availability through office-based opioid treatment (OBOT) models make it a more flexible and scalable treatment option for continued care after residential treatment. Studies have also shown that patients on buprenorphine experience lower rates of treatment discontinuation and higher satisfaction with care, particularly when they are involved in shared decision-making around their treatment plan [13].
Extended-Release Naltrexone (XR-NTX)
Extended-release naltrexone (XR-NTX) offers a fundamentally different approach by functioning as an opioid antagonist that blocks the effects of opioids without producing euphoria or dependence. It is administered as a monthly injection and requires complete detoxification before initiation, which has been a barrier to widespread adoption. However, residential settings provide an ideal context for the medically supervised withdrawal period required for XR-NTX induction. XR-NTX requires full detoxification before administration but has shown promising long-term relapse prevention. Krupitsky et al. [14] demonstrated that XR-NTX combined with cognitive-behavioral therapy led to significantly lower relapse rates at 12 and 18 months. Similar conclusions were drawn by Lee et al. [5], who found XR-NTX particularly effective among criminal justice populations initiating treatment in controlled environments
Krupitsky et al. [14] found that individuals initiated on XR-NTX during residential treatment had significantly lower relapse rates at 12- and 18-month follow-ups compared to those initiated on buprenorphine. When combined with structured cognitive-behavioral therapy (CBT) and case management, patients receiving XR-NTX achieved abstinence rates exceeding 70% at one-year post-treatment. Additionally, a randomized trial by Lee et al. [12] demonstrated that XR-NTX was non-inferior to buprenorphine in preventing relapse among patients who successfully initiated the medication after detox.
Nevertheless, XR-NTX has limitations. Rates of treatment induction remain lower than with agonist therapies due to the detox requirement, and dropout risks are elevated among patients who experience early cravings or low treatment motivation. These findings indicate that XR-NTX may be most effective when targeted toward highly motivated individuals or those with strong social support systems post-discharge.
Combination with Psychosocial Support
Across MAT modalities, integrating medication with behavioral interventions and peer support enhances retention and long-term outcomes [15,16]. Stein et al. [3] emphasized that residential programs adopting comprehensive, patient-centered psychosocial care demonstrate higher rates of sustained recovery. Nunes et al. [15] highlighted that the combination of MAT with behavioral therapies such as CBT, Motivational Interviewing (MI), and trauma- informed approaches enhances medication adherence and reduces relapse. Studies also point to the importance of linking patients to peer recovery support, housing assistance, and employment services as part of a comprehensive discharge planning process [4].
In particular, retention in post-residential care programs was markedly higher when MAT was paired with 12-step facilitation, recovery coaching, and consistent follow-up through case management services [9]. These interventions were associated with improved self-efficacy, better coping strategies, and stronger recovery capital, all of which are protective factors against relapse. Thus, regardless of the specific MAT medication used, long-term sobriety is most likely when pharmacological and psychosocial supports are delivered in an integrated, continuous care framework.
Discussion
The findings of this literature review underscore important distinctions among the three primary medication-assisted treatment (MAT) options; methadone, buprenorphine, and extended-release naltrexone (XR-NTX) in the context of residential treatment for opioid use disorder (OUD). Notably, both buprenorphine and XR- NTX demonstrated superior long-term outcomes in residential settings, especially when integrated with structured behavioral health interventions, such as cognitive-behavioral therapy (CBT), motivational interviewing, and recovery coaching. Buprenorphine emerged as a particularly effective treatment for long-term abstinence and post-discharge retention due to its pharmacological profile, safety, and flexibility of use. Its partial agonist mechanism reduces the risk of overdose and promotes greater patient autonomy, particularly when transitioned to monthly injectable forms or office-based opioid treatment (OBOT) settings. These features make buprenorphine not only suitable for acute stabilization during residential care but also sustainable as a bridge into long-term outpatient recovery frameworks. Furthermore, individuals receiving buprenorphine alongside psychosocial support were more likely to report improved quality of life and reduced substance use at 12-month follow-up, as noted in Cunningham et al. [10].
