Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-159
https://doi.org/10.33790/jrpr1100159Research Article
Effectiveness of Neuro-vision Educational Modules on Knowledge and Confidence
Sanchala Sen, and Jennifer Worischeck*
Department of Occupational Therapy, Winston-Salem State University, Winston-Salem, NC, United States.
Corresponding Author Details: Jennifer Worischeck, Department of Occupational Therapy, Winston-Salem State University, Winston-Salem, NC, United States.
Received date: 24th January, 2025
Accepted date: 22nd February, 2025
Published date: 24th February, 2025
Citation: Sen, S., & Worischeck, J., (2025). Effectiveness of Neuro-vision Educational Modules on Knowledge and Confidence. J Rehab Pract Res, 6(1):159.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The purpose of this study was to explore the perceived effect of structured neuro-vision education modules on the knowledge and confidence of occupational therapy practitioners (OTPs) to address vision impairment post-strokes. The project used a mixed quantitative and qualitative pretest-posttest design with a small convenience sample of six OTPs working in an inpatient rehabilitation hospital. OTPs were educated on assessment and intervention strategies via educational modules created by the research group in a virtual self-faced format. OTPs who completed the modules reported increased knowledge and confidence in treating persons with neurovision deficits. The study outcomes support additional education to empower OT practitioners to be more knowledgeable and confident in addressing vision deficits in neurological conditions. This conclusion emphasizes the need for continued structured education for OT practitioners in addition to the primary education received in OT programs.
Keywords: Vision, Rehabilitation, Stroke, Educational modules, Confidence
Introduction
Strokes are a prevalent and pressing issue in the United States (US), especially in the southeastern part of the country, also known as the “Stroke Belt,” where there is a higher incidence and mortality rate of strokes [1]. Motor, sensory, visual, and cognitive impairments are all possible effects of a stroke. It has been estimated that over 65% of strokes result in visual impairments [2]. Therefore, neuro-vision assessments and interventions are of particular interest for occupational therapy practitioners (OTPs) within rehabilitation. However, visual impairments are not always assessed, and this could be because some OTPs need additional vision assessment education [2]. An additional research study found that neuro-visual impairments post-stroke impact everyday functioning and emotional well-being, and noted that it is of interest to identify, describe, and integrate rehabilitation interventions to improve patient outcomes [3].
At a comprehensive stroke unit located in an inpatient rehabilitation hospital in Southeast United States, there was no additional education provided for OTPs that treat visual impairments caused by strokes. Without consistent neuro-vision training for OTPs, there was not a consistent, sustainable, and efficient way to implement interventions in a way that most benefitted the patient [4]. The problem was the lack of educational modules for visual impairments post-stroke at the study site, and there were no surveys conducted to elicit feedback from OTPs.
Occupational therapy practitioners that assess visual impairments in addition to physical and cognitive abilities can help patients make significant functional improvements during the first six weeks of therapy [5]. The “Stroke Belt” presents a severe problem; therefore, we aimed to provide neuro-visual impairment educational modules to potentially benefit individuals receiving treatment. The scale of impact of this research was significant because early assessment leads to early intervention, which has a probable impact on general rehabilitation where visual function can be increased [2]. OTPs at this facility had indicated that continued training in treatment of visual impairments in neuro-vision rehab would be beneficial. This study was a preliminary stage to support future research to assess knowledge and confidence in neuro-visual stroke intervention.
The purpose of this mixed-methods study was to examine the perceived effect of educational modules for OTPs to address vision impairment post-stroke at an inpatient rehab facility in southeastern United States. There is significant evidence promoting the effectiveness of continued training programs for OTPs; however, there were limited onsite training resources on visual impairments in stroke at this inpatient facility [4]. Our primary objective was to create educational modules focused on neuro-vision post-stroke. These educational modules would serve as a component to assess the knowledge and confidence of OTPs while focusing on their interest in the materials presented.
It is important for OTPs to accurately assess visual impairments because many activities of daily living (ADLs) require accurate visual information. Research shows that visual impairments can decrease occupational participation and performance in activities such as reading, mobility, driving, etc. [4]. Inaccurate or missing visual fields can create safety concerns, such as fall risks, balance issues, inattention to certain parts of the body, etc. OTPs at this inpatient rehab had acknowledged their lack of time and/or resources to remain current regarding trends related to visual impairments post Stroke.
