Journal of Rehabilitation Practices and Research Volume 6 (2025), Article ID: JRPR-183
https://doi.org/10.33790/jrpr1100183Research Article
Reducing Musculoskeletal Disorders in Dental Students Through Ergonomic Education: A Randomized Intervention Study
Carissa Armijo, OTD, OTR/L, Alejandra Villagomez, OTD, OTR/L, Lisa Knecht-Sabres*, DHS, OTR/L, Linda Sangalli, DDS, MS, PhD, Charlotte Bolch, Ph.D., M.S., Dana Lingle, OTD, OTR/L, CHT, Melisa F. Alabsy, DDS, MHA,
Department of Occupational Therapy, Midwestern University, Downers Grove, IL 60515, United States.
Corresponding Author Details: Lisa Knecht-Sabres, DHS, OTR/L, Professor, Department of Occupational Therapy, Midwestern University, 555 31st Street, Downers Grove, IL 60515, United States.
Received date: 01st July, 2025
Accepted date: 23rd September, 2025
Published date: 25th September, 2025
Citation: Armijo, C., Villagomez, A., Knecht-Sabres, L., Sangalli, L., Bolch, C., Lingle, D., & Alabsy, M. F., (2025). Reducing Musculoskeletal Disorders in Dental Students Through Ergonomic Education: A Randomized Intervention Study. J Rehab Pract Res, 6(2):183.
Copyright: ©2025, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Even though there is abundant evidence illustrating high occurrence of musculoskeletal disorders (MSDs) among dental students and professionals, there is limited evidence regarding the most efficient and effective ways to prevent these injuries.
Objective: This study examined the effectiveness of an ergonomic intervention program on the reduction of self-reported pain and MSD symptoms among dental students.
Methods: A randomized control study with a pre/post-test design was used to examine the outcomes of a 10-week ergonomic intervention program offered to the second-year dental students (n=140). Effectiveness of the intervention was measured by the comparison of pre and post-test scores on two measures: (1) the Modified Nordic Musculoskeletal Questionnaire (M-NMQ) and (2) a Researcher-Developed Questionnaire investigating application of ergonomic principles and perceived benefits.
Results: Results demonstrated the benefits of a 10-week intervention program. For example, after the intervention, only 7.4% of participants in the intervention group reported musculoskeletal pain affecting activities outside of the dental lab; whereas, 35% of the control group participants reported the presence of musculoskeletal pain affecting activities outside of the dental lab. Likewise, at the end of the study, only 13% of the intervention group, yet 25% of the control group, reported being in an awkward position over 50% of the time while working in the dental lab. Statistical differences were also found for reports of shoulder and knee pain among the two groups.
Conclusion: This study revealed that a 10-week ergonomic intervention program has the potential to improve the application of ergonomic principles, increase the implementation of routine breaks and stretches during dental simulation clinic sessions and decrease the presence of musculoskeletal pain and dysfunction.
Introduction
Research has revealed that over 85% of dental students report having at least one musculoskeletal disorder (MSDs) [1,2]. Moreover, 70-88% of dental students have conveyed the presence of musculoskeletal pain [3,4]. Musculoskeletal pain is defined as pain that affects bones, joints, ligaments, muscles, and tendons [5]. Unfortunately, reports of MSDs and bodily pain are not limited to dental students and can continue to be problematic for dental professionals throughout their careers. For example, Partido & Wright [6] discovered that approximately 62-91% of dental professionals experience MSDs. Moreover, musculoskeletal pain in dental professionals has resulted in a decreased ability to work in clinical practice [7]. Unfortunately, MSDs not only limit one’s ability to work but can interfere with one’s ability to engage in meaningful activities, leading to various psychosocial concerns and decreased quality of life [8].
One of the major reasons why dental students and professionals are particularly prone to work-related MSDs is due to the specific demands of their job. For example, dental students and professionals need to maintain static working positions for prolonged periods of time [9,10]. Other causes of MSDs among dental students and professionals have been linked to their forceful and repetitive motions, poorly designed instruments, the amount of precision required during dental procedures, the stress associated with the profession, and the lack of breaks and stretching throughout the workday [9-13]. The most common areas for pain among dentists, dental students, and other dental professionals are the neck, shoulders, back, and hands [1,14-16].
Ergonomics is the science of fitting workplace conditions and job demands to the capabilities of the working population [17]. Ergonomics can ensure high productivity, avoidance of illness and injury risks, and increased satisfaction in the workplace [17]. Since MSDs and pain have been identified to occur early in the dental education process, researchers have asserted that it is imperative to enhance education and awareness regarding poor body mechanics and the implementation of proper ergonomic principles during dental school and before faulty postural habits are developed [1,6-7,12, 16,18-20]. However, even though there is abundant evidence that illustrates the high occurrence of MSDs among dental professionals, the current literature suggests that dental students have limited awareness regarding ergonomics [21]. Moreover, there is currently limited evidence regarding the most efficient and effective way to prevent these injuries [9]. However, proper positioning of the body and dental equipment allows for a neutral working posture and has been shown to aid in minimizing postural deviation and muscular strain [16,22,23]. Likewise, frequent breaks and stretching exercises that reverse the person’s common positions at work have been identified as an integral piece of an effective prevention program, in addition to increasing productivity and enhancing career longevity [16,22].
