Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-181
https://doi.org/10.33790/jrpr1100181Research Article
Effect of Posture on Hip Abductor Strength: Implications for Clinical Practice
Steven D. Pheasant PT, PhD1, Richard F. Haydt PT, DPT, OCS, MTC, FAAOMPT2
Professor, Departmnt of Physical Therapy, Misericordia University, 301 Lake Street Dallas, PA, United States.
Corresponding Author Details: Steven D. Pheasant PT, PhD, Professor, Departmnt of Physical Therapy, Misericordia University, 301 Lake Street Dallas, PA, United States.
Received date: 09th June, 2025
Accepted date: 07th August, 2025
Published date: 09th August, 2025
Citation: Pheasant, S. D., & Haydt, R. F., (2025). Effect of Posture on Hip Abductor Strength: Implications for Clinical Practice. J Rehab Pract Res, 6(2):181.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: The slumped sitting (SS) posture has been noted through clinical observation to contribute to hip abductor strength decline. The purpose of the study was to examine the influence of three postures on hip abductor strength when controlling for the testing position: prone lying (PL), erect sitting (ES) and slumped sitting.
Study Design: A cohort study, with subjects serving as their own controls.
Method: 80 subjects ages 18-26. Each subject assumed the PL posture for 5 minutes after which dominant hip abductor strength was immediately tested using a Hand-Held Muscle Testing Dynamometer (HHMTD). Hip abductor muscle strength was tested in the side-lying position. Hip abductor strength was then tested again immediately after each of the following conditions, 5 minutes in the ES posture, 5 additional minutes in the PL position and 5 minutes in the SS posture.
Findings: The average decrease in hip abductor strength following the SS posture was 5%. Twenty-nine percent of the subjects demonstrated >10% decline in hip abductor strength following the SS posture. The average strength decline of those with >10% decrease was 15%. There were no significant differences between the ES and PL strength values.
Conclusion: The SS posture can adversely influence hip abductor strength. The potential influence of the SS posture should be considered when evaluating hip pathology, particularly with conditions involving decreased hip abductor strength.
Level of Evidence: Level III
Key Words: Slumped Sitting, Erect Sitting, Hand-Held Dynamometer
Introduction
Deficient hip abductor strength can be associated with pathologic conditions not only at the hip, but at the knee and ankle as well [1-16]. Accordingly, assessment of hip abductor strength using resisted isometric strength testing (RIST) is a routine component of a lower quarter musculoskeletal examination [17,18]. The authors’ clinical observations have noted the posture assumed by an individual immediately prior to RIST can influence the force production of the hip abductors. The phenomenon of posture influencing muscle strength was documented in a previous study by the authors in which a decline in upper extremity strength was reported [19]. In light of the authors’ clinical observations, previous research findings, as well as the desire to obtain reliable isometric hip abduction strength data (for diagnostic and rehabilitation decisions); the authors developed the current study to investigate if slumped sitting (SS) posture can influence hip abductor strength testing. The authors’ hypothesis is that the SS posture will result in a decline in hip abductor strength when controlling for the test position.
Materials and Methods
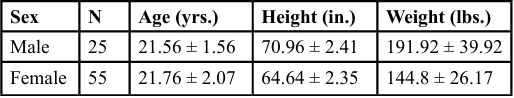
The design was a cohort study, with participants serving as their own controls. Participants included a convenience sample of 80 healthy volunteers (male 25/female 55) between 18 and 26 years of age from a university setting (Table 1). Individuals were excluded from participation for the following reasons: a prior history of spinal surgery; a history of neck or back pain with radiating symptoms into the arms or legs; current spinal pain; a history of dominant hip surgery or a history of dominant hip injury within the last year.