The expected outcome of this study was that there will be positive experiences regarding the educational modules presented in the approach to treatment for neuro-vision at the study site located in the “Stroke Belt” of the southeastern US. Since neuro-vision is a significant part of the OT scope of practice and 75% of patients in inpatient rehab are there due to neurological deficits, this study would be vital in assisting OTPs in addressing this population and their needs [5].
Review of Related Literature
The literature review was organized into two parts. First, there is an explanation of the chosen conceptual framework of the Person-Environment-Occupation (PEO) model and how it is related to the study. Secondly, a brief review of the three main areas of research is presented and critiqued to further support the study. The first area of research that was critiqued is how strokes affect vision. Next, further investigation of current neuro-vision education for the stroke population for OTPs was conducted. Lastly, current evidence-based visual impairment interventions were researched. This assisted with further understanding the gaps of knowledge on OTPs’ perspectives regarding educational modules. In turn, this helped us to understand the experiences of the OTPs.
PEO Model
The conceptual framework for this study was guided by the Person, Environment, and Occupation (PEO) model which explains the relationship between the person, their environment, and their occupation through the lifespan and how they overlap, also known as occupational performance. The greater the overlap between the person, environment, and occupation, the greater or stronger the occupational performance is [6]. The PEO model, developed by Law et al., is a practical model used by rehabilitation therapists that can be used to conceptualize, plan, communicate and evaluate occupational performance interventions [7]. Our goal was to encourage a good fit between increased occupational performance and overall quality of life. The PEO model guided investigators in the development of educational modules for treating patients with neuro-visual impairments through evaluating the person’s visual abilities and how these affected their environment and their occupations.
Effects of Stroke on Vision
A literature review of the effects of stroke on vision allowed the investigators to examine the impact of stroke on visual impairment. This literature review focused on visual functions such as oculomotor control and visual fields. The analysis provided the investigators with important information to determine the best evidence-based interventions to include in the education modules to treat visual impairments post-stroke.
Vision relies on about 40-50% of the brain [8]. About 5-10% of ischemic strokes cause occipital infarcts that generally do not worsen if there is not a new injury [9]. Cranial nerve lesions, specifically the oculomotor, trochlear, and abducens nerve, account for 6-12% of oculomotor impairments caused by stroke or traumatic brain injury [10]. Hemianopias that are caused by strokes account for 10% permanent visual damage [11]. Visual impairment can sometimes go undetected by the patient because it not only alters the quality and amount of visual input but can also alter how the brain processes and uses incoming visual involvement [10].
Visual field deficits post-stroke, such as hemianopia and scotoma are very common after a stroke [10]. Homonymous hemianopia is the most common visual impairment caused by stroke and is seen in approximately 30-50% of stroke survivors [10]. This can cause issues with arrange of visual input and functional responses such as survivors colliding with people and items in their blind spot due to inability to detect visual stimuli in the contra- lesional visual field which can affect driving [12]. However, this does not seem to extend to survivors with bitemporal hemianopia who have a central range of 110-120 degrees because they meet the minimum eyesight requirements to legally drive in some states of the US [13]. One study about visual field deficits in stroke patients noted that about 10% of the study population returned to driving four weeks after the stroke and 38% began driving after six months of the stroke [14].
Oculomotor visual impairments include diplopia, strabismus, nystagmus, cortical blindness, and accommodative deficiencies, to name a few. According to a study with 512 participants, strabismus occurred in 16.5% of stroke survivors in the study [15]. Injury to the abducens and trochlear nerves are two of the most common causes of diplopia. These oculomotor visual impairments create issues with engaging in activities of daily living (ADLs) such as reading and driving.
Current Neuro-Vision Education
A literature review of current neuron-vision education for stroke patients enabled investigators to assess effective application methods. Additionally, it helped investigators determine a suitable, sustainable, and efficient training program for OTPs employed at the inpatient rehab facility. The following screening tool is an example of a visual impairment assessment that was successfully implemented at a study site. The investigator identified this screening tool as a viable option for possible future use.