Similarly, XR-NTX showed considerable promise in supporting sustained sobriety, particularly among individuals highly motivated for total abstinence. Its once-monthly dosing and opioid-blocking mechanism may appeal to patients seeking a non-addictive MAT option. Research indicates that when initiation is successful, XR NTX significantly reduces relapse rates at 12- and 18-month follow ups compared to other MATs. However, a key barrier remains: the requirement for complete opioid detoxification prior to induction. This often limits the immediate applicability of XR-NTX, especially in outpatient or lower-acuity settings.
Residential programs, with their controlled environments and 24/7 medical support, provide an ideal setting for initiating XR NTX safely and effectively. These findings support recent trends in residential care protocols that prioritize detox-to-induction pathways for XR-NTX while integrating behavioral therapies and relapse prevention planning.
Methadone, while highly effective during the acute stabilization phase, presents significant challenges in post-residential continuity due to its daily administration requirements and limited availability outside federally regulated opioid treatment programs (OTPs). Although methadone is associated with strong retention and symptom stabilization during residential care, its sustainability post- discharge often depends on the availability of OTP access and patient compliance with rigid dosing schedules. As such, relapse rates post- discharge remains moderate to high, particularly in underserved or rural communities with limited OTP infrastructure [8]. Thus, while methadone remains a foundational MAT option, it may be best suited for patients who can transition into structured outpatient OTPs with reliable transportation and adherence support.
The review also highlights the critical role of the residential treatment environment itself. Residential settings offer a unique opportunity for MAT initiation, combining structure, clinical supervision, and peer support. These factors create an ideal therapeutic milieu in which patients can stabilize, undergo detoxification, and begin medication protocols under close observation.
Moreover, residential care facilitates smoother transitions into community-based recovery networks when discharge planning includes coordinated referrals, MAT continuation, housing support, and ongoing behavioral health services. The integration of MAT with wraparound services such as peer mentoring, vocational training, and family therapy was consistently associated with improved long-term outcomes across the studies reviewed.
Overall, buprenorphine and XR-NTX demonstrate superior long term outcomes in residential settings, particularly when paired with comprehensive behavioral health support [12,14]. Methadone remains effective for acute stabilization but presents challenges related to daily dosing and continuity of care after residential discharge [8]. XR-NTX’s antagonist mechanism aligns well with patients motivated for abstinence, although detoxification requirements limit its initial accessibility [5]. Residential treatment offers an optimal milieu to initiate MAT by providing structure, medical supervision, and peer reinforcement, which facilitate better engagement and smoother transitions to outpatient care [2,3].
The evidence also underscores the critical role of tailored, patient centered care plans that consider individual factors such as comorbid mental health disorders, social determinants, and patient preferences [11,16]. Without adequate integration of behavioral supports and discharge planning, the risk of relapse remains high despite pharmacological treatment [15].
In summary, while no single MAT proves universally superior across all populations, buprenorphine and XR-NTX currently offer the most promising profiles for long-term sobriety in residential treatment settings. Their success is maximized when paired with comprehensive behavioral health interventions and robust post- discharge continuity of care. Methadone retains its value for immediate stabilization, particularly for individuals with high opioid tolerance or complex clinical profiles, but its post-residential challenges highlight the need for enhanced discharge planning and linkage to outpatient OTPs. Ultimately, optimizing MAT outcomes requires a personalized, multidisciplinary approach that considers not only pharmacological efficacy but also the structural supports available to the individual throughout the recovery continuum.
Limitations of the Research
Despite the valuable insights provided by current studies on medication-assisted treatment (MAT) for opioid use disorder (OUD) in residential settings, several limitations constrain the generalizability and interpretability of the findings.
First, selection bias remains a consistent challenge in comparative studies. Individuals who successfully initiate treatment with extended release naltrexone (XR-NTX) often present with higher levels of internal motivation, social support, or prior abstinence, factors that inherently predispose them to better treatment outcomes. This self selection effect complicates the comparison with individuals on methadone or buprenorphine, who may enter treatment under more coercive or emergent circumstances. As a result, observed differences in relapse or retention rates may reflect baseline disparities rather than the intrinsic efficacy of the medication.
