Journal of Rehabilitation Practices and Research Volume 7 (2026), Article ID: JRPR-193
https://doi.org/10.33790/jrpr1100193Case Report
Adaptive Wakeboarding: A Case Report on Equipment Modifications and Strength Training for Improved Performance
Edwin J. Myers*, OTD, OTR/L, ATP and Kimberly Balbino, MS, OTR/L
Department of Rehabilitation Sciences, Marieb Colleg of Health & Human Services, Florida Gulf Coast University, United States.
Corresponding Author Details: Edwin J. Myers, OTD, OTR/L, ATP, Associate Professor, Department of Rehabilitation Sciences, Marieb Colleg of Health & Human Services, Florida Gulf Coast University, 10501 FGCU Blvd S. Fort Myers, FL, 33965, United States.
Received date: 11th October, 2025
Accepted date: 26th December, 2025
Published date: 01st January, 2026
Citation: Myers, E. J., & Balbino, K., (2026). Adaptive Wakeboarding: A Case Report on Equipment Modifications and Strength Training for Improved Performance. J Rehab Pract Res, 7(1):193.
Copyright: ©2026, This is an open-access article distributed under the terms of the Creative Commons Attribution License 4.0, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Individuals with disabilities often face internal and environmental barriers that limit participation in adaptive sports. In many cases, the necessary equipment is unavailable, requiring individuals to create their own modifications, an approach that can be time-consuming and pose safety risks. This case report addresses a gap in the literature concerning the specific needs of individuals with neurological conditions in adaptive sports. This case study employed a multimodal intervention to modify an adaptive wakeboard and enhance functional performance for a participant with spastic hemiparesis cerebral palsy. The participant, limited to functional use of her left upper extremity, experienced severe pain and fatigue during wakeboarding, which negatively impacted her posture, performance, and quality of life. Following equipment modifications and a twelve-week strength training program, the participant demonstrated augmented performance, a 605% increase in ride time, and greater participation in the sport, alongside a marked improvement in quality of life. The participant’s motivation and success may have been lower if the adaptive sport did not align with her interests, highlighting the importance of self-direction and autonomy.
Keywords: Adaptive Sports, Wakeboarding, Cerebral Palsy, Assistive Technology, Quality of Life, Functional Training
Introduction
Participation in recreational activities offers a range of benefits, including heightened self-confidence, expanded social opportunities, improved management of physical conditions, and a higher overall quality of life [1,2]. To support individuals with disabilities, modifications are often made to equipment, rules, or environments, collectively referred to as adaptive sports and recreation [2]. A wide variety of sports, including basketball, rowing, swimming, soccer, sailing, skiing, snowboarding, and wakeboarding, have been modified to promote inclusive participation [3]. Despite these efforts, individuals with disabilities continue to face multilevel barriers that limit their ability to meet physical activity guidelines and engage in recreational activities compared to those without disabilities [4,5]. Internal barriers include a person having trouble accepting their disability or managing physical symptoms. Financial barriers involve high costs and limited availability of adaptive equipment [4,6]. Barriers may also refer to inaccessible facilities, equipment not yet being developed, and limited studies regarding the efficacy of equipment [7]. While adaptive sports have expanded in scope, individuals with neurological conditions remain underrepresented in both participation and research, leaving a critical gap in understanding how to support their unique needs.
The type of adaptive equipment required varies based on both the sport and the individual’s physical impairments [8]. For individuals with lower extremity limitations, such as those with limb amputations, spinal cord injuries, or cerebral palsy, seated adaptations are often necessary to enable participation. Sports like sit-skiing and sit-kiting have gained popularity as they offer tailored solutions to mobility challenges [8,9]. However, access to appropriate equipment is frequently hindered by financial constraints or limited availability. In such cases, individuals may resort to repurposing gear designed for other sports, which can compromise safety, reduce performance, and place undue physical strain on the body [9].
Physical activity is widely recognized for its role in promoting health, supporting community reintegration, and enhancing overall well- being [4]. For individuals with disabilities, it also serves as a critical tool for managing secondary conditions and preventing functional decline [10]. The modifications required to enable participation in adaptive sports vary based on the nature of the disability and the specific demands of the sport. Neurological conditions such as cerebral palsy often necessitate unique modifications to ensure safety and success. Yet, the literature offers limited insight into the adaptive sport needs of individuals with these conditions, which hinders the development of effective support strategies [11].