Unfortunately, some studies have revealed that even though dental students may understand and be knowledgeable regarding proper ergonomics, they lacked the implementation of this information [24]. Conversely, there is some evidence to suggest that the use of feedback involving photography has been shown to improve the implementation of proper ergonomic principles [7]. Thus, Garbin et al. used photographic analysis to facilitate the students’ self- reflection regarding compliance/non-compliance with ergonomic postures and to help prevent and/or minimize the presence of MSDs among dental students and professionals [24]. That is, they asserted that identifying postural inadequacies and identifying methods to enhance compliance with proper body mechanics may help prevent and/or minimize the presence of MSDs among dental students and professionals [24]. More importantly, Roll et al [12] revealed that increased postural awareness in the dental simulation clinic contributed to a lower risk of musculoskeletal pain, symptoms, and disorders. Additionally, researchers have asserted that alternative modalities include the use of visual reminders, such as photographs of proper ergonomics and reminders to stretch throughout dental labs and procedures, as well as individualized feedback may be beneficial in adopting appropriate ergonomic postures and principles [25].
Ergonomics is within the professional domain of occupational therapy. Since occupational therapy practitioners (OTPs) are skilled at evaluating, adapting, and modifying work task performance and the environment to enhance overall ergonomics and safety, OTPs can be valuable in providing a preventative approach to reducing MSDs among dental professionals [26]. Additionally, OTPs trained in ergonomics have expertise in being able to address the barriers to implementing ergonomic techniques and are able to evaluate the effectiveness of the suggested interventions [26].
Since MSDs are highly prevalent in dental students and there is limited evidence regarding the most effective and efficient methods to address these concerns, the aim of this study was to examine if a ten-week ergonomic intervention program leads to a decrease in self reported pain and MSDs among second-year dental students enrolled in a dental program in the Midwest. Second year dental students were specifically chosen for this study because these students had already received 2 hours of lectures on ergonomics and had received a 30-minute demonstration in the Preclinical Simulation Clinic where an OT faculty member with an expertise in ergonomics reviewed core concepts in ergonomics, appropriate positioning, common detrimental habits, as well as a demonstration of stretching exercises. After the 30-minute encounter, the students were also provided with a pictorial handout for future reference. Second year dental students were also specifically chosen for this study since it was at this point in their educational program that they would start to participate in numerous laboratory activities in the SIM lab, with the ultimate goal of promoting awareness and solid postural habits at an early stage of the students’ dental career.
Thus, the specific aim of this study was to examine the effectiveness of a 10-week ergonomic intervention program on the reduction of self-reported pain and MSD symptoms among second year dental students. More specifically, this study investigated if the use of visual reminders to implement proper body mechanics and regular stretching, located at their laboratory workstation, had an impact on self-reported pain and MSD symptoms among second year dental students. Additionally, the researchers examined if individualized feedback using photo images of instances when students were not implementing proper ergonomic principles had an impact on self-reported pain and MSD symptoms among second year dental students.
Methods
Research Design
This exploratory study used a pre-post-test design to investigate the benefits of the proposed ten-week ergonomic intervention program with participants randomized to control or intervention groups.
Participants
140 second-year dental students enrolled in a Dental Program in the Midwest during the Fall 2023 and Winter 2023 terms were recruited for this study. The only criteria for inclusion in this study was being a second-year dental student at the university. Seventy participants were randomly assigned to the intervention group, and the other seventy participants were randomly assigned to the control group. That is, students assigned to lab station numbers 1-70 were placed in the intervention group and students assigned to lab station numbers 71-140 were assigned to the control group. Numerous steps were taken to minimize any potential perception of coercion. For example, this research project was introduced to dental students by OT faculty and OT researchers who were not involved in the students’ grading. Secondly, it was made explicitly clear that: participation is completely voluntary; all information would be kept confidential; dental faculty responsible for grading their laboratory work would have no knowledge regarding their decision to participate/decline participation in this study; and were informed of their right to discontinue at any time, for any reason, without any consequences. Additionally, to help minimize any feelings of awkwardness or pressure to fill in the RedCap surveys, when students are asked to fill out the RedCap survey on their phones/laptops at the beginning of the class, the OT researchers introducing the study to the dental students made an announcement indicating that if any student does not want to participate in the study and/or fill out the survey, that they can use their phones/laptops to search the web, engage in social media, etc. while their peers are filling out the survey. The anonymity of the participants was maintained throughout the data collection and data analysis process.
Measures
Quantitative data was collected through two measures: (1) the Modified Nordic Musculoskeletal Questionnaire (M-NMQ) and (2) a Researcher-Developed Questionnaire, which were both administered and stored via Research Electronic Data Capture (REDCapTM), a secure online software developed for research purposes.
The Modified Nordic Musculoskeletal Questionnaire (M-NMQ). The Modified Nordic Musculoskeletal Questionnaire (M-NMQ) is a well-known, public domain, and highly used questionnaire that assesses reports of musculoskeletal symptoms, pain, and MSDs [27]. The M-NMQ is a 27-item questionnaire containing yes/no questions about any aches, pain, discomfort, and/or numbness in various parts of the body within the last 12 months. It also asks if any of the above-mentioned symptoms have prevented them from doing normal everyday work within the last 12 months and if they have had any trouble at any time within the last 7 days. The M-NMQ includes basic demographic questions such as gender, age, height, and weight. It adapts the original Nordic Musculoskeletal Questionnaire (NMQ) by providing more detailed, region-specific questions about pain and numbness.