Rowe et al. [16] completed a review of a study to evaluate the ‘Vision Impairment Screening Assessment’ (VISA) tool. The purpose of the tool is to assist clinical professionals with identifying visual impairments in stroke survivors. The study presented two alternatives for delivering the screening, (1) the material was printed (VISA print) and a practitioner administered the screening, and (2) the material was provided to the stroke survivor via computer application (VISA app). The mean age of the stroke survivor participants was 70.6 (SD 13.5). Out of 221 male and female screened participants, VISA print was fully completed by (n=101),and (n=100) completed the VISA app. Both VISA versions contain five sections: (1) patient history, (2) visual acuity assessment, (3) movement and eye alignment, (4) assessing visual Fields, (5) visual inattention detection. The VISA print’s sensitivity was 97.67%, and specificity was 66.67%. The VISA apps sensitivity was 88.31%, and the specificity was 86.98%. Sensitivity and specificity indicated the accuracy of the screening tool and validated the acceptable use for screening for visual impairments. This study offered evidence that supported using standardized method of screening for visual problems in stroke survivors. Educating OTPs about validated screening assessments would subsequently benefit the patient by improving the identification of visual impairments [16].
Evidence-Based Interventions
A literature critique of evidence-based interventions allowed the investigators to analyze the most effective intervention and assessment strategies for visual impairments caused by stroke. The information suitable for this study included documented evidence of intervention effectiveness or best practices, patient preferences, and clinical expertise. Hanna et al. [17] did a review study to produce an overview of interventions for adults18 and up (N = 4142) who were experiencing visual impairment post-stroke. Two authors were responsible for gathering and selecting relevant articles to examine the quality of evidence and chance of bias. Forty-nine research articles were collected to study interventions for the following: ocular motility deficits, visual field loss, visual perceptual deficits, and reduced central vision. A mixed-methods design was used to approach the forty-nine included articles, as there was a quantitative and qualitative portion of the examination. This portion assessed bias through one observational study with a questionnaire, along with four additional surveys/questionnaires. One of the articles critiqued within this study was specifically done to investigate current assessments, protocols, referrals, and treatments for visual impairment post-stroke. 45% of OTPs said to begin treatment within 2 weeks of stroke, 75% said to begin treatment within 6 weeks, and 38% said to continue treatment for up to 3 months. Other surveys within the study noted that the most used interventions for unilateral spatial inattentionin OT were perceptual retraining and visual scanning training. OTPs reported that visual inattention was the most common visual impairment treated, along with visual deficits. These interventions involved non-computerized scanning training, ADL training, and the use of aids and/or modifications. Additional ways to compensate for these visual impairments included occlusion and prism adaptation. The study concluded that, overall, there is a need for further randomized controlled trials to dictate how effective the available post-stroke visual impairment interventions are [17].
Method
Research Design
The study used a mixed-method approach with phenomenology as the design strategy. The phenomenon of interest within this study was the OTPs’ experience of usefulness and acceptance of the educational modules on managing visual impairment for stroke patients. Quantitative and qualitative data were collected using pre and post surveys and an electronic exit questionnaire to gather OTPs’ narrative perspectives about the study's effectiveness. Investigators found this research design appropriate to capture the participants’ improvement in knowledge and confidence.
Sampling
Sample selection for this study included a non-probability technique of convenience sampling. The rationale for using convenience sampling stemmed from time constraints, available resources, and affordability. Convenience sampling entailed recruiting as many OTPs as possible from the study site to achieve saturation. The study site was selected based upon a request from the inpatient facility stakeholders for an elaborate post-stroke neuro-vision training program. Participants were selected based on proximity to the investigators, homogeneous location and profession, willingness to participate, and easy accessibility. The key informant (KI), who was currently employed at the study site, recruited all participants from the inpatient facility. Initially, 13 participants completed the consent forms but seven of them did not complete the entirety of the modules and hence were excluded from the project. The study sample included six practitioners (n=6) that completed all aspects of the study. The participants' demographics were: five females and one male, ages ranging from 20-60 years, credentials ranging from Certified Occupational Therapy Assistant to Master of Occupational Therapy, and experience ranging from new graduate to over 20 years of patient care. Participant inclusion criteria were full-time or part time, PRN (pro rate nata/as needed) employment at the inpatient facility and currently licensed as an OT practitioner. The exclusion criteria were employment on other units outside the targeted site and participants who did not read or speak English. The sample size for this study included recruiting as many OTPs from the practitioners working at the study site as possible. Not all OTPs at the study site worked with a stroke population. The justification for this sample size was based on the criteria for OTPs who worked with stroke survivors at the study site and those that were interested in improving their knowledge in caring for stroke patients.