The hip abductor strength of the dominant hip of each subject was tested following 5 minutes of sustained positioning under each of the following conditions: 1.) first prone lying (PL1) posture, 2.) slumped sitting (SS) posture, 3.) second prone lying (PL2) posture and 4.) erect sitting (ES) posture. The SS posture and ES posture were alternated for order with each successive subject to minimize learning and/ or fatigue effects. For example; the first subject was positioned in the PL1 posture for 5 minutes and then immediately tested, the SS posture for 5 minutes and immediately tested, the PL2 posture for 5 minutes and immediately tested and the ES posture for five minutes and immediately tested. The order of postures and testing for the second subject was PL1, ES, PL2 and SS. This alternating pattern of assignment was maintained throughout the testing of the 80 subjects. The dominant hip was determined by the leg each subject chose to kick a ball.
The 5-minute period of posture maintenance is consistent with the authors’ clinical observations for strength changes to occur in the hip abductors. It also coincides with the time frame used in our previous study that examined the influence of cervical posture on shoulder external rotator strength [19].
The PL posture (PL1 and PL2) involved having each subject lie face down on the table with the cervical spine in neutral while the forehead rested on the hands (Figure 1). The SS posture was defined as a position of relaxed, unsupported, slumped sitting. This was characterized by a protruded cervical spine, protracted/abducted scapulae and thoracolumbar flexion (Figure 2). Each subject was cued to maintain the head and eyes level in the transverse plane by focusing his or her gaze on a mark on the wall. The ES posture was defined by the vertical alignment of the following: tragus of the ear, bodies of the cervical vertebrae, acromion of the scapula, coronal mid-line of the thorax with the maintenance of the lumbar lordosis [20]. Due to the frontal plane posture alignment, the scapulae were drawn into a retracted/adducted position (Figure 3). In both the SS and ES postures, the subjects were seated unsupported on a table with feet positioned on a stool for stability and comfort.

Figure 1. The PL posture (P1 and P2) involved having each subject lie face down on the table with the cervical spine in neutral while the forehead rested on the hands.

Figure 2. The SS posture was defined as a position of relaxed, unsupported, slumped sitting. This was characterized by a protruded cervical spine, protracted/ abducted scapulae and thoracolumbar flexion. Each subject was cued to maintain the head and eyes level in the transverse plane by focusing his or her gaze on a mark on the wall.

Figure 3. The ES posture was defined by the vertical alignment of the following: tragus of the ear, bodies of the cervical vertebrae, acromion of the scapula, coronal mid-line of the thorax with the maintenance of the lumbar lordosis.
A sole investigator was charged with visually monitoring each subjects’ lying and sitting posture under each condition to assure the criterion of the condition was maintained throughout each 5-minute period. Verbal and tactile cues were provided to each subject as needed throughout the test period to maintain the designated posture. All subjects were successful in maintaining each posture for the required 5 minutes.
For consistency all strength testing of the dominant hip abductors was performed by the same designated investigator using a Micro FET3 Hand-Held Muscle Testing Dynamometer (HHMTD). Wilder et al. [21] determined the side-lying testing position to be more reliable than either the supine or standing positions using a HHMTD when compared by coefficient of variation (side-lying 3.7%, standing 4.2%, supine 6.1%).Wilder et al. also determined test-retest reliability for the side-lying hip abductor strength testing protocol to be high to moderate with an ICC of .902. Strength testing consisted of two 5 second “make” isometric tests for hip abduction. “Make” isometric testing (participant exerting force against a stationary tester) was used since it has been demonstrated to be more reliable than “break” isometric testing (tester exerting force to overcome a stationary participant) when used to test shoulder external rotator strength [22]. Arnold et al. demonstrated test-retest reliability (ICC of .93) using a manually stabilized dynamometer testing hip abductor strength in supine [23].