Researcher-Developed Questionnaire. The researchers of this study gathered additional data through a researcher-developed questionnaire to obtain supplementary information regarding complaints of pain, the practical application of proper ergonomic principles within the dental simulation clinic, and the participant’s perceived benefits and value of the intervention strategies used in the study. The Researcher-Developed Questionnaires were informed by the literature and modified according to expert opinion. Expert opinion was provided by three professors with an extensive background in research, an occupational therapist with an extensive background in ergonomics, and three professors with extensive experience in dental education. The researcher-developed pre-test questionnaire consisted of 9 closed-ended questions and 1 open--ended question (Appendix A). The researcher-developed post-test questionnaires contained additional questions to gather feedback and additional data regarding the perceived benefits and perceived value of the intervention strategies used in this study (Appendix B). Most of the questions on this survey were Likert-type items with answers on a 5-point assessment scale (e.g., 1 = not valuable at all; 2 = somewhat valuable; 3 = neutral; 4 = very valuable; and 5 = extremely valuable.) In addition, self-perceived pain intensity was investigated on both the pre-test and post-test on a 11-point scale, with 0 = no pain and 10 = extreme pain.
Procedure
Approval was obtained from the University’s Institutional Review Board before the study procedures began (#23027). The researchers informed all second-year dental students that participation was completely voluntary, that all information would be kept confidential, and of their right to discontinue at any time, for any reason, without any consequences. The researchers answered any and all questions before the participants were asked to provide consent and before any data was collected. If a participant decided not to participate after reviewing the study information, they were excused from the study, shown gratitude for their interest, and assured that no consequences would occur for their desire not to participate. 3 students in the experimental group declined to have individual and verbal feedback related to their implementation of ergonomic principles in the dental lab.
The first step of the intervention for all second-year students was to review ergonomic principles and content which was presented in a lecture format to the dental students by an OT professor in the students’ previous quarter of their didactic and laboratory education. More specifically, the OT researchers reviewed key concepts about proper positioning of the student, proper positioning of the mannequin, and proper positioning of the instruments, equipment, materials and work environment. The researchers reviewed previously taught ergonomic principles to all second-year dental students at the beginning of their lab and reinforced their usage by placing photographs of the recommended ergonomic principles unobtrusively at each of the students’ workstations which served as a visual reminder to implement proper ergonomic principles during their clinical laboratory experiences. In addition to the photos related to proper ergonomic principles, the researchers also reviewed previously taught and recommended stretching exercises and reminded the dental students of the importance of implementing these stretches during their clinical laboratory experiences. To reinforce the implementation of stretching exercises within the dental laboratory, the OT researchers placed photographs of the recommended stretching exercises at each student’s workstation, as a visual reminder to implement stretches throughout their clinical laboratory days. All OT researchers either had an expertise in ergonomics or were calibrated by an OT ergonomic specialist in the application of ergonomics in the dental laboratory as it relates to the position of the student, as well as the position of tools, instruments, and mannequins in the environment. All OT researchers demonstrated a high level of agreement on various observations in the dental lab, including scoring of the Rapid Upper Limb Assessment, before the onset of this research project.
Additionally, for the dental students randomly assigned to the intervention group (n=70), the researchers took several photos of when they were not implementing proper ergonomic principles during their laboratory activities. Immediately after, the researchers then reviewed the photo individually with the corresponding dental student and educated them on the appropriate strategies to improve their application of proper ergonomic principles while performing their activities in the dental lab. The researchers observed the students on a consistent laboratory day and time, every week, over a 10-week period of time. The researchers took 3 photos per student in the intervention group over a 10-week timeframe and strived to take these photos and provide immediate and individualized one on one feedback for each student approximately every 3 weeks. The individualized and one on one feedback was based on noncompliance to recommended dental ergonomic principles based on the current literature [3-7,9,16,18,25] which was consistent with the material that was presented to the students as part of their dental education prior to this research study, as the evidence suggested that noncompliance to recommended dental ergonomic principles could be related to the position of the student or the position of items in the environment (e.g., position of tools, instruments, chair, mannequin, etc.). More specifically, the researchers took a photo which depicted noncompliance of a particular student, showed the student the photo, and asked the student if they could identify how they were noncompliant. If the student could not identify the concern/at risk behavior, the researcher raised awareness of the noncompliant concern. In either case, the researcher educated the student participant regarding how they could enhance implementation of recommended ergonomic principles.
All photos were taken by the researchers and were deleted on the researchers’ phones on the same day that the photo was taken and immediately after the respective student participant received feedback regarding the photo which depicted non-compliance with proper ergonomics. If the student participant wanted to keep a copy of the photo, the researchers texted or emailed the photo to the respective dental student, but the researchers did not save any of the photos, emails, or text messages, per IRB approval. For ethical reasons, interventions for the control group (individualized visual and verbal feedback) were offered after the completion of all data collection.
Data Analysis
Descriptive statistics were used to examine the pre and post-test data and to determine if there were changes from baseline to after the end of the 10-week intervention program. More specifically, the Yes/No and Likert-type questions were analyzed with descriptive statistics and reported in terms of counts and percentages. Variables of interests were reviewed for missing data, which were handled as being missing at random (MAR) and managed through case-wise deletion. No imputation methods were used to account for missing data. Given the data limitations with not being able to link pre-test results to post-test results, analysis of post-test results were compared between the control vs. intervention group using Chi-square tests to assess any potential relationships between the groups on each of the M-NMQ questions. The assumptions of a Chi-square test were met which included that the data had categorical variables with frequencies, observations were all independent, the categories of the variables were mutually exclusive, and the expected cell counts were generally 5 or greater. The missing data of participant pre- and post- survey responses was limited to only about 3 participants from the control group not responding to a few of the questions on the NMQ towards the end of the questionnaire. Therefore, as much participant data was retained as possible with missing responses removed for just the analysis of those individual questions between the control and intervention groups. Effect sizes were also calculated for the Chi-square tests to quantify the strength of the association between the two categorical variables (intervention/control and the pain questionnaire questions for each limb). Phi effect size was calculated for all analyses with a 2x2 contingency table and Cramer’s V effect size was used for all contingency tables greater than 2x2. Significance level was set at p-value < 0.05 and all tests were conducted in the statistical software R, version 4.4.1.