Randomization and Bias Management
A key informant (KI) was responsible for recruiting participants at the study site. The investigators sent an email invitation to participate in the study to the KI, who forwarded it to the target population. To prevent coercion, the KI was asked to limit discussion about the study until after the study's conclusion and to avoid accessing the informant list. The email invitation informed the therapists of the study's purpose and their involvement. Interested OTPs sent an email to a secure email address, requesting more information about the survey and the consent form. Participants were required to sign and return the consent form before receiving the link to the education modules. After completing the consent forms, participants received access to the education modules, and their progress was tracked by using a self-created four-digit identifier and Microsoft Excel codebook.
Instruments/Measures
The primary instruments used in this study were: intervention protocol, Microsoft Excel/Forms for codebook, investigator-created demographic questionnaire, pre- and post-survey, education modules, and an electronic exit questionnaire. Details on each of the measures are provided below.
Intervention Protocol
The intervention protocol was based on Warren’s [18] Hierarchical Model, which is a model used for evaluation and treatment of visual deficits. The Warren Hierarchical Model is based upon a hierarchy of skills where lower-level basic skills, such as visual functions, are first acquired and then higher-level skills, such as visual processes, can be later acquired [18]. In utilizing this model in practice, OTPs are recommended to use a bottom-up approach during evaluation and treatment of first acquiring lower-level skills to allow development of higher-level skills [18]. Additionally, the protocol includes information about types of visual impairments such as diplopia, convergence impairment, oculomotor deficits, saccades, accommodative disorders, visual field impairments, etc., and guidelines on how to treat post-stroke visual impairments.
Demographic Questionnaire, Pre-and-Post Survey
Investigators self-created and utilized a demographic questionnaire and a pre-and post-survey where the OTPs were given questions using a five-point Likert scale to capture their knowledge and confidence about neuro-vision before and after completing the educational modules. Some examples of questions that were asked in the pre-post survey were: I feel confident in my ability to select appropriate occupational therapy assessments to complete without seeking help from others, I believe I have the knowledge to implement occupational therapy interventions with patients that have neurological vision impairments, I feel confident in my ability to provide therapeutic interventions to patients with neurological vision impairments. Investigators utilized a Microsoft Excel codebook to track participant progress and to organize demographic information.
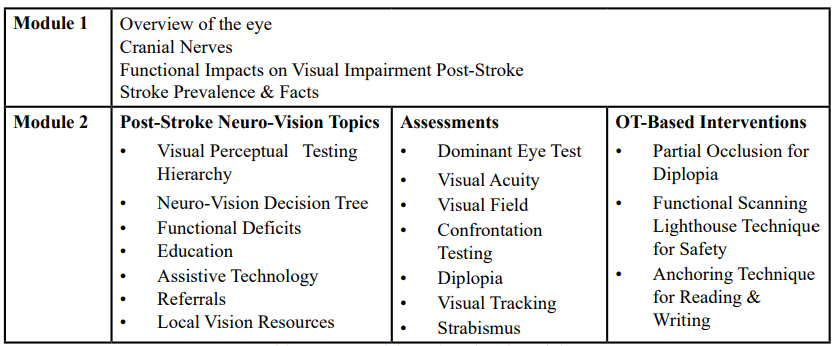
Education Modules
Microsoft Power Point was used to create the two educational modules. Videos and voice overs were self-created and incorporated into the Power Point slides. The Brain Injury Visual Assessment Battery for Adults (BIVABA), consultation with certified OT vision specialists, evidence-based practice research reviews, and feedback from experienced OTPs were utilized to create the educational modules. To assess learned and retained knowledge, the investigators included quizzes that had multiple-choice, true/false, and matching questions in the modules. The questions were self-administered virtually by the participants after watching the videos. The correct answers to the educational module quizzes were provided to the participants at the end of each module. The topics included in the education modules are depicted in Table 1.