This case report examines the experience of an individual with spastic hemiparesis due to cerebral palsy who faced significant barriers to participating in adaptive wakeboarding. Wakeboarding is both a competitive and recreational sport in which participants ride a wakeboard while holding a tow rope, propelled across the water by an electrically powered overhead cable. To accommodate individuals with impaired standing balance, adaptive wakeboarding incorporates a seated aluminum frame, referred to as a cage, mounted on the board [12]. Depending on the participant’s core strength and support needs, the seat may include a backrest, and foot straps are used to secure the lower extremities during motion. Successful participation requires sufficient bilateral upper body strength to maintain grip and posture while navigating the course. This single case study explores how targeted equipment modifications and strength and conditioning interventions can enhance performance and participation for individuals with hemiplegia. Furthermore, it is critical to promote participation in recreational activities of choice, as this impacts motivation and supports self-directedness. Insights from this case may inform future approaches to equipment design, strength and conditioning training, and accessibility in adaptive sports for individuals with neuromotor impairments.
Client Profile
The participant is a 30-year-old female with cerebral palsy and spastic hemiplegia, referred to the Department of Rehabilitation Sciences by the University Office of Adaptive Services due to significant pain and fatigue in her left upper extremity while attempting adaptive wakeboarding. Cerebral palsy is a group of neurological disorders affecting movement and posture, often resulting from early brain injury. Spastic hemiplegia involves motor impairment on one side of the body [13]. In her case, the right side is severely limited due to uncontrolled tone and is nonfunctional for daily activities. She expressed interest in wakeboarding but was not able to participate to her full potential. Her inability to grip the tow rope with both hands placed excessive strain on her left shoulder. She was unable to tolerate more than a few minutes of activity before experiencing pain and fatigue, which persisted for several days post-session. This led to frustration and a reduction in both her quality of life and social participation, as reported by the participant. Informed consent was obtained from the participant prior to the evaluation.
Initial Presentation
During the initial evaluation, the participant presented with a full range of motion (ROM) in the left upper and lower extremities. The right lower extremity exhibited increased tone and limited ROM, though she was able to ambulate independently with an ataxic gait pattern. Her right upper extremity demonstrated severe spastic hemiplegia and was nonfunctional for the purpose of this activity, although she could reduce tone with focused effort. The participant also displayed diminished core strength and postural control, with a tendency to lean to the right. While she could achieve an upright seated posture, she was unable to tolerate balance challenges without support, necessitating the use of a backrest when positioned in the wakeboarding cage.
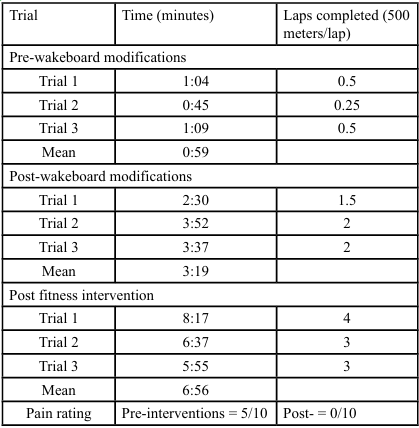
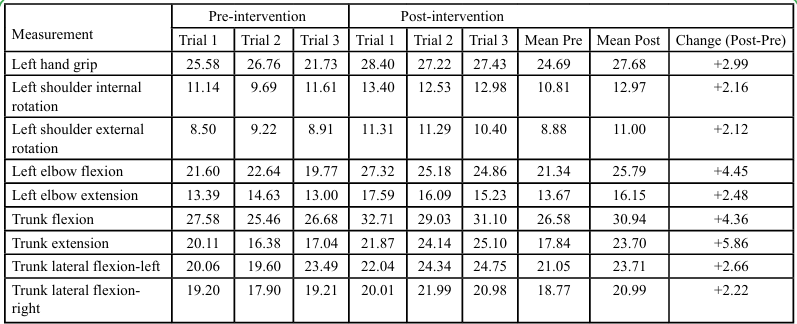
Strength measurements were obtained using the BTE Primus RS, which allowed for simulation of functional movement patterns relevant to wakeboarding. The BTE Primus RS is a computerized rehabilitation and performance system designed to assess and train strength, endurance, and functional movement patterns. It allows for precise measurement of performance output across multiple planes, making it particularly useful for simulating sport-specific tasks and tracking progress over time [14]. Pre- and post-intervention performance data were collected using the Primus at each stage of the intervention (Table 1). At the time of the initial evaluation, the participant reported no pain. However, during the initial wakeboard trials, she experienced left upper extremity pain rated at 5/10 by the end of the third trial.