The open-ended questions on the researcher developed questionnaires were analyzed for common themes. Thematic data analysis is a qualitative approach which identifies patterns and similar themes across participants allowing meaning to emerge from the data [28,29,30]. More specifically, the researchers individually immersed themselves in the data by “repeated reading” to gain familiarity and to begin to find patterns [28,29,30]. Data analysis meetings with all researchers were used to identify patterns, reduce and group data, and identify themes. The researchers followed the six steps of the recommended systematic thematic analysis process: (1) transcript creation and data familiarization; (2) keyword identification; (3) code selection; (4) theme development; (5) conceptualization through the interpretation of keywords, codes, and themes; and (6) development of a conceptual model [28,29,30]. With this approach, in order to reduce bias and enhance rigor, each researcher read the qualitative data independently and then came together, after individually completing these steps, to collaborate and conceptualize interpretation of key words, codes, and themes. This process was repeated until consensus was achieved. Peer debriefing, member checking and expert examination were used throughout the data analysis process. As a result, trustworthiness of data was enhanced through individual coding, peer review, and expert examination.
Results
Intervention Group
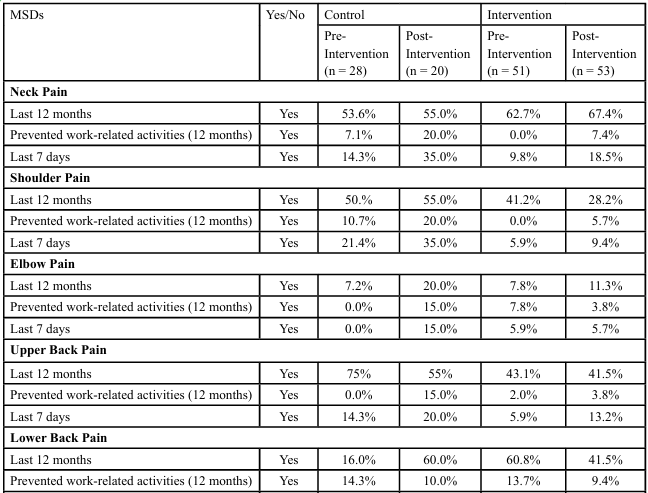
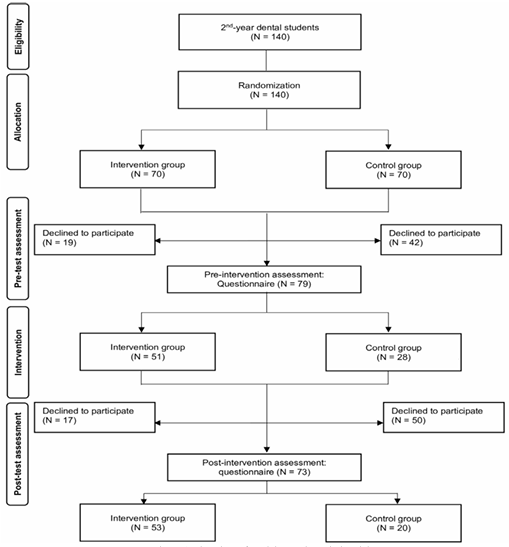
51 out of 70 participants in the intervention group (73%) completed the pre-test survey and 53 out of 70 (76%) completed the post survey. The scores of the intervention group’s pre- and post-survey are shown in Table 1. Figure 1 shows the flowchart of study participants.
Modified Nordic Musculoskeletal Questionnaire Results
Table 1 shows the site of musculoskeletal pain in the last 12 months, if the site of pain prevented participants from performing work related activities in the last 12 months, and if they experienced pain in the last 7 days (as reported by the participants in the intervention group). The results from the pre and post-test scores in the intervention group revealed that: the participants in the intervention group: (1) had decreased reports of musculoskeletal pain that affected their occupations/activities outside of the simulation clinic and (2) reported less pain in their neck, shoulders, wrists and hands.
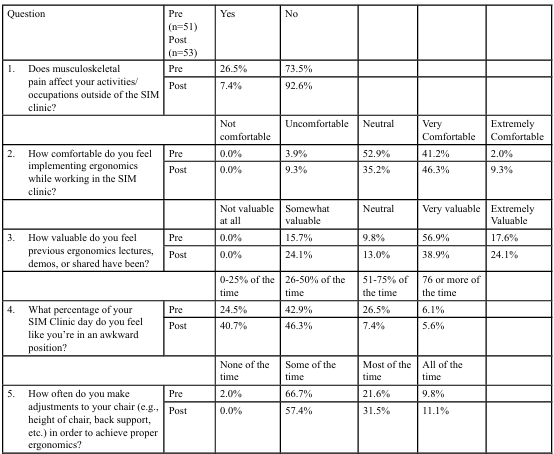
Researcher Questionnaire Results
Table 2 shows the results of the Researcher Questions regarding how comfortable the participants felt implementing ergonomics, how MSD pain affected activities in the simulation clinic, if previous lectures regarding ergonomics were valuable, how comfortable they were in making adjustments to their workstation and chair, how mindful they were of taking breaks, and how often they implemented stretching at their bench pre and post intervention. The results from the pre and post-test scores for the intervention group on the Researcher Questionnaire revealed the following findings: the participants in the intervention group: (1) felt more comfortable implementing ergonomic principles; (2) reported being in an awkward position less of the time; (3) made more frequent adjustments to their work stations to implement proper ergonomic principles; (4) reported that having pictures at their workstation which depicted proper ergonomics helped them be more mindful/facilitated implementing recommended stretches throughout their workday; and (5) felt that individualized photos and feedback were very valuable/ helpful to apply ergonomic principles efficiently. When asked about their recommendations to help them better implement proper ergonomics throughout their dental school program, suggestions included the following: more faculty involvement in taking breaks, stretching, and applying ergonomic principles; more pictures/images and demonstrations related to stretches and application of proper ergonomics; more education/lectures/lab on ergonomic principles; and more regular follow-ups.