Electronic Exit Questionnaire
Investigators utilized a self-created electronic exit questionnaire where the OTPs were given open-ended questions to share their experiences. Some examples of questions that were asked in the electronic exit questionnaire were: what was your experience while participating in the education modules, what are your thoughts about participating in the module overall, do you feel that the completion of the educational module will help with future interventions, and are there any areas of improvement for the module. A final question welcoming any open comments that the participants may have also was included in the electronic exit questionnaire.
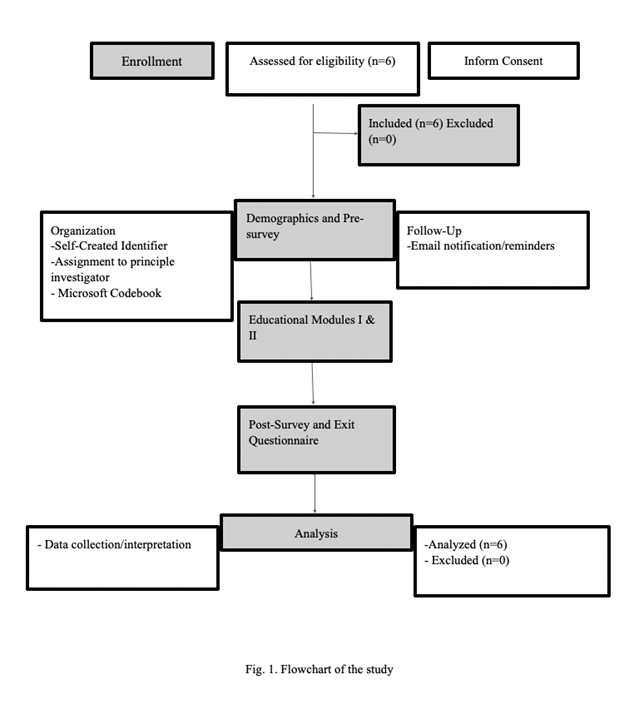
Procedures/Data Collection
Institutional Review Board (IRB) approval was received from the investigators’ institution and a permission letter was obtained from the site facility. An email invite was sent to the key informant at the site who forwarded that email to all OTPs working at the site. After receiving the email invitation, interested OTPs had two weeks to contact the investigators to request, sign, and return the signed consent form. Participation in the study was voluntary, and education modules could be completed at times convenient to the participants. The setting of the study was a virtual environment. After receiving the signed consent, the investigators sent the two educational modules and exit questionnaire to the participants. The study participants had three weeks to complete the educational modules and exit questionnaire. The investigators monitored the completion rates and emailed reminders to individual participants who had not started or finished the modules and/or exit questionnaires within 2-3 weeks after receiving the consent form. Once the modules and exit questionnaire were completed, the participants’ contribution to the study was concluded. Data was collected online from the study site and retrieved from an encrypted secure online cloud. The procedures and data collection of the study lasted two months from September 2022 to November 2022. See Figure 1 for flowchart of the study.
Data Analysis
Quantitative analysis of pretest and posttest surveys was completed using Microsoft Excel® version 2016 data analysis tools to compute the percentage of change in pretest and posttest results. Comparative analysis of pretest and posttest participants' surveys were completed. Demographic responses were analyzed using descriptive statistics. Qualitative analysis was completed using inductive content analysis and Microsoft Excel® version 2016 was used as the code book to highlight major concepts and ideas being conveyed. The resulting concepts were continually reviewed and grouped together to identify common themes related to the study question. Redundant or recurring information was eliminated. Participants’ information was coded using a standard numbering method to identify respondents uniquely. Information collected from the pre- and posttest surveys were compared to determine if there were any significant changes in participants’ perceived knowledge and confidence after completing the education modules. The qualitative survey was utilized to identify common themes, determine what participants found helpful, and areas for future improvement.