Assistive Technology Intervention
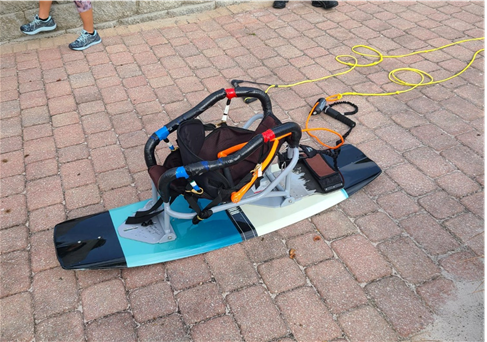
Following approval from the university’s Institutional Review Board, targeted modifications were made to the participant’s adaptive wakeboard to address her specific functional needs. Modifications were guided by user-centered design principles to ensure the equipment addressed the participant’s unique functioning and safety requirements [15]. Given her diminished core strength, the back support was adjusted to provide enhanced trunk stability. The original wakeboard design (Figure 1) was modified to attach a spreader bar (Figure 2) to the forward vertical supports, allowing the seat to distribute the effort required to control the tow rope. However, the spreader bar is a standardized attachment mechanism that normally fits under the seat and behind the vertical supports. The normal positioning of the spreader bar was unfeasible for the participant to use due to her hemiplegia. Therefore, the design was revised to develop a camp that fits both the forward vertical bars on the wakeboard seat and the spreader bar. Brackets were designed in SolidWorks and printed on a Ultimaker 5S 3D printer in high- performance polylactic acid (PLA+) and are fixed using 5M machine screws that are threaded into the rearmost component of the clamps (Figure 3). The screws on the camps only need to be tightened enough to prevent vertical movement of the spreader bar during operation. This modification allowed customization of the angle of control for the participant, reducing strain on her left shoulder. To promote safety, a quick-release mechanism was added, and the participant instructed to wear a specialized glove to support grip and reduce fatigue. Figure 4 shows the fully assembled wakeboard on day of initial trial.
To evaluate safety, the system was first mocked up in a controlled laboratory setting using the BTE Primus RS to simulate towing conditions. A weighted load was placed in the adapted wakeboard to replicate the participant’s presence, and the safety features were tested repeatedly under her direct observation. This process ensured both mechanical reliability and psychological reassurance prior to field implementation. Before formal trials began, the participant completed an orientation session to familiarize herself with the modified equipment, including safety protocols and handling techniques, ensuring confidence and preparedness.
Due to limited availability of adaptive equipment, an international search was conducted to source the necessary components. Multiple vendors noted that the market for such specialized gear is small, making access both difficult and costly. These barriers underscore the broader challenges faced by individuals with complex physical needs in adaptive sports.
Prior to equipment modification, the participant averaged a run time of 59 seconds and was unable to complete a full lap in three consecutive trials (Table 1). After the modifications, her run time increased to 3 minutes and 20 seconds, with an average of 1.8 laps per run, demonstrating greater endurance and control (Figure 5 and 6). While these gains were significant, further progress was anticipated through targeted strength and conditioning training. Improving physical function could address underlying strength and postural limitations.

Figure 6: Participant Utilizing the Adaptive Wakeboard System Showing Quick Release Mechanism Attached to Spreader Bar
Targeted Fitness Intervention
The 12 week home exercise program consisted of three sessions per week, each lasting approximately 30–45 minutes. Exercises targeted core stability, trunk control, and left upper extremity endurance, using resistance bands, light free weights, and body weight activities such as seated balance drills. Progression was achieved by gradually increasing resistance and repetitions as tolerated. In addition, the participant attended 17 group fitness sessions at an inclusive recreation center, which provided circuit style training adapted for individuals with disabilities. These sessions were supervised by trained staff and emphasized aerobic conditioning, functional strength, and peer support. There were no costs associated with participation. The individual program was supervised directly by the principal investigator and research team, and the inclusive recreation center is a non profit agency that did not charge for the sessions. To support adherence, the participant engaged in weekly telehealth consultations with the research team, maintained exercise logs, and received ongoing encouragement. Based on her exercise logs, the participant completed 100% of the prescribed home sessions, performing at least three sessions per week for all twelve weeks in addition to the 17 supervised group fitness sessions. Progression of the home program was not standardized; exercises were modified subjectively in response to her performance, fatigue levels, and observed movement quality. During each weekly telehealth check in, the research team reviewed her logs, directly observed her completing selected exercises to verify accuracy, and adjusted resistance, repetitions, or technique as needed to ensure appropriate challenge and safety. This structured yet accessible program ensured safety while promoting measurable gains in strength and endurance.