Second, variability in residential treatment quality, duration, and clinical staffing further limits the ability to generalize across studies. Programs differ in the intensity of therapeutic interventions, access to peer support, staffing ratios, and discharge planning protocols, all of which are known to influence treatment outcomes. For instance, a patient receiving XR-NTX in a high resource facility with comprehensive behavioral health support may experience significantly different results than a similar patient in a lower-resourced setting. Without standardized treatment conditions across studies, it becomes difficult to isolate the specific effects of the medication itself from those of the environment in which it is delivered.
Third, many existing studies suffer from short follow-up periods, with the majority tracking participants for only 6 to 12 months post- treatment. Few studies extend beyond 18 months, which limits our understanding of the durability of MAT benefits over time. Given that sustained recovery often involves cycles of relapse and re- engagement, longer-term data are essential to determine whether initial treatment success translates into enduring sobriety and improved life functioning. The lack of long-term outcomes also makes it challenging to assess the role of MAT in promoting broader psychosocial recovery, including employment stability, reduced criminal justice involvement, and family reunification.
Fourth, there is inconsistent attention to social determinants of health across the MAT literature. Factors such as stable housing, employment opportunities, access to transportation, community stigma, and family support play critical roles in recovery outcomes but are often underreported or unevenly measured. These external factors can moderate the effectiveness of MAT by influencing treatment adherence, follow-up care engagement, and overall quality of life. The absence of systematic assessment of these variables reduces the ability to apply findings equitably across diverse populations, especially those from marginalized or underserved communities.
Lastly, racial and ethnic disparities in MAT access and outcomes remain underexplored. Although some studies report participant demographics, few disaggregate outcomes by race, gender, or socioeconomic status. This oversight limits the field's capacity to understand how structural inequities intersect with MAT engagement and success, particularly for populations disproportionately affected by both opioid use and systemic barriers to care.
Several limitations are noted within the current literature. Selection bias is common, as patients opting for XR-NTX may be inherently more motivated, skewing comparative results [12]. Variability in the quality, duration, and intensity of residential treatment programs complicates generalizations across studies [3]. Additionally, most research includes follow-up periods of less than 18 months, limiting insight into truly sustained recovery [14]. Finally, social determinants such as housing stability and family support, known to influence MAT success, are inconsistently accounted for, which hampers a holistic understanding of long-term outcomes [16].
Collectively, these limitations point to the need for more rigorous, longitudinal, and equity-focused research in order to accurately evaluate the long-term effectiveness of MAT modalities in residential treatment settings. Future studies should employ more robust research designs that control for motivational and environmental variables, incorporate social determinants of health, and ensure representation across diverse demographic and geographic populations.
Future Considerations
Building upon the current evidence base, future research on medication-assisted treatment (MAT) for opioid use disorder (OUD) in residential treatment settings should aim to address existing gaps and expand our understanding of what contributes to long-term recovery. One of the most pressing needs is for longitudinal studies extending beyond 24 months, which can more accurately capture the durability of MAT-related outcomes, including sustained abstinence, psychosocial functioning, and quality of life. Given that relapse often occurs after the first year of treatment, short-term follow-ups fail to fully reflect the challenges and successes individuals face in maintaining sobriety over time.
Additionally, there is a need for well-designed randomized controlled trials (RCTs) that compare the effectiveness of different MAT types specifically methadone, buprenorphine, and extended release naltrexone, when initiated within standardized residential treatment programs. These trials should control for the intensity and type of psychosocial interventions offered, such as cognitive behavioral therapy (CBT), motivational interviewing (MI), or 12 step facilitation. Standardizing these supports would help isolate the pharmacological effects of the medication from the influence of the treatment environment and allow for more meaningful comparisons across MAT modalities.
Moreover, future investigations should explore personalized or stratified approaches to MAT, taking into account individual patient characteristics such as severity of addiction, co-occurring mental health disorders, trauma history, prior treatment attempts, and motivational levels. The integration of precision medicine principles, matching specific treatment modalities to individual profiles, may improve treatment adherence, engagement, and overall outcomes. This direction would benefit from the development and validation of clinical decision-making tools that help providers tailor MAT choices to patient-specific needs.
Another critical area for future exploration is the role of recovery housing and community-based support networks in sustaining MAT outcomes following residential treatment discharge. Stable housing environments that support sobriety, such as recovery residences or sober living programs, have been associated with improved retention in care and reduced relapse. However, empirical studies evaluating the intersection of MAT and recovery housing remain limited. Research should also assess the impact of wraparound services such as employment assistance, peer recovery coaching, and family support programs on post-treatment success, particularly for individuals transitioning back into high-risk or underserved communities.