Results
Quantitative Data Analysis
Quantitative data was collected via the investigator created pretest and posttest survey using a 5-point Likert scale to measure participants’ self-ratings. Participating practitioners were provided with six statements related to confidence and knowledge in treating post-stroke visual impairments and were instructed to rate each statement based on the level of perceived agreement on a scale of 1-5. 1= strongly disagree and 5= strongly agree. Participants were provided with these statements both before and after the completion of educational modules (pre- and post-survey) (see Appendix A). The structure of the pre- and post-surveys aimed at gathering information to answer the study’s two research questions were as below:
Research question #1: What is the current knowledge and confidence of OT practitioners in treating post-stroke visual impairments?
The pre-survey mean between all participants and level of agreement for all 6 questions combined was 3.16, meaning participants were between “neutral” and “somewhat agree” regarding statements about having knowledge and confidence when treating patients experiencing visual impairments post-stroke.
Research question #2: What was the practitioners’ perceived experience after the completion of the educational modules?
The post-survey mean between all participants and level of agreement for all 6 questions combined was 4.15, meaning the participants were now between “somewhat agree” and “strongly agree” with statements about perceived knowledge and confidence in treating post-stroke visual impairments. All participating practitioners perceived a combined mean increase (32%) in knowledge and confidence after completing the educational modules, indicating the purpose of the research study was met. Participants had the largest mean perceived increase (44.4%) in statements regarding the knowledge to implement assessments and confidence to provide interventions for patients with neuro-vision impairments (Appendix D). Overall, the results supported our research hypothesis that participating practitioners would perceive an increase in confidence and knowledge to effectively treat post-stroke visual impairments. Research question #2 was also measured with qualitative responses.
Qualitative Data Analysis
Qualitative responses were obtained from the exit questionnaire created by the investigators. Content data analysis was utilized to analyze the data, which was chosen due to the small sample size. Once data was successfully collected with Microsoft Forms, student investigators exported the information to a Microsoft Excel document to create a codebook. The responses were organized and coded in Microsoft Excel by all the investigators separately and then reviewed as a group for accuracy and agreement on themes. The qualitative data analysis process included highlighting the major concepts and ideas being conveyed. The resulting concepts were continually reviewed and grouped together until saturation occurred to form themes related to the study question. Redundant or recurring information was eliminated. Each investigator selected several common themes for each question. Investigators then combined the common themes for each question and discussed themes until reaching saturation (Appendix E).
Perception and Description of Participation in Educational Modules
Participants were asked to provide their thoughts about participating in the education modules. Many of them described their experience as a good review to help maintain skills. Participant 6 stated; “ I appreciate the detail and breakdown on topics.” For this question, investigators discussed several themes but settled on informative, good review, and pertinent as the most common themes.
Participants described their experience during the modules with phrases and terms such as: appreciating the flow of the material, information was presented well, and participant 3 remarked that it was “thorough information without being busy.” Participant 6 commented that the information was “presented with creativity.” From these remarks, we identified the common themes as organized and creative.
Perception of Effects on Future Interventions
Participants felt that the educational modules would improve their intervention approach in the future. They explained that the modules helped them by providing them with a “basic toolkit (participant 3),” “hospital/home environment intervention examples, and good resources for ideas (participant 7).” Participant 6 stated: “ I liked the newly introduced intervention ideas”. Therefore, common themes for this section were evidence-based and great intervention ideas.
Educational Module Improvement Suggestions
Participants shared areas of improvement for the modules. They noted that handouts would be beneficial for clinical use. One participant felt more interactive components would have been helpful but due to the nature of the questionnaire, investigators couldn’t probe more for a better understanding of this statement. The common themes identified were lack of handouts for clinical use and limited interaction. Participants were then offered the opportunity to share any other comments or suggestions where they expressed, they felt it was easy to participate. Others felt that two separate modules for interventions instead of one and immediate access to all sections would have been more helpful.
Common Themes
The most common themes identified were informative, evidence-based, and organized. Participants identified the educational modules as “informative” in several responses related to areas such as future interventions and perception of participation. While the term “evidence-based” wasn’t used explicitly it was inferred from the language used when participants described the perception of the effects on their future intervention. Additionally, “organized” was a recurrent sentiment when participants provided comments for descriptions of participation in educational modules.