Over the course of the intervention, she completed all twelve weeks of the home program and attended 17 group sessions. She attended 100% of the group sessions which consisted of a standardized exercise program tailored to address individual strength and conditioning needs. Post intervention assessments revealed marked gains in left upper extremity strength, core balance, and overall endurance (Table 2). Her run time increased to 6 minutes and 56 seconds, with an average of 3.33 laps per session. Notably, she reported 0/10 pain following wakeboarding and expressed enthusiasm about her ability to participate fully in the sport.
Data Analysis
Pre- and post-intervention performance data were analyzed descriptively. For each measure, mean values across three trials were calculated to illustrate central tendency, and change scores were reported to highlight differences between pre- and post-intervention phases. Given the single case design, inferential statistics were not applied, as these require larger sample sizes. Instead, descriptive statistics and direct comparison of pre- and postintervention values were used to demonstrate clinically meaningful changes in performance.
Results
Following equipment modifications and completion of the 12 week fitness intervention, the participant demonstrated clear improvements in wakeboard performance. Wakeboarding run times increased from a mean of 59 seconds pre intervention to 416 seconds (6 minutes, 56 seconds) post intervention, representing a 605% improvement. The participant progressed from being unable to complete a full lap to averaging 3.33 laps per run, indicating a substantial change in functional capacity.
Strength and trunk control measures also showed consistent gains (Table 2). For example, left-hand grip strength increased by nearly 3 kg, left elbow flexion improved by more than 4 kg, and trunk extension increased by almost 6 kg. These changes reflect enhanced upper extremity endurance and core stability, both of which are critical for sustained wakeboarding performance. Pain ratings decreased from 5/10 during initial trials to 0/10 post intervention, and the participant reported enthusiasm and satisfaction with her ability to engage in the sport without discomfort.
Overall, descriptive data highlight clinically meaningful improvements in endurance, strength, and quality of life. The participant’s ability to sustain longer rides, complete multiple laps, and eliminate pain during activity underscores the effectiveness of combining equipment modifications with targeted fitness training in adaptive sport participation.
Discussion
The participant’s performance gains reflect more than physical advancement; they demonstrate the impact of a multimodal, individualized approach to adaptive sport participation. By combining equipment modifications with targeted strength and conditioning, the intervention addressed both mechanical barriers and underlying physical limitations. The elimination of pain and a notable increase in endurance enabled sustained engagement in wakeboarding and supported broader participation in daily activities. These outcomes indicate the therapeutic potential of adaptive sports to encourage autonomy, confidence, and community integration [4].
Despite these outcomes, the case highlights the persistence of systemic barriers. Sourcing appropriate components required international outreach, 3D printing, and tailored modifications. These barriers underscore the lack of scalable, commercially available solutions for individuals with complex physical needs [6]. Addressing these gaps will require coordinated efforts among clinicians, engineers, manufacturers, and policymakers to expand access and affordability of adaptive equipment.
Moreover, the participant’s experience also illustrates the importance of interdisciplinary collaboration and user-centered design. Her involvement in the design and testing process not only ensured safety and functionality but also enhanced psychological readiness and trust in the system. Although she experienced fatigue following wakeboarding, it remained within expected limits and did not interfere with other meaningful activities. This shift, from activity- limiting fatigue to manageable exertion, marked a turning point in her functional capacity and quality of life.
This case also underscores the importance of integrating strength and conditioning training with equipment modifications. While modifications alone yielded initial gains, the fitness intervention was essential for achieving sustained performance improvements. Future research should investigate scalable models for integrating assistive technology with personalized physical training to facilitate participation in adaptive sports.
Conclusion
Individuals with disabilities remain significantly underrepresented in recreational sports, often due to barriers in equipment access, cost, and awareness. While the literature identifies these challenges, this case underscores the urgent need for action. The participant’s experience illustrates how tailored interventions, combining assistive technology with strength and conditioning training, can transform not only performance but also quality of life. However, accessing the appropriate equipment remains time-consuming and costly, and many individuals are left to navigate this process on their own. These barriers perpetuate health disparities and limit opportunities for social engagement and community integration.