Control Group
28 out of 70 (40%) participants in the control group completed the pre-intervention survey and 20 out 70 (28%) completed the post intervention survey. The scores of the control group’s pre- and post surveys are shown in Table 1.
Modified Nordic Questionnaire Results
Table 1 shows the site of musculoskeletal pain in the last 12 months, if the site of pain prevented participants from performing work related activities in the last 12 months, and if they experienced pain in the last 7 days (as reported by the participants in the control group). The results from the pre and post-test scores for the control group revealed the following findings: (1) an increase in reported pain in the neck, shoulder, elbow, wrist/hand, upper back, lower back, knee, and ankle/feet pain that prevented work-related activities and (2) a decrease in reported pain in the Hip/Thigh.
Researcher Developed Questionnaire
Table 3 shows the results of the Researcher Developed Questionnaire regarding how comfortable the participants felt implementing ergonomics, how MSD pain affected activities in the simulation clinic, if previous lectures regarding ergonomics were valuable, how comfortable they were in making adjustments to their workstation and chair, how mindful they were of taking breaks, and how often they implemented stretching at their bench pre and post intervention. The results from the pre and post-test scores for the control group on the Researcher Questionnaire revealed the following findings: the participants in the control group: (1) felt more comfortable implementing ergonomic principles; (2) reported being in an awkward position more of the time; (3) made more frequent adjustments to their work stations to implement proper ergonomic principles; (4) were less mindful of taking breaks; (5) reported that having pictures at their workstation which depicted proper ergonomics helped them be more mindful/facilitated implementing recommended stretches throughout their workday. When asked about their recommendations to help them better implement proper ergonomics throughout their dental school program, suggestions included the following: more stretching throughout the clinic days, consistency with proper ergonomic feedback and implementation, better loupes to allow for proper ergonomics, timer on monitors every 15 minutes to remind students of a break and stretching, and dental faculty feedback on proper ergonomics with the dental students.
Control vs. Intervention Groups
The baseline demographic data that was collected from the pre survey for the control and intervention groups consisted of gender, height (in inches), and weight (in pounds). A comparison of the three demographic characteristics between the control (n = 28) and intervention (n = 51) groups was conducted and no statistically significant differences were found (p-values all > 0.05). Table 4 shows the results of the comparisons in percentages between the control and intervention groups on each of the questions of the M-NMQ. Phi effect sizes were calculated for most of the analyses with effect sizes indicated that were calculated using Cramer’s V formula. The interpretation of Phi and Cramer’s V effect sizes are similar with the effect sizes ranging from 0 to 1. A small effect is about 0.1, a medium effect is about 0.3, and a large effect is about 0.5. A statistically significant relationship was identified between the two groups for shoulder pain in the last 7 days (p-value = 0.009 from Chi-Square test) with shoulder pain decreasing to only 5 participants (9.4%) in the intervention group compared to 7 participants (35.0%) in the control group. The effect size was 0.28 which is a medium effect for the association between group and shoulder pain. In addition, a statistically significant relationship was identified between the two groups for knee pain in the last 7 days (p-value = 0.011 from Chi Square test) with knee pain decreasing to 0 participants (0%) in the intervention group compared to 2 participants (11.8%) in the control group. The effect size was 0.28 which is also a medium effect for the association between group and knee pain. The other questions from the M-NMQ did not indicate any statistically significant relationships between the control vs. intervention groups.
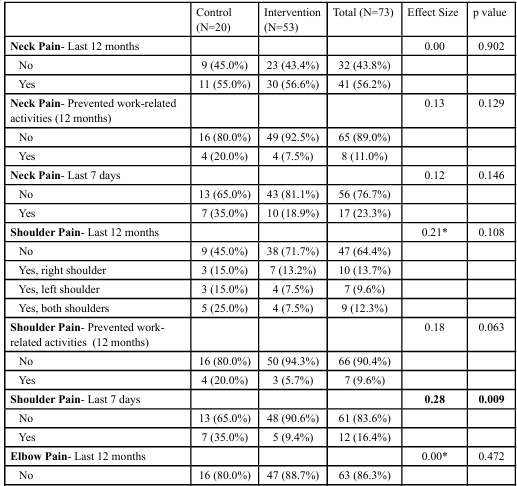
Table 4: Comparison of Percentages of the Modified Nordic Musculoskeletal Questionnaire for Post-Test Between Control vs. Intervention
Discussion
The aim of this study was to examine the effectiveness of a ten week ergonomic intervention program on reduction of self-reported pain and symptoms of MSDs among second-year students enrolled in a Midwest dental program. The results of this study indicated similar findings in terms of the frequency and location of pain among dental students [1,3-4,14-16]. That is, over 50% of the dental students in this study reported neck, shoulder, back, and hand pain in the 12 months preceding this study. Consistent with other studies, the results of this study seem to suggest that interventions which reinforce proper positioning of the body and dental equipment, allowing for a neutral working posture, can help minimize muscular strain and complaints of pain [16,22,23]. Similarly, the findings from this study support the work of other researchers who have provided evidence that the implementation of breaks and stretching exercises that reverse the person’s common positions at work are an instrumental piece of an effective ergonomic intervention [16,22]. Additionally, the outcomes of this study also support the conclusions of other researchers who have asserted that the use of feedback involving photography can help improve the implementation of proper ergonomic principles [7] and help prevent and/or minimize the presence of MSDs among dental students and professionals [24]. Likewise, this study seems to support the current evidence which declares that the use of visual reminders, such as photographs of proper ergonomics and reminders to stretch throughout dental labs and procedures, as well as individualized feedback may be beneficial in adopting appropriate ergonomic postures and principles [25].