Fifteen active hip abduction movements in the standing position served as a warm-up to testing for the dominant hip abductors. Two sub-maximal and one maximal practice isometric strength testing trials were performed to familiarize the subjects to the testing protocol prior to the initial period of prone lying. All isometric strength testing was performed with the subject in side-lying to standardize the testing position. Hip abductor strength testing was performed from the side-lying position with the dominant hip up. The subjects’ dominant lower extremity (up) position for strength testing was 10° of hip joint abduction, 0° of hip joint external rotation, and 0° of hip joint flexion. The dominant leg rested on a stool that was positioned to maintain the hip in 10° of abduction. The non-dominant lower extremity (down) position was 30° of hip flexion and 30° of knee flexion (Figure 4). Subjects were permitted to support his/her head with the non-dominant side (down) upper extremity. Subjects were not permitted to stabilize his/her trunk by using the dominant side (up) upper extremity to push onto the table. HHMTD was held perpendicular to the dominant femur and positioned 5 cm proximal to the lateral femoral epicondyle. Each subject was instructed to provide a maximal effort for 5 seconds while the tester maintained the stationary position of the HHMTD. A 15 second rest period separated the two trials.
Study approval was granted by the University Institutional Review Board. Informed consent was obtained and the rights of the subjects protected.
Results
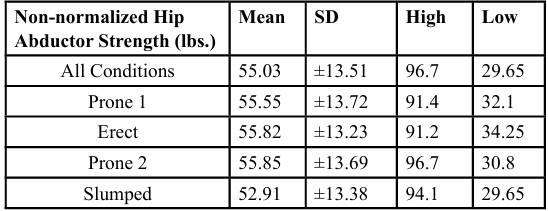
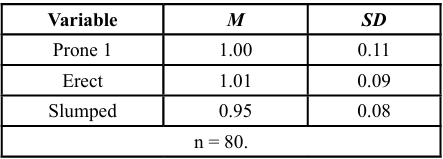
Hip abductor mean strength values are provided for each postural condition. (Table 2)

Figure 4. The subjects’ dominant lower extremity (up) position for strength testing was 10° of hip joint abduction, 0° of hip joint external rotation, and 0° of hip joint flexion. The dominant leg rested on a stool that was positioned to maintain the hip in 10° of abduction to aid preparation for “make” testing. The non dominant lower extremity (down) position was 30° of hip flexion and 30° of knee flexion.
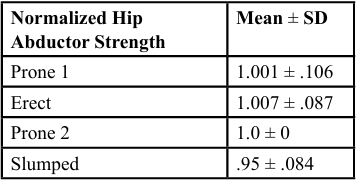
Mean hip abductor strength values for each postural condition were normalized for each subject (Table 3) (Figure 5). Strength values were normalized to the PL2 strength means due to the wide variation in hip abductor strength among subjects. The normalized hip abductor strength mean values were calculated by obtaining the mean of the 2 trials for each subject under each condition and dividing by the mean of each subject’s PL2 trials.
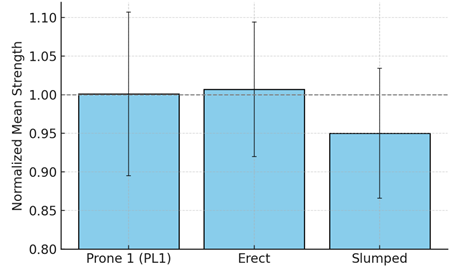
Figure 5: Normalized Means Strength values for each condition were normalized to the PL2 strength means
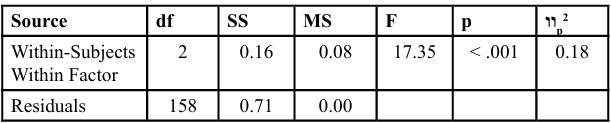
ANOVA with repeated measures indicated significance for hip abductor strength differences among the three groups of normalized hip abductor strength means F(2, 158) = 17.35, p < 0.001. (Table 4, Table 5, Table 6) Tukey post hoc comparisons indicated PL1 was significantly greater than SS, t(79) = 4.64, p <0 .001 and ES was significantly greater than SS, t(79) = 6.22, p < 0.001. No significant difference was determined between PL1 and ES t(79) = -0.55, p=0.848. An average 5% decline in hip abductor strength was demonstrated following SS. Twenty-nine percent of the subjects (23/80) demonstrated a decline in hip abductor strength of ≥10%. The average decline in this sub-population was 15%. The 10% decline was subjectively determined by the researchers to attempt to identify the presence of a sub-population of subjects experiencing a larger magnitude of strength decline in line with the authors’ clinical observations and the authors’ previous study [19]. In acknowledgement of the raw data, 8.75% (7/80) experienced a decline in hip abductor strength of ≥10% following 5 minutes in the ES posture. The Assumption of Normality was met using a Q-Q scatterplot [24]. Mauchly’s Test of Sphericity was satisfied [25]. No outliers were detected based on Mahalanobis distances [26].