Adaptive sports offer more than physical benefits, they promote autonomy, emotional well-being, and social inclusion. For individuals with neuromotor impairments, preventative approaches are essential for reducing secondary conditions and supporting long-term participation. This case highlights the importance of considering both physical and psychosocial factors when designing interventions. To foster equitable access, collaboration among healthcare professionals, engineers, policymakers, and community organizations is essential. Expanding the availability and affordability of adaptive equipment is a critical step toward empowering individuals with disabilities to lead active, engaged lives.
Limitations
While this case report demonstrated meaningful progress in performance and participation, certain limitations should be acknowledged. The intervention combined equipment modifications with a fitness program, making it difficult to isolate the effects of each component. Removing the equipment modifications to test the fitness intervention independently was deemed clinically inappropriate, as it would have returned the participant to a baseline level of function that precluded safe participation.
Additionally, geographic constraints limited in-person monitoring of the home exercise program. Weekly telehealth consultations were implemented to support adherence, though remote supervision may have introduced variability in execution. Future studies may benefit from replicating this research with a larger cohort, frequent data collection and phased intervention designs to better understand the relative contributions of assistive technology and physical training.
Acknowledgment:
We would like to thank Danielle Iqbal, MS, OTR/L for her valued assistance with research design and data collection.
Competing Interests:
The Authors have no competing interests to disclose.
References
Lastuka, A., & Cottingham, M. (2016). The effect of adaptive sports on employment among people with disabilities. Disability and Rehabilitation, 38(8), 742–748. View
Mavritsakis, O., Treschow, M., Labbé, D., Bethune, A., & Miller, W. C. (2021). Up on the hill: The experiences of adaptive snow sports. Disability and Rehabilitation, 43(15), 2219–2226. View
Mannella, S., Labbé, D., Bundon, A., Sauve, J. McBride, C. B., Best, K., Yung, O., & Miller, W. C. (2023). Access at elevation: Strategies used to support participation for people with disabilities in adaptive snowsports. Journal of Outdoor Recreation and Tourism, 43, 100685. View
Diaz, R., Miller, E. K., Kraus, E., & Fredericson, M. (2019). Impact of adaptive sports participation on quality of life. Sports Medicine and Arthroscopy Review, 27(2), 73–82. View
Wekesser, M., Costa, G. H., Pasik, P. J., & Erickson, K. (2023). "It shaped my future in ways I wasn't prepared for -in the best way possible": Alumni volunteers' experiences in an adapted sports and recreation program. Adapted Physical Activity Quarterly, 40(2), 303–322. View
McLoughlin, G., Weisman Fecske, C., Castaneda, Y., Gwin, C., & Graber, K. (2017). Sport participation for elite athletes with physical disabilities: Motivations, barriers, and facilitators. Adapted Physical Activity Quarterly, 34(4), 421–441. View
Duvall, J., Satpute, S., Cooper, R., & Cooper, R. A. (2021). A review of adaptive sport opportunities for power wheelchair users. Disability and Rehabilitation. Assistive Technology, 16(4), 407–413. View
Oh, H., Johnson, W., & Syrop, I. P. (2019). Winter adaptive sports participation, injuries, and equipment. Sports Medicine and Arthroscopy Review, 27(2), 56–59. View
Loy, D. P., Autry, C. E., Piacenza, J., & Piacenza, N. (2022). Blowing in the wind... exploring windsports as the next generation of adaptive sports and recreation (Part I: Kiting and gliding). Palaestra, 36(3), 7-14. View
Gaskin, C. J., & Morris, T. (2008). Physical activity, health related quality of life, and psychosocial functioning of adults with cerebral palsy. Journal of Physical Activity & Health, 5(1), 146–157. View
Mulligan, H. F., Hale, L. A., Whitehead, L., & Baxter, G. D. (2012). Barriers to physical activity for people with long-term neurological conditions: A review study. Adapted Physical Activity Quarterly, 29(3), 243–265. View
Adaptive Sports Fund. (n.d.). Adaptive wakeboarding. View
Papavasiliou, A., & Hagberg, G. (2021). Editorial: Cerebral palsy: New approaches to understanding its nature and treatment. Frontiers in Neurology, 12, 720937. View
BTE (2024). Primus RS. Retrieved October 1, 2024. View
Ortiz-Escobar, L. M., Chavarria, M. A., Schönenberger, K., Hurst, S., Stein, M. A., Mugeere, A., & Rivas Velarde, M. (2023). Assessing the implementation of user-centered design standards on assistive technology for persons with visual impairments: A systematic review. Frontiers in Rehabilitation Sciences, 4, Article 1238158. View