More specifically, overall, the results of this study revealed that a 10 week ergonomic intervention program has the potential to improve the application of ergonomic principles, increase the implementation of routine breaks and stretches during dental simulation clinic sessions, and decrease the presence of musculoskeletal pain and dysfunction. For example, in the intervention group there was a decrease in reports of musculoskeletal pain that affected their occupations/activities outside of the simulation clinic, whereas in the control group there was an increase in reports of musculoskeletal pain that affected their occupations/activities outside of the simulation clinic.
Affecting Occupations/Activities in Simulation Clinic
As previously discussed, dental students and professionals are particularly prone to work-related musculoskeletal disorders [6,8,22]. The results of this study support the above premise as over 40% of all the participants in this study initially reported that musculoskeletal pain affected activities/occupations outside of the dental lab. However, after the 10-week intervention program, participants in the intervention group had a decrease in the number of participants who reported musculoskeletal pain which affected activities/occupations outside of the dental lab (26.5% on the pre-test and 7.4% on the post test). In contrast, the control group had an increase in the reporting of musculoskeletal pain that affected activities/occupations outside of the dental lab at the end of this study (14.3% on the pre-test and 35.0% on the post-test). These results are even more substantial when one compares the post-test scores of the intervention group (7.4%) with the control group (35%). Moreover, this seems even more important when one considers that the intervention group had a higher percentage of reported difficulties prior to the intervention (26.6%) in comparison to the control group (14.3%), yet, at the end of the intervention, the intervention group had a lower percentage of participants who reported musculoskeletal pain that affected activities/occupations outside of the dental lab (7.4% versus 35.0%). These results seem to suggest that the interventions provided in this study can decrease reports of musculoskeletal pain which interfere with daily activities and occupations outside the dental simulation clinic.
Visual and Verbal Feedback
Even though both the control and intervention group demonstrated improvement regarding how comfortable they felt implementing ergonomics while working in the simulation clinic; the intervention group had a greater percentage of participants (55.6% versus 45.0%) who indicated that they felt comfortable or extremely comfortable on the post-test. These results may suggest that the review of information related to the importance of the implementation of ergonomic principles and regular stretching which was provided immediately prior to this study, as well as the daily visual reminders (i.e., photos of ergonomic principles and recommended stretches) at all of the participants’ lab stations, was beneficial; however, it might also suggest that the use of individualized verbal and visual feedback (photographs taken when dental students were not implementing proper ergonomic principles and the verbal feedback provided regarding how to improve) may be even more effective. In terms of their reports regarding adjusting their workstations, both the intervention and control group reported making more consistent adjustments by the end of this study. Regarding workstation adjustments, the intervention group demonstrated a significant increase from 40.8% to 57.4% of participants reporting frequent adjustments. Conversely, while the control group also showed an increase, it was more pronounced with a rise from 39.3% to 65% in the control group. Since these findings were similar in both groups, this may suggest that the review of information related to the importance of the implementation of ergonomic principles and regular stretching provided immediately prior to this study and as daily visual reminders (i.e., photos of ergonomic principles and recommended stretches) at all of the participants’ lab stations may be sufficient in effecting ergonomic changes related to the working environment. These findings also support Eyvazlou et al. [23] assertion that effective intervention strategies need to include ergonomically correct workstations and the desperate need for further research on work related MSDs within the dental practice environment.
Benefits of Photo Feedback
Participants in the intervention group reported a significant decrease in time spent in awkward positions compared to the control group. At pre-intervention, 32.6% of the intervention group reported being in awkward positions over 50% of the time, which decreased to 13% at post-intervention. Conversely, the control group's reported time in awkward positions increased from 21% to 25%. This finding seems to suggest that the use of individualized verbal and visual feedback is more effective than lectures and posting of photos regarding proper ergonomic principles. This finding is also consistent with the current evidence concerning the benefits of photographic analysis and improved implementation of ergonomic principles by dental students [6,7]. In fact, the researchers in this study concur with Grabin et al. [24] and believe that the application of photographic analysis in clinical situations not only facilitated self-reflection but ultimately increased clinical compliance. For example, participants in this study often expressed that being able to visually see their own ergonomic deficiencies led to an increase in ownership and motivation to change their posture when working in the dental lab. These tenets were also indicated by the participants’ feedback on the researcher developed post-test survey as approximately half (47.2%) of the participants reported that the individualized photos and feedback were very valuable in terms of being able to better apply ergonomic principles in the dental lab. Similarly, the results from the post-intervention survey also revealed that the interventions provided to intervention group increased the frequency of the implementation of stretching exercises at their bench (i.e., 52.9% of the participants reported stretching 1-2 times/day on the pre-test and 74.1% of them reported stretching 1-2 times/day on the post-test).