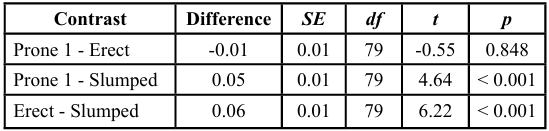
Table 6: The Marginal Means Contrasts for each Combination of Within-Subject Variables for the Repeated Measures ANOVA
Discussion
The results of the current study indicate a decline in hip abductor strength following five minutes in a SS posture. There was a 5% decline in hip abductor strength in the SS condition compared to the ES and PL conditions. Twenty-nine percent (23/80) of the subjects experienced a hip abductor strength decline of equal to or greater than 10%. The average strength decline in this sub-population of subjects was 15%. The decline in hip abductor strength appears transient in nature since the hip abductor strength returned to baseline PL values once removed from the SS posture and the PL posture was assumed.
These findings from the current study are similar to the those reported in the authors’ previous study in which shoulder external rotator strength changes occurred in response to various sitting postures [19]. That study reported an 8% decline in shoulder external rotator strength in response to five minutes in a SS posture. Additionally, that study identified a sub-population of 32% who experienced a decline in shoulder external rotator strength of ≥ 10% with an average strength decline of 19% [19]. The authors’ previous study also noted that shoulder external rotator strength decline was transient in nature as shoulder external rotator strength values returned to baseline once subjects returned to the neutral cervical posture.
The intent of the current study was solely to identify whether hip abductor strength was influenced by various postures (PL, SS or ES). The data indicates a strength decline phenomenon does occur in the lower extremity similar to that reported for the upper extremity when subjected to SS spinal stresses [19]. The author’s surmise the spinal mechanism associated with motor nerve root compression resulting in transient strength decline is different in the two studies with the previous study likely stenosis and the current study likely disc related.
The authors chose to sample the strength of the hip abductors for several reasons. First, the authors clinically observed the hip abductors as a lower extremity muscle group that experiences a strength decline in response to the SS posture. Second, the hip abductors are of functional significance for stabilizing the hip and pelvis in the frontal plane during single limb stance activities [1-10]. Third, the gluteus medius and minimus are single joint hip abductors whose force production is less likely to be influenced by the postures of interest (PL, SS, ES) minimizing length tension considerations as factor. Lastly, the hip abductors were chosen due to their predominant L5 nerve root innervation and the high incidence of L5 nerve root involvement in individuals with lumbar intervertebral disc pathology which the authors surmise may be a potential contributing cause for the observed phenomenon [27,28].
Although the authors’ intent was not to determine the cause of the hip abductor strength decline, one may consider possible explanations for the observed findings. The authors surmise a transient L5 nerve root compression may be responsible for the hip abductor strength decline observed in response to the SS posture [29,30]. The offset load to the lumbar intervertebral discs that accompanies the SS posture, particularly in this age group, may result in deformation of the discs’ posterior annulus to the extent to encroach upon the motor aspect of the L5 nerve root [31-33]. While the aforementioned mechanism may explain the strength decline observed in the current study, it does not account for the absence of pain and/or paresthesia common to nerve root compression and associated radiculopathy [34]. Other potential explanations for the cause of L5 nerve root compression resulting in associated gluteus medius weakness include lumbar stenosis, and spondylolisthesis. These explanations are less likely due to the age of participants in the authors’ current study [35].