Lastly, future studies should intentionally include diverse populations and settings, ensuring representation across race, gender, socioeconomic status, and geography. By incorporating social determinants of health and focusing on health equity, researchers can develop interventions that are not only effective but also inclusive and responsive to the unique barriers faced by marginalized groups affected by the opioid crisis.
Future research should focus on long-term longitudinal studies exceeding 24 months to capture sustained recovery trajectories beyond the acute post-treatment phase [12]. Randomized controlled trials comparing MAT modalities initiated in residential care with standardized psychosocial supports are needed to isolate the medication effect and optimize integrated treatment protocols [11,15]. Personalized MAT approaches that consider patient-specific factors such as psychiatric comorbidity, motivation, and prior treatment history, may improve retention and outcomes [16]. Further exploration of recovery housing and community-based supports post-discharge will clarify their role in enhancing MAT effectiveness [3]. Finally, research should prioritize diverse populations to address health disparities and ensure equitable access to evidence-based MAT services [2].
In summary, a forward-looking research agenda should prioritize long-term, individualized, and context-sensitive investigations that reflect the complex realities of recovery. This approach will not only refine clinical decision-making but also inform policies and practices that support sustained recovery and improve the lives of those affected by opioid use disorder.
Conclusion
This comprehensive literature review affirms that there is no one size-fits-all medication-assisted treatment (MAT) that is universally superior for every individual with opioid use disorder (OUD) in residential treatment settings. However, the current body of evidence consistently highlights buprenorphine and extended-release naltrexone (XR-NTX) as the MAT modalities with the strongest support for promoting long-term sobriety and retention when initiated during residential care. These medications offer distinct pharmacological advantages. Buprenorphine with its partial agonist profile provide a favorable safety margin, and XR-NTX with its antagonist properties aligning well with patients seeking complete abstinence.
A critical factor underlying the success of these MAT options is their integration with comprehensive, person-centered behavioral health supports. The combination of pharmacotherapy with evidence-based psychosocial interventions including cognitive-behavioral therapy (CBT), motivational enhancement therapy (MET), and peer recovery services, consistently correlates with better treatment adherence, reduced relapse rates, and improved overall functioning. This integration underscores the importance of addressing the multifaceted nature of OUD, which encompasses biological, psychological, and social dimensions.
Given the heterogeneity of patients presenting to residential treatment, differing in addiction severity, co-occurring mental health conditions, motivation, and social support systems. Treatment programs should prioritize flexible and individualized MAT protocols. These approaches enable clinicians to tailor medication choices and psychosocial interventions to meet the unique needs and preferences of each individual, thereby optimizing engagement and outcomes.
Clinical and Policy Recommendations
1. Staffing Models: Residential programs should adopt interdisciplinary staffing models that include addiction medicine specialists, psychiatric providers, trained nursing staff, peer recovery coaches, and licensed behavioral health clinicians. This team-based approach ensures the coordinated delivery of MAT alongside evidence-based psychotherapy and wraparound services.
2. Medication Induction Protocols: Programs should develop clear and flexible medication induction protocols that allow for the timely initiation of buprenorphine or XR-NTX based on a thorough clinical assessment. Incorporating shared decision making and motivational interviewing during induction can improve patient engagement and adherence.
3. Discharge Planning: Effective discharge planning must begin at admission and include warm handoffs to outpatient MAT providers, linkage to recovery housing, continued access to peer support networks, and enrollment in intensive outpatient or community-based services. Establishing formal partnerships with outpatient clinics can reduce treatment gaps and prevent relapse.
4. Program Design Implications: Residential facilities should consider integrating longer-stay options or step-down levels of care for individuals needing extended stabilization. Programs should also invest in ongoing training for staff on best practices in MAT delivery, trauma-informed care, and stigma reduction.
5. Policy Advocacy: At the systems level, providers should advocate for insurance reimbursement models that support bundled care (e.g., combining MAT with psychosocial services) and regulatory frameworks that allow residential programs to initiate and maintain MAT without barriers. Emphasizing the need for parity between mental health, substance use, and medical services is critical for sustainable delivery.