Musculoskeletal (MSD) Pain
According to researchers [1,14-16] the most common areas for pain among dentists, dental students, and other dental professionals are the neck, shoulders, back, and hands. The results of this study revealed that a 10-week intervention has the potential to decrease reports of musculoskeletal pain. For example, after 10 weeks of intervention, there was a decrease of participants in the intervention group that reported having aches, pain, discomfort, and numbness in their neck during the last 12 months (62.7% versus 57.4%). Whereas, in the control group, there was an increase in participants that reported having ache, pain, discomfort, numbness in their neck during the last 12 months (53.6% versus 55%). When participants were asked about having trouble (ache, pain, discomfort, and numbness) in their shoulders, the intervention group showed a decrease (41.2% versus 28.2%) in the percentage of participants that reported trouble, however in the control group, there was an increase (50% versus 55%) in participants that reported trouble in their shoulders. Regarding having ache, pain, discomfort in the wrists/hands and upper back during the last 12 months, there was a decrease in participants that reported having ache, pain discomfort, numbness in their wrists/hands and upper back in the intervention group and in the control group. However, when asked about having trouble (ache, pain, numbness) in their lower back, there was a decrease (60.8% versus 41.5%) in the percentage of participants in the intervention group that reported having trouble in the lower back, whereas there was no change in the control group. Again, these findings seem to suggest that the individualized visual and verbal feedback may be an effective strategy to decrease musculoskeletal pain in dental students.
Limitations and Recommendations for Future Research
One limitation of this study is the relatively small sample size which may limit the ability to generalize the results. Therefore, the results of this study can only be generalized to the sample of students, but we hope that this study assists in informing future studies related to this topic. Another limitation of this study relates to the fact that the only criterion for inclusion is that participants were second-year dental students, which could have limited the findings. Unfortunately, this inclusion criterion also did not account for any other factors that may affect the outcomes (e.g., previous musculoskeletal disorders, existing ergonomic knowledge, or baseline pain levels). Thus, future studies may want to include more longitudinal data collection and interventions and account for the above-mentioned factors that could potentially affect outcomes. Additionally, one needs to consider that, even though the Researcher Developed Questionnaire was informed by the literature and expert opinion, it is lacking established reliability and validity which could impact the credibility of the findings. Also, another limitation of this study is that there was an unequal number of survey responses for the control and intervention groups which could have impacted the findings. The researchers randomly selected control versus intervention groups by their assigned laboratory workstation number (i.e., 1-70; 71-140). Since these students’ workstation assignments were geographically together, it is possible that this randomization process influenced the response rates and/ or results. Thus, future studies may want to consider assigning randomness differently (e.g., all even and odd number workstations, pulling numbers out of a hat, etc.). A limitation of the study in regard to data analysis was that the pre and post-survey data was not able to be linked which weakened the statistical approach of using paired data for analysis. Additionally, another factor that could have influenced the results is that the post-intervention survey was completed during the last week of the quarter, a week in which the participants in this study were taking practicums and reported high stress related to final exams, etc. Thus, the timing of the post-tests could have limited the number of participants willing to complete the post-test surveys or could have resulted in higher stress-related MSD pain. Therefore, future studies should consider the students’ coursework load when setting schedules to collect post-test data and attempt to avoid periods of high stress (e.g., final exams and weeks of lab practicums). Furthermore, one needs to consider that potential confounding factors, such as participants' physical fitness, stress levels, and/or lifestyle factors (e.g., sleep quality, physical activity, etc.) were not measured and could have influenced the outcomes of this study. Thus, future studies may want to include these factors in their data collection measures. Lastly, since many of the participants in this study reported that they corrected their posture and/or adjusted their workstation at the mere presence of the researcher walking by their workstation, it is possible that this “presence” increased the ergonomic awareness among the participants. Yet, as this occurred in both groups, this did not likely influence the difference between the intervention group and the control group.
Conclusion
The results of this study support the current evidence and appears to suggest that a 10-week ergonomic intervention program, which includes visual reminders to stretch and implement proper ergonomics, photography, and one on one individualized feedback, has the potential to improve the application of ergonomic principles, increase the implementation of routine breaks and stretches during dental laboratory classes, and decrease the presence of musculoskeletal pain. However, one needs to consider the limitations of this study. These findings also seem to support the critical role of education in preventing occupational health hazards among future dental professionals. By integrating ergonomic principles into dental curricula, educators can equip students with the knowledge and skills necessary to protect their long-term well-being while enhancing their academic performance. Furthermore, the implementation of routine breaks and stretches within the dental laboratory setting can serve as a model for promoting healthy lifestyle behaviors among students. This study highlights the need for a multidisciplinary approach, involving occupational therapy and dental education, to cultivate a culture of health and workplace wellness within the dental programs.
Competing Interests:
The authors of this research declare no competing interest regarding this study.