The phenomenon of a myotomal strength deficit without pain or other sensory symptoms has been described in the literature as “painless weakness” or “painless motor radiculopathy” [36-38]. Lipetz et al [36], in a case series, described patients presenting with radiculopathy due to documented lumbar intervertebral disc pathology whose clinical presentation was profound motor weakness in the absence of pain. Siller et al [38], in a retrospective study, reported that 3.9% of patients undergoing cervical decompression surgery had a pre-operative diagnosis of painless motor radiculopathy. In a study of 100 college-age participants, the authors’ previous study [19] also suggested a painless motor radiculopathy to explain a posture induced transient shoulder external rotator muscle weakness. Although the SS posture can potentially cause intervertebral disc deformation and is surmised to have contributed to the decline in hip abductor strength in the current study, the precise mechanism resulting in the observed strength decline remains speculative.
Clinical relevance
The clinical relevance of the study lies with the recognition that a SS posture assumed prior to hip abductor strength testing will likely result in a 5% decline in hip abductor force production. A failure to recognize this SS posture induced strength decline would impact not only the reliability of the hip abductor strength measurement but would also bias any resultant diagnostic or rehabilitative decisions.
The more significant finding of the study is the identification of the sub-population of individuals 29% (23/80) who are more susceptible to the SS posture induced hip abductor strength decline. These individuals are likely to experience a decline in hip abductor strength of 15 %, if tested following a period in the SS posture. It would follow that these individuals would be more likely to experience the consequences of a more profound decline in hip abductor strength for example: gait deviations, hip muscle strain, hip joint pathology and associated knee and ankle dysfunction requiring formal intervention.
Therefore, individuals who present with conditions associated with a hip abductor strength impairment, should be evaluated for a SS posture induced cause of the strength impairments by re examining the hip abductor strength after a period of erect sitting. This will confirm the role the SS posture played in the hip abductor strength decline so intervention can be directed more effectively. Accordingly, if hip abductor strength improves in response to the ES posture, posture correction into lumbar extension should be a critical element in the intervention as this will address the underlying cause of the strength decline. On the other hand, if the SS posture is overlooked as a contributing factor to the strength decline, this deficit and any associated limitations will likely persist since the underlying cause of the decline (SS posture) would continue to go unaddressed.
The authors note the following study limitations: 1. Participants in the current study were young, healthy, and asymptomatic individuals which limits generalization of findings to other populations. 2. A limitation was the five-minute time frame spent in the postures of interest. Shorter or longer time in the stated postures may have produced different findings. 3. Future research could include the application of electrodiagnostic and/or diagnostic imaging to provide additional evidence confirming L5 nerve compression and it’s source as the explanation for hip abductor weakness found in the current study.
The current study indicates a SS posture should be considered as a contributing factor to hip abductor weakness. Previous studies indicate that hip abductor weakness can factor in hip pathological conditions such as trochanteric bursitis [11], acetabular labral involvement [12], gluteus medius strains [13], and hip degenerative joint disease [14,16]. Hip abductor weakness also factors in knee pathologies such as patellar femoral syndrome and various knee and ankle ligamentous injuries [3-10]. Specifically, hip abductor weakness is a common factor associated with anterior cruciate ligament injury [6,7]. A practical implication to ponder is the following scenario: a female field hockey player sitting on the bench in a SS posture enters the game. If this flexed lumbar position, as noted in the current study, is maintained during play resulting in a decrease of hip abductor strength, she may be more vulnerable to the above injuries.
Conclusion
The current study identified time spent in the SS posture, prior to strength testing, can result in hip abductor strength decline that returns to normal after time spent in PL or ES postures. PL or ES postures prior to hip abductor strength testing do not result in the same strength decline. Certain individuals are more susceptible to the SS induced hip abductor strength decline than others. Therefore, when assessing and treating LE pathologies that present with hip abductor weakness, it is imperative for clinicians to recognize the influence SS posture could have on hip abductor strength. Overlooking individuals with habitual SS posture as a factor in hip abductor strength decline could lead to inaccurate conclusions regarding strength, continued hip abductor weakness, further decline, potential LE pathologies and possible permanent weakness.