In conclusion, residential treatment centers play a pivotal role as initiation points for effective MAT strategies that can significantly enhance long-term recovery trajectories. By embracing evidence based, patient-centered models of care that integrate pharmacological and behavioral treatments and by operationalizing supportive staffing structures, induction protocols, and discharge processes, these programs can better support individuals in overcoming OUD and achieving sustained sobriety. Future research and policy should continue to refine these approaches to maximize access, equity, and long-term success for diverse populations affected by the opioid epidemic.
Competing Interests:
The authors declare that they have no competing interests.
References
Centers for Disease Control and Prevention (CDC). (2024). Overdose Deaths Remain High in the U.S. View
Volkow, N. D., & Collins, F. S. (2017). The role of science in addressing the opioid crisis. New England Journal of Medicine, 377(4), 391–394. View
Stein, B. D., Gordon, A. J., Sorbero, M., Dick, A. W., Pacula, R. L., Burns, R. M., & Gordon, A. J. (2020). Trends in buprenorphine and extended-release naltrexone receipt among adults with opioid use disorder in U.S. residential treatment facilities, 2015–2017. Journal of Addiction Medicine, 14(6), 500–507.
Laudet, A. B. (2007). What does recovery mean to you? Lessons from the recovery experience for research and practice. Journal of Substance Abuse Treatment, 33, 243-256. View
Lee, J. D., Friedmann, P. D., Kinlock, T. W., Nunes, E. V., Boney, T. Y., Hoskinson, R. A., Jr., ... & O’Brien, C. P. (2016). Extended-release naltrexone to prevent opioid relapse in criminal justice offenders. New England Journal of Medicine, 374(13), 1232–1242. View
Comer, A. L., Jinadasa, T., Sriram, B., Phadke, R. A., Kretsge, L. N., Nguyen, T. P. H., … Cruz-Martín, A. (2020). Increased expression of schizophrenia-associated gene C4 leads to hypoconnectivity of prefrontal cortex and reduced social interaction. PLoS Biology, 18(1). View
Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2019). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews, 3, CD002209. View
Sordo, L., Barrio, G., Bravo, M. J., Indave, B. I., Degenhardt, L., Wiessing, L., ... & Pastor-Barriuso, R. (2017). Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ, 357, j1550. View
Timko, M., Schneider, M., et al. (2016). Treatment-Based Classification System for Low Back Pain: Revision and Update. Phys Ther. 96(7):1057-66. View
Cunningham, C. O., Sohler, N. L., Korin, L., Galea, S., & Kunins, H. V. (2021). Residential initiation of buprenorphine and outcomes at 12 months: A comparative study. Journal of Substance Abuse Treatment, 124, 108-116.
Weiss, R. D., Potter, J. S., Fiellin, D. A., Byrne, M., Connery, H. S., Dickinson, W., ... & Ling, W. (2019). Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: A randomized clinical trial. JAMA Internal Medicine, 179(1), 13–22. View
Lee, J. D., Nunes, E. V., Novo, P., Bachrach, K., Bailey, G. L., Bhatt, S., ... & Rotrosen, J. (2018). Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): A multicenter, open-label, randomized controlled trial. The Lancet, 391(10118), 309–318. View
Volkow, N.D., Jones, E.B., Einstein, E.B. and Wargo, E.M. (2019). Prevention and Treatment of Opioid Misuse and Addiction: A Review. JAMA Psychiatry, 76, 208-216. View
Krupitsky, E., Blokhina, E., Verbitskaya, E., et al. (2020). Long- term effectiveness of extended-release naltrexone in OUD recovery: A randomized clinical trial. The Lancet Psychiatry, 7(2), 104-112.
Nunes, E. V., Levin, F. R., Reilly, M. P., & El-Bassel, N. (2021). Behavioral interventions in conjunction with MAT: Systematic review and meta-analysis. Addiction, 116(4), 777–791.
Krawczyk, N., Feder, K., Fingerhood, M., & Agus, D. (2020). Stigma and discrimination towards patients with opioid use disorder: The role of medication-assisted treatment in residential treatment settings. Substance Abuse, 41(3), 263–269.