Discussion and Conclusion
Quantitative results indicated that the educational modules were perceived as a positive experience as they helped improve knowledge and confidence of the OTPs that participated in the study. Additionally, the participants felt that by improving visual function, they could further improve their patients’ occupational engagement and safety upon discharge. The Likert style Knowledge and Confidence questionnaire reflected improved scores post intervention. The pre-evaluation scores ranged from 3.0-3.35 and the post evaluation scores were between 3.83-4.33, indicating a 32% average improvement in feelings of knowledge and confidence. The study results show that overall knowledge of the OTPs increased, and they became more confident in providing neuro-vision interventions due to the education provided. The results of this study correspond with the study by Rowe et al. [16], which states that educating OTPs about validated screening assessments would subsequently benefit the patient by improving the identification of visual impairments.
Qualitative themes that emerged included improved knowledge and confidence in providing vision care to stroke clients. Additionally, participants appreciated the information format of embedded videos and creatively organized material. Participants’ qualitative responses were positive and indicated the education modules were beneficial to them and would serve as a resource for future use. The positive qualitative themes support this project’s focused question that education can help participants in improving their knowledge and confidence in treating difficult issues such as neuro-vision further improving patient outcomes. Both quantitative data and qualitative themes support the focused question in that neuro-vision education benefits both the participants and the clients they treat. In conclusion, the qualitative and quantitative data indicated that the educational modules improved the occupational therapy practitioners' knowledge and confidence in treating visual impairment post-stroke.
Implications for occupational therapy practice
According to the American Stroke Association (ASA), over 65% of stroke survivors access rehabilitation services in the United States. As a result, OTPs working in rehabilitation centers can treat a lot of people with a stroke [19]. In addition to muscle weakness, sensory issues, and cognitive problems, these patients can have visual impairments too. These impairments can affect their activities of daily living (ADLs) and instrumental activities of daily living (IADLs) such as walking, reading, and driving. OTPs receive primary education in visual assessments and interventions as part of their coursework, but this is not enough to manage complex issues that may arise after a stroke. Evidence-based educational modules such as the ones provided in this study can assist OTPs in gaining that extra knowledge and increasing their confidence in utilizing evidence supported assessments and interventions. Early identification of visual impairments may lead to appropriate assessments and interventions to be used soon in the recovery process improving safety and function and thus reducing burden on caregivers.
Study Limitations
Several limitations exist in this study. First was the small sample size (n=6) which decreases the ability to generalize the results to the wider population. Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. Data saturation was not reached due to the limited number of participants. Convenience sampling was used so participants had some innate motivation when they started the education modules. Second, continued COVID-19 related limitations such as a virtual format, busy practitioners, and burnout limited the number of participants that completed the study. Additionally, one participant cited communication and technology difficulties in accessing the videos. Finally, one of the outcome tools was developed by the study investigators. While steps were taken to utilize the best available literature to create this survey, the tool was not standardized and had limited validity.
Future Research
Future research should be followed with the study group to assess retained knowledge and confidence 1-year post-program implementation. Additionally, future research should be completed with a larger sample size in several different hospitals in additional geographic locations. By enlarging the sample size, we would be able to better assess the perceived increase in knowledge and confidence for additional OTPs. Furthermore, we would be able to provide more OTPs with our educational modules to increase their clinical skills and thus improve patient outcomes.
Acknowledgements:
We thank all the occupational therapy participants in this study for their time, support, and cooperation, without which this study would not have been possible. We also thank Brandon Wolf, Catherine Coats, Lashara Barnes, and Camille Crabtree for their support in creating the modules and collecting data while they were MSOT students at Winston-Salem State University.
Declaration of interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information:
Notes on contributors:
Dr. Sanchala K. Sen, OTD, MS, OTR/L, BCPR. FAOTA is an assistant professor in the department of occupational therapy at Winston-Salem State University, North Carolina, United States.
Jennifer Worischeck, OTR/L is a registered occupational therapist working in acute care. She was a graduate student at Winston-Salem State University, Winston-Salem, North Carolina, USA, at the time of this study. This study was completed as partial fulfillment of her degree.