Competing Interests:
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors would like to acknowledge and thank the following Doctor of Physical Therapy students at Misericordia University for their assistance with various aspects of the study: Joseph Cassaro DPT, Trevor George DPT, Thomas Machi DPT, Julianne Munda DPT, Robin O’Dell DPT, Jerry Struble DPT, Brad Thomas DPT, Chris Tiffany DPT and Robert Wozniak DPT.
The authors would also like to thank John Pheasant MS Mechanical Engineering for his review of the manuscript and thoughtful insight.
References
Neumann, D. A. (2017). Kinesiology of the musculoskeletal system: Foundations for rehabilitation (3rd ed., pp. 512–515). St. Louis, MO: Elsevier. View
O’Sullivan, K. O., Smith, S. M., & Sainsbury, D. (2010). Electromyographic analysis of the three subdivisions of the gluteus medius during weight-bearing exercise. Sports Medicine, Arthroscopy, Rehabilitation, Therapy & Technology, 2(17), 1–9. View
Cashman, G. E. (2012). The effect of weak hip abductors or external rotators on knee valgus kinematics in healthy subjects: A systematic review. Journal of Sport Rehabilitation, 21(3), 273–284.View
Ford, K. R., Nguyen, A. D., & Dischiavi, S. L. (2015). An evidence-based review of hip focused neuromuscular exercise interventions to address dynamic lower extremity valgus. Open Access Journal of Sports Medicine, 6, 291–303. View
Hewett, T. E., Myer, G. D., Ford, K. R., et al. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. American Journal of Sports Medicine, 33(4), 492–501. View
Hewett, T. E., Myer, G. D., & Ford, K. R. (2006). Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. American Journal of Sports Medicine, 34(2), 299–311. View
Kayambashi, K., Ghoddosi, N., & Straub, R. K. (2016). Hip muscle strength predicts non contact anterior cruciate ligament injury in male and female athletes: A prospective study. American Journal of Sports Medicine, 44(2), 355–361. View
Lee, S. P., & Powers, C. M. (2014). Individuals with diminished hip abductor muscle strength exhibit altered ankle biomechanics and neuromuscular activation during unipedal balance tasks. Gait & Posture, 39(3), 933–938. View
Powers, C. M. (2003). The influence of altered lower extremity kinematics on patellofemoral joint dysfunction: A theoretical perspective. Journal of Orthopaedic & Sports Physical Therapy, 33(11), 639–649. View
Wilson, J. D., & Davis, I. S. (2008). Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clinical Biomechanics, 23(2), 203–211.View
Lustenberger, D. P., Ng, V. Y., & Best, T. M. (2011). Efficacy of treatment of trochanteric bursitis: A systematic review. Clinical Journal of Sport Medicine, 21(5), 447–453. View
Yazbek, P. M., Ovanessian, V., & Martin, R. L., et al. (2011). Nonsurgical treatment of acetabular labrum tears: A case series. Journal of Orthopaedic & Sports Physical Therapy, 41(5), 346–353. View
Lindner, D., Shohat, N., & Botser, I., et al. (2015). Clinical presentation and imaging results of patients with symptomatic gluteus medius tears. Journal of Hip Preservation Surgery, 2(3), 310–315. View
Arokoski, M. H., Arokoski, J. P., & Haara, M., et al. (2002). Hip muscle strength and muscle cross-sectional area in men with and without hip osteoarthritis. Journal of Rheumatology, 29(10), 2185–2194.View
Rasch, A., Bystrom, A. H., Dalen, N., et al. (2007). Reduced muscle radiological density, cross-sectional area and strength of major hip and knee muscles in 22 patients with hip osteoarthritis. Acta Orthopaedica, 78, 505–510.View
Marshall, A. R., de Noronha, M., Zacharias, A., et al. (2016). Structure and function of the abductors in patients with hip osteoarthritis: Systematic review and meta-analysis. Journal of Back and Musculoskeletal Rehabilitation, 29(2), 191–204. View
Cyriax, J. (1982). Textbook of orthopaedic medicine: Diagnosis of soft tissue lesions (Vol. 1, 8th ed., p. 44). London: Bailliere Tindall. View
Magee, D. J. (1992). Orthopedic physical assessment (2nd ed., pp. 338–339). Philadelphia, PA: W.B. Saunders. View
Pheasant, S., Haydt, R., Gottstein, T., et al. (2018). Shoulder external rotator strength in response to various sitting postures: A controlled laboratory study. International Journal of Sports Physical Therapy, 13(1), 50–57. View
Kendall, F. P., & McCreary, E. K. (1983). Muscles: Testing and function (3rd ed., p. 280). Baltimore, MD: Williams & Wilkins.