References
Singh, V., Nettem, S., Soe, H., Babji, N., Sahari, A., Yusof, L., et al. (2022). Perception of risk factors at work associated with musculoskeletal symptoms in dental students of Meleka, Malaysia: A cross-sectional study. Work. 73(3):969-976. View
Al-Emara, Z., Karaharju-Suvanto, T., Furu, P., & Furu, H., (2024). Musculoskeletal disorders and work ability among dentists and dental students in Finland. Work. 78(1):73-81. View
Aghahi, R. H., Darabi, R., & Hashemipour, M. A., (2018). Neck, back, and shoulder pains and ergonomic factors among dental students. Journal of education and health promotion, 7, 40. View
Santucci, N., Jellin, J., & Davenport, T., (2020). Dental and physical therapy faculty collaborate in assessing and educating dental students on musculoskeletal disorders. J Dent Educ. 85(1):53-59. View
Cleveland Clinic. Musculoskeletal Pain [Internet]. 2024 [cited 2024 Aug 22]. View
Partido, B. B., Wright, B. M., (2018). Self-assessment of ergonomics amongst dental students utilising photography: RCT. Eur J Dent Educ. 22(4):223–33. View
Partido, B. B., (2020). Longitudinal effects of utilising photography on the accuracy of ergonomic self-assessments amongst dental hygiene students. Eur J Dent Educ. 24(1):63–70. View
Zhou, Y., Zhou, W., Aisaiti, A., Wang, B., Zhang, J., Svensson, P., et al. (2021). Dentists have a high occupational risk of neck disorders with impact on somatosensory function and neck mobility. J Occup Heal. 63(1):e12269. View
Das, H., Motghare, V., Singh, M., (2018). Ergonomics in Dentistry. Int J Appl Dent Sci. 4(4):104–10. View
Soo, S., And, W., Chong, C., Tew, I., & Yahya, N., (2023). Occupational ergonomics and related musculoskeletal disorders among dentists : A systematic review. Work. 74(2) :469-476. View
Karibasappa, G. N., Sujatha, A., Rajeshwari, K., (2014). Department of Public Health Dentistry, ACPM Dental College, Dhule 424001, Maharashtra, India. Dentists’ Knowledge, Attitude and Behavior towards the Dental Ergonomics. IOSR J Dent Méd Sci. 13(5):86–9. View
Roll, S. C., Tung, K. D., Chang, H., Sehremelis, T. A., Fukumura, Y. E., Randolph, S., et al. (2019). Prevention and rehabilitation of musculoskeletal disorders in oral health care professionals A systematic review. J Am Dent Assoc. 150(6):489–502. View
Faust, A. M., Ahmed, S. N., Johnston, L. B., Harmon, J. B., (2021). Teaching methodologies for improving dental students’ implementation of ergonomic operator and patient positioning. J Dent Educ. 85(3):370–8. View
Huppert, F., Betz, W., Maurer-Grubinger, C., Holzgreve, F., Fraeulin, L., Filmann, N., et al. (2021). Influence of design of dentist’s chairs on body posture for dentists with different working experience. BMC Musculoskelet Disord. 22(1):462. View
Netanely, S., Luria, S., & Langer, D., (2020). Musculoskeletal disorders among dental hygienist and students of dental hygiene. Int J Dent Hyg. 18(2):210–6. View
Mane, V., & Rajhans, N., (2024). Assessment of ergonomic risk of work related musculoskeletal disorders among dentists in Kolhapur región. Work. 79(4):2087-2101. View
Garcia, P. P. N. S., Gottardello, A. C. A., Wajngarten, D., Presoto, C. D., Campos, J. A. D. B., (2017). Ergonomics in dentistry: experiences of the practice by dental students. Eur J Dent Educ. 21(3):175-179. View
Kamal, A., Ahmed, D., Habib, S., Al-Mohareb, R., (2020). Ergonomics of preclinical dental students and potential musculoskeletal disorders. J Dent Educ. 84(12):1438-1446. View
Lietz, J., Ulusoy, N., Nienhaus, A., (2020). Prevention of Musculoskeletal Diseases and Pain among Dental Professionals through Ergonomic Interventions: A Systematic Literature Review. Int J Environ Res Public Health. 17(10):3482. Published 2020 May 16. View
Danylak, S., Walsh, L., & Zafar, S., (2023). Measuring ergonomic interventions and prevention programs for reducing musculoskeletal injury risk in the dental workforce: A systematic review. J Dent Educ. 88(1):128-141. View
Sabbagh, h., Shagagi, A., Basheer, H., Mahmoud, R., & Arafah, A., (2023). Effect of ergonomics awareness in controlling work related musculoskeletal-pain among dental students: A cross sectional study. Work. 76(3):1125-1133. View
Khalekar, Y., Zope, A., Chaudhari, L., Brahmankar, U., Gadge, H., Deore, S., (2016). Prevention is better than cure. Journal of Applied Dental and Medical Sciences. 2(1).
Eyvazlou, M., Asghari, A., Mokarami, H., Hosseinabadi, M. B., Jazari, M. D., Gharibi, V., (2021). Musculoskeletal disorders and selecting an appropriate tool for ergonomic risk assessment in the dental profession. Work (Read, Mass). 68(4):1239–48. View
Garbin, A. J. Í., Garbin, C. A. S., Diniz, D. G., Yarid, S. D., (2011). Dental students’ knowledge of ergonomic postural requirements and their application during clinical care: Ergonomic postural requirements. Eur J Dent Educ. 15(1):31–5. View
Sangalli, L., Alabsy, M., Lingle, D., Alessandri-Bonetti, A., & Mitchell, J., (2023). Assessment of dental ergonomics among dental students: A retrospective study. J Dent Educ. 87(11):1559 1569. View
American Occupational Therapy Association (AOTA). Occupational Therapy’s Role in Ergonomics [Internet]. 2017. [cited 2023 Aug 13]. Available from: https://www.aota.org/~/ media/Corporate/Files/AboutOT/Professionals/WhatIsOT/WI/ Facts/ergonomics.pdf View
Aboalshamat, K. T., (2020). Nordic Assessment of Occupational Disorders among Dental Students and Dentists in Saudi Arabia. J Int Soc Prev Community Dent.10(5):561–8. View
Braun, V., Clarke, V., (2006). Using thematic analysis in psychology. Qual Res Psychol. 3(2):77–101. View
Clarke, V., Braun, V., (2018). Using thematic analysis in counselling and psychotherapy research: A critical reflection. Couns Psychother Res. 18(2):107–10. View
Ozuem, N., Howell, K., & Ranfagni, S., (2023). A Step-by-Step Process of Thematic Analysis to Develop a Conceptual Model in Qualitative Research. Int J Qual Methods, 22. View