References
Howard, G., & Howard, V. J. (2020). Twenty years of progress toward understanding the stroke belt. Stroke, 51(3), 742–750. View
Rowe, F., Hepworth, L., Howard, C., Hanna, K., Cheyne, C., & Currie, J. (2019). High incidence prevalence of visual problems after acute stroke: An epidemiology study withimplications for service delivery. PLoS ONE, 14(3), 1-16. View
Norup, A., Guldberg, A., Radmer-Friis, C., Deurell, E. M., & Forchhammer, H. B. (2016). An interdisciplinary visual team in an acute and sub-acute stroke unit: Providing assessment and early rehabilitation. Neuro Rehabilitation, 39(3), 451–461. View
Falkenberg, H. K., Mathisen, T. S., Ormstad, H., & Eilertsen, G. (2020). "Invisible" visual impairments: A qualitative study of stroke survivors` experience of vision symptoms, health services and impact of visual impairments. BMC Health Services Research, 20(302), 2-12. View
Hillier, R., & Tarbutton, N. M. (2014). Vision deficits following stroke implications for occupational therapy practice. OT Practice, 19(21), 13-16.
Rigby, P., Trentham, B., & Letts, L. (2019). Modifying performance contexts. In B.A.B. Schell & Gillen (Eds.), Willard & Spackman’s occupational therapy (13th ed., pp. 460-479). Wolters Kluwer. View
Law, M., Cooper, B., Strong, S., Stewart, D., Rigby, P., Letts, L., (1996). The person-environment-occupation model: a transactive approach to occupational performance. Can J Occup Ther. 63:9–23.View
Lighthill, C. R., Perez, E. E., & McWilliams, K. B. (2013). Coming into focus: Brain injury and vision therapy. Rehab Management, 26(9), 20–23.
Frolov, A., Feuerstein, J., & Subramania, P. (2017). Homonymous hemianopia and vision restoration therapy. Neurologic Clinics, 35(1), 29-43. View
Warren, M. (2018). Evaluation and treatment of visual deficits after brain injury. In H. Pendleton& W. Schultz-Krohn (Eds.), Pedretti’s occupational therapy practice skills for physicaldys function (8th ed., pp. 594-631). Elsevier.
Perea, J. D., & Anise, M. C. (2019). Beyond cueing to the left and a red line: Treatment methodsfor homonymous hemianopia. SIS Quarterly Practice Connections, 4(2), 28–30. View
Perez, C., & Chokron, S. (2014). Rehabilitation of homonymous hemianopia: Insight into blindsight. Frontiers in Integrative Neuroscience. 8(82). View
Peli, E., & Satgunam, P. (2014). Bitemporal hemianopia; its unique binocular complexities and a novel remedy. Ophthalmic and Physiological Optics, 34(2), 233-242. View
Dalen, I., Hoff, J., Midelfart, A., Næss, H., Rødahl, E., Sand, M., Tharaldsen, R., Thomassen, L., & Wilhelmsen, G. (2020). Vision-related quality of life in patients with occipital stroke. Acta Neurologica Scandinavia, 141 (6), 509-518.
Iliescu, D., Timaru, C., Alexe, N., Gosav, E., De Simone, A., Batras, M., & Stefan, C. (2017). Management of diplopia. Romanian Journal of Ophthalmology, 61(3), 166-170. View
Rowe, F. J., Hepworth, L., Howard, C., Bruce, A., Smerdon, V., Payne, T., & Burnside, G. (2020). Vision Screening Assessment (VISA) tool: Diagnostic accuracy validation of a novel screening tool in detecting visual impairment among stroke survivors. BMJ Open, 10(6), 1-9. View
Hanna, K. L., Hepworth, L. R., & Rowe, F. J. (2017). The treatment methods for post-stroke visual impairment: A systematic review. Brain and Behavior, 7(5), 2-26. View
Warren, M. (1993). A hierarchical model for evaluation and treatment of visual perceptual dysfunction in adult acquired brain injury, part 1. American Journal of Occupational Therapy, 47(1), 42-54. View
American Stroke Association. (n.d.). Stroke rehab. View