Wilder, K. S., Glatthorn, J. F., Bizzini, M., et al. (2009). Assessment of hip abductor muscle strength: A validity and reliability study. Journal of Bone and Joint Surgery—American Volume, 91(11), 2666–2672. View
Stratford, P. W., & Balsor, B. E. (1994). A comparison of make and break tests using a hand-held dynamometer and the Kin Com. Journal of Orthopaedic & Sports Physical Therapy, 19(1), 28–32. View
Arnold CM, Warkentin KD, Chilibeck PD, Magnus CR. (2010). The reliability and validity of handheld dynamometry for the measurement of lower-extremity muscle strength in older adults. J Strength Cond Res, 24(3):815-24. View
DeCarlo, L. T. (1997). On the meaning and use of kurtosis. Psychological Methods, 2(3), 292-307. View
Field, A. (2013). Discovering statistics using SPSS (4th ed.). Sage Publications View
Newton, R. R., & Rudestam, K. E. (2012). Your statistical consultant. Sage Publications View
Hoppenfeld, S. (1977). Orthopaedic neurology (pp. 56–57). Philadelphia, PA: Lippincott. View
Deyo, R. A., Rainville, J., & Kent, D. L. (1992). What can the history and physical examination tell us about low back pain? JAMA, 268(6), 760–765. View
Berry, J. A., Elia, C., Saini, H. S., Miulli, D. E., & others. (2019). A review of lumbar radiculopathy, diagnosis, and treatment. Cureus, 11(10), e5934. View
Lee-Robinson, A., & Lee, A. T. (2010). Clinical and diagnostic findings in adults with lumbar spine radiculopathy. American Journal of Clinical Medicine, 7(2), 70–77 View
Alexander, L. A., Hancock, E., & Agouris, I., et al. (2007). The response of the nucleus pulposus of the lumbar intervertebral discs to functionally loaded positions. Spine, 32(14), 1508 1512. View
Wilke, H. J., Neef, P., Cami, M., et al. (1999). New in vivo measurements of pressures in the intervertebral disc in daily life. Spine, 24(8), 755–762. View
Nachemson, A. (1965). The effect of forward leaning on lumbar intradiscal pressure. Acta Orthopaedica Scandinavica, 35, 314 328. View
Casey, E. (2011). Natural history of radiculopathy. Physical Medicine and Rehabilitation Clinics of North America, 22(1), 1–5.View
Lee, S., Kang, J. H., Srikantha, U., Jang, I., & Oh, S. (2014). Extraforaminal compression of the L-5 nerve root at the lumbosacral junction: clinical analysis, decompression technique, and outcome: Clinical article. Journal of Neurosurgery: Spine SPI, 20(4), 371-379. View
Lipetz, J. S., Misra, N., Silber, J. S., et al. (2005). Resolution of pronounced painless weakness arising from radiculopathy and disk extrusion. American Journal of Physical Medicine & Rehabilitation, 84(7), 528–537. View
Gaffney, C. J., & Spiker, W. R. (2016). Painless weakness from lumbar disc herniation: Recommended management and outcomes. Seminars in Spine Surgery, 28, 31–36. View
Siller, S., Kasem, R., & Witt, T. N., et al. (2018). Painless motor radiculopathy of the cervical spine: Clinical and radiological characteristics and long-term outcomes after operative decompression. Journal of Neurosurgery: Spine, 28(6), 1–9. View